Trimester-Specific Medication Risk Calculator
Check Medication Safety by Gestational Age
Enter the medication name and gestational age (from fertilization) to see trimester-specific risks and safer alternatives.
When you're pregnant, taking any medication isn't just about how it helps you-it's about how it might affect your baby. The truth is, not all medications are risky at every stage of pregnancy. What’s dangerous in the first trimester might be harmless in the second, and what’s safe early on could become risky later. Understanding trimester-specific medication risks isn’t about avoiding all drugs-it’s about timing them right.
Why Timing Matters More Than You Think
The first 12 weeks of pregnancy, known as the first trimester, are when your baby’s organs form. This is called embryogenesis. During weeks 3 to 8 after fertilization, your baby’s heart, brain, limbs, and face are all taking shape. That’s why exposure to certain medications during this window can cause structural birth defects. After week 8, the risk of major malformations drops sharply-but other risks emerge. Before day 20 after fertilization, most medications follow an “all-or-nothing” rule. If the embryo is damaged, it usually doesn’t survive, and you’ll miscarry. If it survives, it’s likely unharmed. That’s why some women panic after taking a cold pill before they knew they were pregnant-but in most cases, there’s no cause for alarm. After week 8, the baby is no longer forming organs. Instead, they’re growing and maturing. That’s when medications can affect how organs function-not how they’re built. For example, taking certain antidepressants late in pregnancy might lead to breathing issues or jitteriness in the newborn, but not a heart defect.First Trimester: The Most Sensitive Window
The first trimester is where the biggest fears live. And for good reason. Some medications have well-documented, severe risks during this time. Isotretinoin (Accutane), used for severe acne, is one of the most dangerous. If taken between days 21 and 55 after fertilization, it raises the risk of serious brain, heart, and facial defects by 50 times compared to the baseline. That’s why the FDA requires the iPLEDGE program-two negative pregnancy tests before starting, monthly tests during treatment, and one month of contraception after stopping. Since the program started, pregnancy rates among users dropped from nearly 5 per 100 women per year to less than 1. Another example is paroxetine (Paxil), an SSRI antidepressant. If taken between days 20 and 24 after fertilization, it increases the risk of heart defects from about 1% to 2-3%. That’s not a huge jump in absolute terms, but it’s enough to make doctors recommend switching to sertraline (Zoloft), which shows no increased risk in the first trimester based on studies of over 850,000 pregnancies. Even common drugs like ondansetron (Zofran), used for morning sickness, carry a small but real risk. A study of 1.8 million pregnancies found a 32% higher chance of heart defects when taken in the first trimester. But if you wait until after week 10, that risk disappears.Second Trimester: Shifting Risks, Fewer Structural Threats
By the second trimester, your baby’s structure is mostly set. That means the big fear-birth defects-is much lower. But new concerns appear. This is when many women start taking blood pressure meds. ACE inhibitors like lisinopril or enalapril are fine before week 8-but after that, they can cause serious problems: low amniotic fluid, kidney damage, and even skull deformities in the baby. The risk climbs to 30-40% if taken between weeks 12 and 20. The fix? Switch to labetalol or methyldopa, both of which are safe throughout pregnancy with no increased risk of major malformations. Antibiotics like tetracycline can stain developing teeth and affect bone growth if taken after week 15. So even if you need an antibiotic, your doctor will pick one that’s safe in the second trimester, like amoxicillin or cephalexin. And while SSRIs like sertraline are considered low-risk for birth defects in the first trimester, they can still cause neonatal adaptation syndrome if taken into the second half of pregnancy. Symptoms like jitteriness, poor feeding, or fast breathing usually resolve within days after birth-but they’re still stressful for new parents.