When a drug goes straight into your bloodstream, there’s no second chance. No stomach acid to kill off contaminants. No immune system on standby. That’s why sterile manufacturing for injectables isn’t just about cleanliness-it’s about survival. A single bacterium in a vial can trigger sepsis. A trace of endotoxin can cause organ failure. And in the last decade, we’ve seen what happens when it goes wrong: 64 deaths from contaminated steroids in 2012, recalls affecting thousands, and billions lost in failed batches.
Why Sterile Manufacturing Is Non-Negotiable
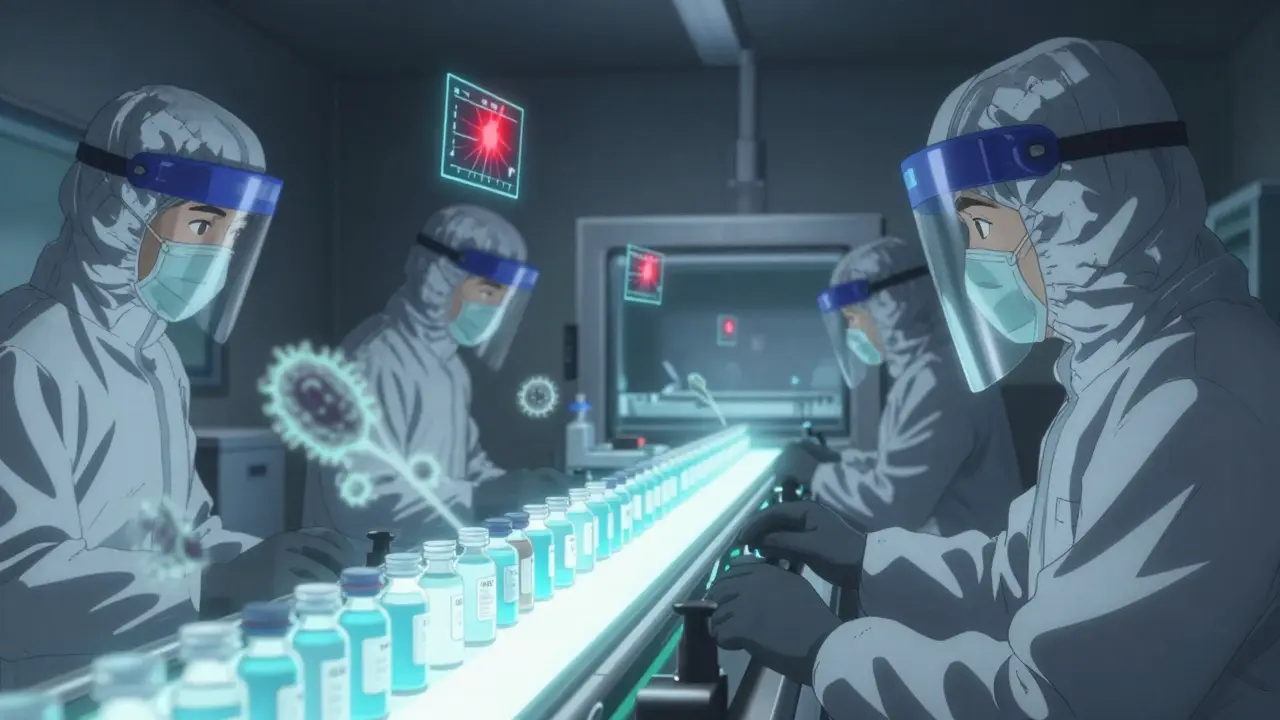
Oral pills dissolve in the gut. Creams sit on the skin. But injectables? They bypass every natural barrier. That’s why the standards for sterile manufacturing are among the strictest in all of pharmaceutical production. The goal isn’t just "clean." It’s sterile-meaning no living organisms, no particles, no endotoxins. The World Health Organization sets the bar at a contamination probability of less than one in a million (SAL 10^-6). That’s not a suggestion. It’s a legal requirement under FDA, EU GMP Annex 1, and WHO guidelines. This isn’t theoretical. In 2022, the FDA cited 1,872 deficiencies in sterile manufacturing facilities-up from 1,245 in 2019. Most of these weren’t about paperwork. They were about people, processes, and environments that failed to hold the line against contamination.Two Paths to Sterility: Terminal vs. Aseptic
There are only two ways to make a sterile injectable: terminal sterilization or aseptic processing. And they’re not interchangeable. Terminal sterilization means you fill the product, seal it, then kill everything inside with heat or radiation. Steam at 121°C for 15-20 minutes is the gold standard. It’s reliable, proven, and achieves a sterility assurance level of 10^-12-far beyond the required 10^-6. But here’s the catch: only 30-40% of injectables can survive this. Biologics like monoclonal antibodies, mRNA vaccines, and protein-based therapies? They’ll denature. They’ll fall apart. So for these, you need aseptic processing. Aseptic processing is like performing brain surgery in a dust storm. You never sterilize the final product. Instead, you sterilize everything around it: the containers, the equipment, the air, the gloves, the operators. Everything happens in an ISO 5 cleanroom-the equivalent of a Class 100 room-with no more than 3,520 particles per cubic meter larger than 0.5 microns. That’s less than the dust you’d find on a laptop keyboard after a week. The FDA and EU both require RABS (Restricted Access Barrier Systems) or isolators for aseptic filling. Isolators are sealed, glove-box-like chambers. RABS are open-front barriers with laminar airflow. Both aim to keep operators from touching the product. But isolators reduce contamination risk by 100 to 1,000 times compared to traditional cleanrooms, according to industry experts. The trade-off? They cost 40% more to install and maintain.The Hidden Rules: Cleanrooms, Water, and Air
It’s not just about the filling line. Every step before it matters.- Water for Injection (WFI) must have endotoxin levels below 0.25 EU/mL. That’s stricter than drinking water standards by a factor of 10,000. WFI isn’t just purified-it’s distilled or reverse-osmosis filtered and stored at 70-80°C to prevent microbial growth.
