When a patient walks into the ER with shortness of breath, the clock starts ticking. Is it heart failure? COPD? A pulmonary embolism? The difference between a quick discharge and a week-long hospital stay often comes down to one simple blood test: NT-proBNP.
Why NT-proBNP Is the First Test You Should Order
NT-proBNP isn’t just another lab value. It’s a direct signal from the heart. When the heart’s ventricles stretch under pressure-like in heart failure-they release this protein fragment into the bloodstream. The higher the level, the more strain the heart is under. Unlike symptoms that can mimic other conditions, NT-proBNP gives you an objective, measurable clue.
Here’s the real power: if the NT-proBNP level is below 300 pg/mL, heart failure is almost certainly ruled out. That’s a 98% negative predictive value. In plain terms, if the number is low, you can stop chasing heart failure and look elsewhere. This isn’t theory-it’s standard practice in the UK, the US, and across Europe. NICE guidelines, the ESC, and the AHA all say the same thing: order NT-proBNP for anyone with suspected acute heart failure.
Think about the cost savings. An echocardiogram runs over $3,000. A chest CT for suspected PE? Even more. But NT-proBNP? Around $18.42. And it’s fast. Most hospital labs turn it around in under an hour. In emergency departments across the UK, this test has cut unnecessary echocardiograms by 19% in just a few years.
When to Order It: The 5 Clear Clinical Scenarios
You don’t order NT-proBNP for everyone. But there are five clear situations where it’s not just helpful-it’s essential.
- Acute dyspnea in the ER or urgent care-Any adult over 40 presenting with sudden shortness of breath, especially if they have a history of hypertension, diabetes, or prior heart disease. Don’t wait for chest X-rays or ECGs. Order NT-proBNP first.
- Unexplained fatigue or swelling in older adults-Elderly patients often don’t have classic chest pain. They just feel tired, have swollen ankles, or can’t climb stairs anymore. These are red flags. NT-proBNP can catch early heart failure before it becomes severe.
- Worsening symptoms in known heart failure patients-If a patient with heart failure suddenly gains weight, feels more breathless, or needs more diuretics, check NT-proBNP. Rising levels mean the condition is worsening, even before symptoms get worse.
- Post-acute coronary syndrome (heart attack)-Even if the heart attack seems over, elevated NT-proBNP after a heart attack predicts higher risk of future heart failure or death. It helps decide who needs closer follow-up.
- Before major non-cardiac surgery in high-risk patients-Patients over 65 with diabetes or kidney disease undergoing hip replacement or cancer surgery? A pre-op NT-proBNP can predict who’s at risk for heart complications after surgery.
These aren’t guesses. They’re backed by 28 years of outcome data. Every major guideline agrees.
How to Interpret the Numbers-It’s Not Just One Cutoff
Here’s where things get tricky. NT-proBNP isn’t a simple yes-or-no test. The cutoff changes based on age, kidney function, and body weight.
For patients under 50: < 450 pg/mL rules out heart failure.
For patients 50-75: < 900 pg/mL.
For patients over 75: < 1,800 pg/mL.
Why? Because NT-proBNP naturally rises about 15-20% per decade-even in healthy people. If you use the same cutoff for a 25-year-old and a 78-year-old, you’ll misdiagnose half the elderly population.
And kidney disease? That’s another layer. If a patient has stage 3 or worse chronic kidney disease, NT-proBNP levels rise even without heart failure. In these cases, use a higher rule-out cutoff: < 1,200 pg/mL for patients with CKD stage 3-5. Don’t assume high = heart failure. Always check eGFR.
Obesity? That’s the opposite problem. Fat tissue suppresses NT-proBNP. For every 5-point increase in BMI, levels drop 25-30%. So if a severely obese patient has a level of 400 pg/mL, that’s actually high for them. Don’t dismiss it.
What NT-proBNP Can’t Tell You
This test is powerful, but it’s not magic. It doesn’t tell you why the heart is strained. It doesn’t show blockages, valve problems, or arrhythmias. That’s why it’s never used alone.
Here’s a common pitfall: a 78-year-old with atrial fibrillation and stage 3 kidney disease has an NT-proBNP of 850 pg/mL. Is this heart failure? Or just aging, AFib, and CKD? No one knows for sure. That’s why you need the full picture: symptoms, exam, ECG, kidney function, and sometimes an echo. NT-proBNP narrows the field-it doesn’t close the case.
And don’t order it for asymptomatic patients. Medicare data shows 18% of NT-proBNP tests are ordered in people with no symptoms. That’s wasted money and leads to unnecessary anxiety. The test is for people with signs of heart strain-not for routine screening.