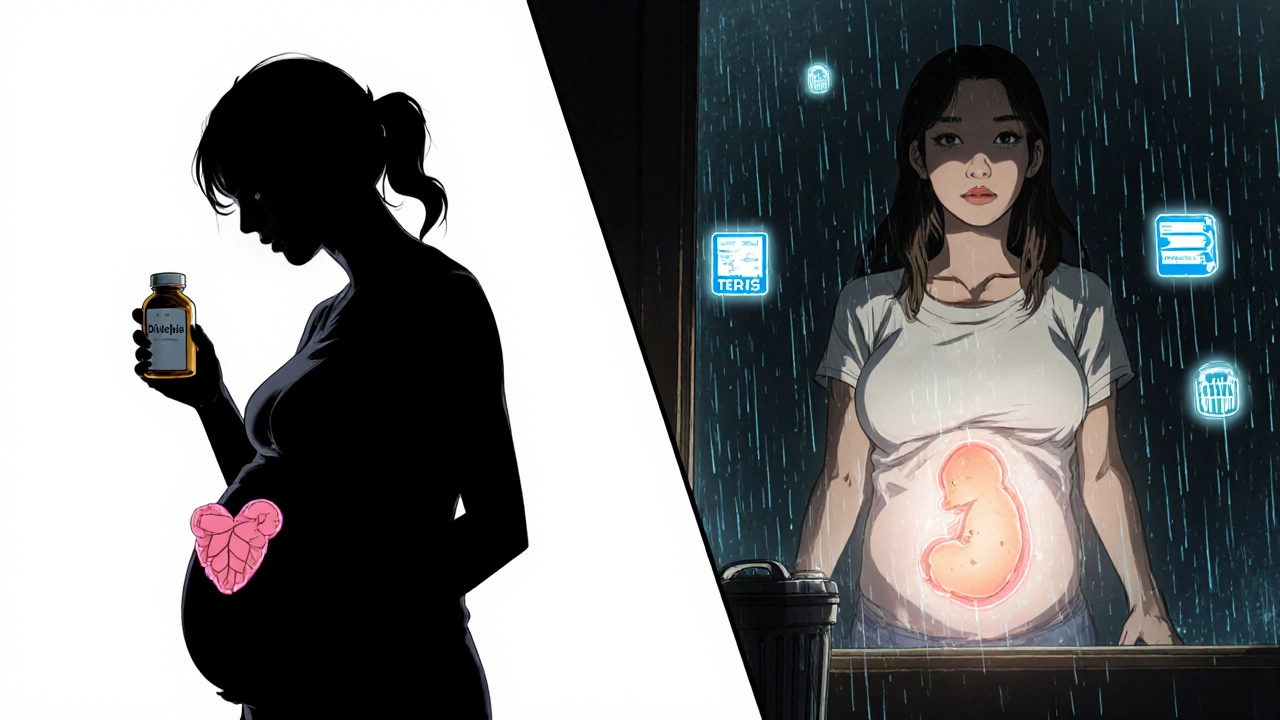
Third Trimester: The Functional Risks
The third trimester is all about growth and preparation for life outside the womb. Medications here don’t change your baby’s shape-they change how their body works after birth. NSAIDs like ibuprofen or naproxen are safe before week 20. But after week 20, they can reduce amniotic fluid levels by 10-15%. After week 32, they can cause the ductus arteriosus-a vital blood vessel in the fetal heart-to close too early. This can lead to serious heart problems in the newborn. SSRIs taken in the third trimester carry a 20-30% risk of neonatal withdrawal symptoms. Paroxetine is the worst offender here. Sertraline is better, but even it can cause fussiness, tremors, or feeding trouble in newborns. That’s why many doctors recommend slowly reducing the dose starting at 34 weeks-cutting by 25% every two weeks-under psychiatric supervision. One mom on Reddit shared how she lowered her sertraline dose from 100mg to 50mg over six weeks before delivery and avoided the withdrawal symptoms her first child had. Opioids and benzodiazepines taken late in pregnancy can cause neonatal abstinence syndrome (NAS)-a condition where the baby is born addicted and goes through withdrawal. Symptoms include screaming, seizures, and trouble eating. These drugs should be avoided if possible, and if used, tapered under medical supervision.What’s Actually Safe?
Not everything is risky. Some medications have been studied across hundreds of thousands of pregnancies and show no clear danger at any stage. Acetaminophen (Tylenol) remains the go-to pain reliever during pregnancy. Over 24 studies involving more than 215,000 pregnancies found no link to neurodevelopmental problems at standard doses (up to 3,000mg per day). Only long-term, high-dose use (over 3,500mg daily for more than two weeks) shows possible concerns. Doxylamine and pyridoxine (Diclegis), the combination used for morning sickness, has been studied in over 1,000 pregnancies and shows no increased risk of birth defects. It’s safer than many herbal remedies that are unregulated and poorly studied. Antihistamines like loratadine (Claritin) and cetirizine (Zyrtec) are Category B-meaning animal studies show no risk, and human studies haven’t found harm. Yet many women are told to avoid them in the first trimester. That’s outdated advice. These drugs are safe when needed. Metformin, used for PCOS and gestational diabetes, is safe throughout pregnancy. A woman on Reddit stopped her metformin at 8 weeks out of fear-only to end up hospitalized at 14 weeks with dangerously high blood sugar. ACOG recommends continuing it unless there’s a specific reason not to.
How to Make Smart Decisions
The biggest problem isn’t lack of information-it’s inconsistent advice. A 2023 survey found that 73% of pregnant people got conflicting guidance from different providers about the same medication. Here’s how to cut through the noise:- Use gestational age from fertilization, not your last period. Most risk windows are measured from conception. If your doctor says “week 10,” ask if that’s from your LMP or ultrasound. A 5-day dating error can mean the difference between a safe and risky exposure.