- Containers (vials, syringes, cartridges) must be depyrogenated. That means heating them to 250°C for at least 30 minutes to destroy endotoxins from bacterial cell walls. A single failed depyrogenation run can contaminate an entire batch.
- Airflow in ISO 5 zones must be unidirectional-like a silent, invisible wall of filtered air moving at 0.3-0.5 meters per second. It sweeps particles away from the product, never toward it.
- Pressure differentials between rooms are critical. ISO 8 gowning areas must be at +10 to +15 Pascals relative to ISO 7 corridors, which must be +10 to +15 relative to ISO 5 filling rooms. If pressure drops, contaminated air flows in.
- Temperature and humidity are tightly controlled: 20-24°C and 45-55% RH. Too dry? Static builds up and attracts particles. Too humid? Microbes thrive.

Testing for Failure Before It Happens
You can’t test sterility into a product. You can only prove you didn’t mess it up. That’s where media fill simulations come in. Every six months, manufacturers run a fake production run using growth media instead of the actual drug. They fill thousands of units-5,000 to 10,000-and incubate them for 14 days. If even one vial grows bacteria? The entire process fails. The FDA says a failure rate above 0.1% means your aseptic technique is broken. Real-world example: A top-10 pharma company had three media fill failures in one quarter because of tiny holes in their RABS gloves. Each failure cost $450,000 in lost product, retraining, and downtime. That’s not an outlier. A 2022 BioPhorum survey found 68% of sterile facilities had at least one sterility test failure per year-with an average cost of $1.2 million per event. Environmental monitoring is continuous now. Gone are the days of weekly air samples. EU GMP Annex 1 (2022) requires real-time particle and microbial monitoring. Air samplers must detect as low as 1 CFU per cubic meter in ISO 5 zones. If you hit an Alert Level of 1 CFU/m³, you investigate. At Action Level 5 CFU/m³? You stop production.Costs, Risks, and the Growing Market
Sterile manufacturing isn’t cheap. Setting up a small-scale facility-5,000 to 10,000 liters annual capacity-costs $50 to $100 million. A single aseptic filling line can run $15-25 million. Terminal sterilization? Around $50,000 per batch. Aseptic? $120,000 to $150,000. Why the gap? It’s not just equipment. It’s labor, training, validation, monitoring, and the constant risk of batch loss. But the market is growing fast. Sterile injectables hit $225 billion in 2023 and are projected to reach $350 billion by 2028. Biologics-monoclonal antibodies, gene therapies, cell therapies-are driving 65% of that growth. And over 40% of all new drug approvals now require sterile delivery. The problem? Many facilities aren’t ready. Only 28 of 1,200 Chinese sterile manufacturing sites passed FDA inspections in 2022. In the U.S. and EU, 68% of inspection deficiencies relate to aseptic technique failures. Training isn’t optional. Operators need 40-80 hours of aseptic technique training annually, plus semi-annual media fill qualifications. And documentation? One production run generates 250-300 pages of records. Nearly 20% of those pages are dedicated to sterility assurance alone.