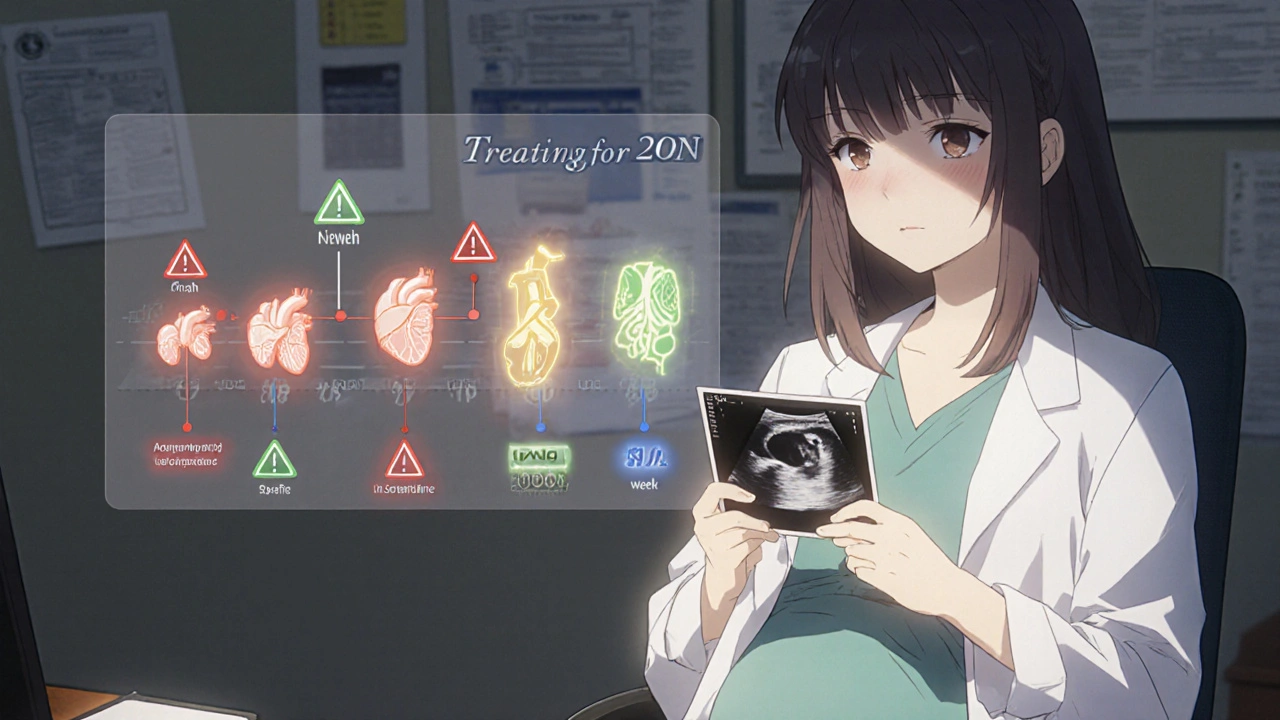
- Check the TERIS database or Micromedex for trimester-specific data. These aren’t just drug lists-they show risks by week.
- Use the CDC’s Treating for Two tool. It’s free, evidence-based, and gives you trimester-specific guidance for over 100 medications.
- Don’t stop meds cold turkey. If you’re on an antidepressant or blood pressure pill, work with your doctor to switch or taper safely. Stopping suddenly can be more dangerous than the drug itself.
- Ask your provider: “Is this medication necessary? Is there a safer alternative? What’s the risk if I don’t take it?”
What’s Changing in 2025?
Regulations are catching up. Since 2015, the FDA replaced the old A-B-C-D-X letter categories with the Pregnancy and Lactation Labeling Rule (PLLR). Now, drug labels include detailed sections on trimester-specific risks, clinical considerations, and data from pregnancy registries. In 2023, the NIH launched a $4.7 million project to build a real-time medication risk calculator that factors in your genetics, exact gestational age, and how your body processes drugs. Early prototypes are expected by mid-2025. Meanwhile, the European Medicines Agency now requires all new drug applications to include trimester-stratified data-meaning future medications will come with clearer, more precise safety info.Bottom Line: It’s Not About Avoiding All Drugs-It’s About Timing Them Right
You don’t need to suffer through morning sickness, anxiety, or high blood pressure because you’re afraid of medication. The goal isn’t zero exposure-it’s smart exposure. The safest strategy? Talk to your provider early. Know your exact gestational age. Use trusted resources like Treating for Two or MotherToBaby. And never stop a necessary medication without a plan. About 2-3% of birth defects are linked to medications. But with the right timing, most of those can be avoided. You’re not just protecting your baby-you’re protecting your own health, too.Is it safe to take Tylenol during pregnancy?