What’s Changing Now?
The rules are tightening. The FDA’s 2023 guidance on aseptic processing pushes for continuous manufacturing and advanced process controls. ISO 14644-17:2023 now requires real-time monitoring of airborne particles and microbes. Closed processing systems-where the product never leaves a sealed environment-are now in 65% of new facilities, down from 40% just five years ago. Automation is rising. One company switched from manual visual inspection to automated systems and cut defect rates from 0.2% to 0.05%. The catch? It cost $2.5 million. But when a single contaminated vial can trigger a recall affecting thousands of patients, the ROI is clear. Rapid microbiological methods are cutting test times from 14 days to 24 hours. Digital twins-virtual models of production lines-are being used to simulate failures before they happen. And AI is starting to predict contamination risks based on historical data from environmental monitors.Bottom Line: No Room for Error
Sterile manufacturing for injectables isn’t about meeting a checklist. It’s about building a culture where every action, every glove change, every air filter replacement, every media fill result, matters. One mistake can kill. One delay can cost millions. One failure can destroy trust. The companies winning now aren’t the ones with the biggest budgets. They’re the ones with the most disciplined processes, the best-trained staff, and the humility to know that even the smallest oversight can have the biggest consequence. If you’re producing or using injectables, you’re not just buying a drug. You’re buying a guarantee that every step-from the water used to the gloves worn-was designed to protect life. That’s the standard. And it’s non-negotiable.What’s the difference between terminal sterilization and aseptic processing?
Terminal sterilization kills microbes after the product is sealed, using heat or radiation. It’s reliable but only works for products that can handle high temperatures or radiation-about 30-40% of injectables. Aseptic processing keeps everything sterile during production without final heat treatment. It’s used for sensitive biologics like antibodies and vaccines but requires extreme control over air, surfaces, and personnel. Aseptic processing is more complex and costly, but it’s the only option for heat-labile drugs.
Why is ISO 5 so important in sterile manufacturing?
ISO 5 is the cleanest classification for aseptic filling zones, allowing no more than 3,520 particles ≥0.5μm per cubic meter. This level of cleanliness is required because injectables enter the bloodstream directly. Even a single particle carrying a microbe can cause infection. ISO 5 zones use unidirectional airflow, high air change rates (20-60 per hour), and strict gowning protocols to minimize contamination risk. Anything less than ISO 5 is not permitted for direct product contact.
What happens if a media fill fails?
A media fill failure means the aseptic process failed to prevent contamination during simulation. The batch is rejected, and production stops. The company must investigate the root cause-glove tears, improper gowning, airflow disruption, training gaps-and fix it before restarting. The FDA requires re-validation with at least three consecutive successful media fills. A failure rate above 0.1% triggers regulatory scrutiny and can lead to warning letters or facility shutdowns.
Are isolators better than RABS for sterile manufacturing?
Isolators provide a fully enclosed, sealed environment, reducing contamination risk by 100-1,000 times compared to traditional cleanrooms. RABS are open-front barriers with laminar airflow and are easier to operate and maintain. Studies show both can achieve similar contamination rates when operated correctly. Isolators are preferred for high-risk products and complex processes, but RABS are still widely used and accepted by regulators if properly validated and maintained. The choice depends on product type, scale, and operational culture.
How often do sterile manufacturing facilities fail inspections?
In 2022, the FDA cited 1,872 deficiencies in sterile manufacturing facilities-up from 1,245 in 2019. About 68% of these were related to aseptic technique failures, 37% to inadequate environmental monitoring, and 28% to media fill failures. Personnel training issues accounted for 22%. These numbers show that human error and procedural gaps are the biggest risks, not equipment failure. Facilities that invest in continuous training, real-time monitoring, and automation see significantly fewer deviations.