Yes, acetaminophen (Tylenol) is considered the safest pain reliever during pregnancy. Studies involving over 215,000 pregnancies show no increased risk of birth defects or developmental issues at standard doses (up to 3,000mg per day). Long-term, high-dose use (over 3,500mg daily for more than two weeks) may carry some risk, so stick to the lowest effective dose for the shortest time.
Can I take ibuprofen while pregnant?
Ibuprofen is generally safe before week 20, but should be avoided after that. After week 20, it can reduce amniotic fluid levels and increase the risk of kidney problems in the baby. After week 32, it can cause the baby’s heart to close a vital blood vessel too early, leading to serious complications. Always switch to acetaminophen after the first trimester unless your doctor advises otherwise.
Are SSRIs safe during pregnancy?
Some SSRIs are safer than others. Sertraline (Zoloft) has the best safety profile in the first trimester with no increased risk of birth defects. Paroxetine (Paxil) increases the risk of heart defects if taken early and can cause withdrawal symptoms in newborns if taken late. If you’re on an SSRI, work with your doctor to switch or taper gradually-especially in the third trimester-to reduce the chance of neonatal adaptation syndrome.
What should I do if I took a medication before I knew I was pregnant?
Don’t panic. Before day 20 after fertilization, most medications follow an “all-or-nothing” rule: either the pregnancy ends, or it continues without harm. If you took a medication after that, the risk depends on the drug and exact timing. Contact your provider or call MotherToBaby (1-866-626-6847) for a free, expert risk assessment. They’ll help you understand if you need further testing or monitoring.
Why do different doctors give me different advice about the same medication?
Because pregnancy medication data is complex, and not all providers have access to up-to-date, trimester-specific resources. Many still rely on outdated guidelines or general warnings. A 2023 survey found that 73% of pregnant people received conflicting advice. Use trusted tools like Treating for Two or the TERIS database to bring evidence-based info to your appointments. Ask your provider: “What’s the source of this recommendation?”
How do I know my gestational age accurately?
Last menstrual period (LMP) dating is often inaccurate. Ultrasound dating, especially between weeks 8 and 13, is the gold standard. If you’re unsure about your exposure timing, ask for an early ultrasound. A 5-day error in dating can lead to unnecessary worry-or missed risk. Most major risk windows are defined from fertilization, not your last period, so accurate dating is critical.



sharicka holloway
November 28, 2025 AT 02:24Finally, someone broke this down without fear-mongering. I took Zofran at 7 weeks and panicked for months-turns out my baby is fine. This post saved me from unnecessary guilt.
Alex Hess
November 29, 2025 AT 22:32This is what happens when you let laypeople interpret clinical data. You cite studies, but you ignore confounding variables, sample bias, and the fact that 90% of these ‘risks’ are statistically insignificant. People need to stop treating pregnancy like a minefield.
Leo Adi
November 30, 2025 AT 15:34In India, we don’t have access to most of these databases. My doctor told me to avoid all pills unless it’s a life-or-death situation. I took paracetamol for fever at 12 weeks-no one told me it was safe. I wish I’d had this guide. Thank you for writing it.
Mira Adam
December 2, 2025 AT 13:48So we’re supposed to trust a blog post over decades of medical caution? The fact that you’re reducing complex fetal development to a timeline suggests you’ve never held a newborn with a congenital defect. This isn’t optimization-it’s rationalization.
Miriam Lohrum
December 4, 2025 AT 11:49There’s a quiet dignity in accepting uncertainty. We don’t need perfect data to make wise choices-just humility. The real risk isn’t the medication, it’s the belief that we can control everything. Sometimes, the best thing you can do is listen-to your body, your doctor, and the silence in between.
Frances Melendez
December 5, 2025 AT 03:29You’re normalizing drug use during pregnancy like it’s a grocery list. What about the long-term neurological effects? What about the kids who grow up on SSRIs because their moms were too lazy to try therapy? This isn’t empowerment-it’s pharmaceutical convenience dressed up as science.
Rebecca Price
December 5, 2025 AT 09:36Edward, I’m glad you’re here. I just read this post after my OB told me to stop my metformin at 8 weeks. I did-and ended up in the hospital with gestational diabetes. I wish I’d had this before. Thank you for being the voice that says: ‘Don’t stop. Ask better questions.’
Edward Batchelder
December 5, 2025 AT 18:56Thank you, Rebecca. I’ve been trying to get my sister to read this for weeks. She’s 14 weeks and terrified of every pill she’s ever taken. This is exactly the calm, clear, evidence-based guide we need. No hype. No fear. Just facts. Please share this everywhere.