Payton Daily
December 29, 2025 AT 03:51Man, I just read this and I’m sitting here thinking-how the hell do they even sleep at night? One tiny mistake and someone’s kid dies from a shot meant to save them. It’s not just science, it’s like a religious ritual at this point. You gotta believe in the process, or it breaks.
ANA MARIE VALENZUELA
December 29, 2025 AT 21:33Let’s be real-this whole system is a house of cards held together by overworked techs and fear of FDA letters. 1,872 deficiencies in 2022? That’s not ‘strict standards,’ that’s systemic collapse. They’re papering over human error with more checklists. Pathetic.
Bradly Draper
December 31, 2025 AT 10:24I work in a hospital pharmacy. I’ve seen what happens when a batch goes bad. It’s not just numbers on a report-it’s someone’s mom in ICU, wondering why her fever spiked after the ‘safe’ shot. This post? It’s the quiet truth no one talks about. Thank you.
Gran Badshah
January 2, 2026 AT 03:52bro in india we make injectables for 50 cents a vial and ship them worldwide… u think they got isolators? nah. they got gloves that tear and fans that blow dust. but hey, it’s cheap. and someone’s getting healed. maybe that’s the real tradeoff?
Vu L
January 2, 2026 AT 19:22Wait-so you’re telling me we’re spending $25 million on a machine that just moves liquid in a clean room… but we can’t cure cancer? This is capitalism in a nutshell. We fix the delivery system, not the disease. Brilliant.
oluwarotimi w alaka
January 3, 2026 AT 13:46they say ‘sterile’ but i know the truth… the fda and big pharma are in bed with the WHO. they want you dependent. why else would they make it so damn expensive? one bacterium? pfft. they just need you scared enough to pay $1,000 for a shot that should cost $2. the endotoxins? they’re in the water… on purpose. to keep you coming back.
Debra Cagwin
January 4, 2026 AT 20:08This is such an important conversation. So many people don’t realize how much care, training, and humility goes into every single vial. To the workers in those cleanrooms-you’re unsung heroes. Thank you for showing up, every day, even when no one’s watching.
Hakim Bachiri
January 5, 2026 AT 06:30Let me just say-this is why America leads. We have the cleanrooms. The isolators. The $2.5 million automated inspection systems. Meanwhile, Europe’s still using ‘laminar airflow’ like it’s 1998. And China? They’re still trying to spell ‘depolymerization.’ We don’t just make medicine-we make miracles. With precision. With excellence. With… punctuation.
Celia McTighe
January 5, 2026 AT 16:30Wow. Just… wow. 😭 I didn’t realize how much goes into this. I used to think pills were the hard part. But this? This is like watching a ballet where one misstep kills someone. Hats off to everyone in those rooms. 🙏💙
Ryan Touhill
January 7, 2026 AT 15:27It’s fascinating how we’ve elevated sterile manufacturing to an art form-yet still rely on humans to maintain it. We’ve built cathedrals of cleanliness… and then let untrained temps in with sweaty palms. The irony is poetic. And tragic.
James Hilton
January 8, 2026 AT 19:18So we spend $150K per batch to make sure a shot doesn’t kill you… but we can’t afford to pay nurses minimum wage? Yeah. That’s the American dream.
Mimi Bos
January 10, 2026 AT 00:23wait… so if u use a glove that’s been worn for 12 hours… and the air is too dry… and the temp is off by 1 degree… it’s all ruined? like… one little thing? that’s wild. i thought it was just ‘wash your hands’
Kelsey Youmans
January 10, 2026 AT 19:13While the technical details are compelling, one must not overlook the ethical imperative underpinning this entire discipline. The sanctity of the human body, the inviolability of the bloodstream-these are not regulatory concerns; they are metaphysical imperatives. To compromise sterility is to violate a covenant with life itself.
Sydney Lee
January 12, 2026 AT 11:14Everyone talks about contamination, but no one talks about the psychological toll. Imagine being the person who missed a tear in a glove. Imagine knowing you might have killed someone. That’s not a job. That’s a life sentence.
Teresa Marzo Lostalé
January 12, 2026 AT 23:36It’s funny… we build these insane systems to keep out one bacterium… but we let misinformation spread like wildfire on the internet. One fake post can kill more people than a bad vial. Maybe we need a sterile information cleanroom too. 🤔