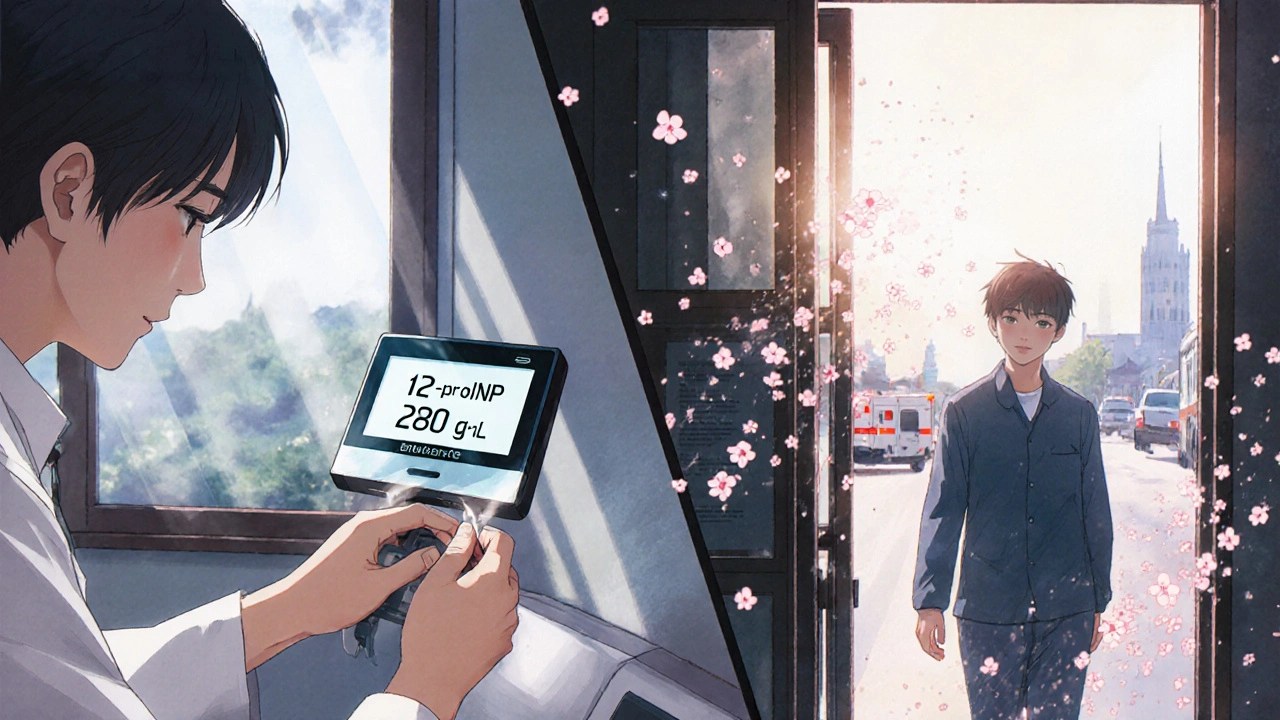
Point-of-Care Testing Is Changing the Game
Five years ago, you had to wait hours for results. Now, point-of-care devices like the Roche Cobas h 232 give you NT-proBNP levels in 12 minutes. That’s faster than drawing blood.
In rural clinics or urgent care centers without on-site labs, this is a game-changer. A doctor can test, interpret, and decide whether to send the patient to the hospital-all in one visit. In the UK, pilot programs in community clinics saw 31% fewer unnecessary ambulance transfers after adopting point-of-care NT-proBNP.
The accuracy? Within 95% of lab results. It’s not perfect, but it’s good enough to rule out heart failure quickly. And speed saves lives.
What’s Next for NT-proBNP?
The 2024 ACC/AHA/HFSA guidelines will expand its use to risk-stratify patients after a heart attack. Early data from the VICTORIA trial shows that if NT-proBNP drops after treatment, the risk of death or hospitalization falls by 35%. That means the test isn’t just for diagnosis-it’s becoming a tool to guide therapy.
But the biggest threat isn’t new technology. It’s overuse. With easy access and high reimbursement, some clinicians order it reflexively. The solution? Standardized protocols. Hospitals that implemented ordering rules-like requiring a clinical suspicion of heart failure before testing-reduced inappropriate orders by 33%.
NT-proBNP is here to stay. It’s the most validated cardiac biomarker we have. But like any tool, it’s only as good as the person using it. Know when to order it. Know how to read it. And never forget: it’s one piece of the puzzle.






Stephanie Deschenes
November 26, 2025 AT 01:16NT-proBNP is one of those tests that should be in every ER protocol. I’ve seen too many patients wait hours for echo results while we could’ve ruled out HF in 20 minutes with a simple blood draw. The cost savings alone make it a no-brainer.
And the age-adjusted cutoffs? Absolutely critical. I once dismissed a 79-year-old’s 800 pg/mL as ‘normal’ because I forgot to adjust for age. Turned out she had silent HF. Lesson learned.
Also, never ignore kidney function. I had a patient with CKD stage 4 and a 1,600 pg/mL result-no HF, just uremia. If you don’t check eGFR, you’re just guessing.
Cynthia Boen
November 27, 2025 AT 21:16This is the most overhyped test in medicine. Everyone acts like it’s a magic bullet but it’s just another biomarker that gets misused by lazy docs who don’t want to think.
And don’t even get me started on point-of-care devices. They’re inaccurate half the time and cost 10x more than a lab draw. It’s all about billing, not patient care.
Bea Rose
November 28, 2025 AT 03:4498% negative predictive value? That’s statistically meaningless if the pre-test probability is 5%. You’re not ruling out heart failure-you’re ruling out a hypothesis based on flawed assumptions.
Also, the obesity correction factor is not standardized. Different hospitals use different formulas. That’s not evidence-based medicine. That’s chaos.
Michael Collier
November 29, 2025 AT 04:55Thank you for this comprehensive and clinically grounded overview. The emphasis on context-age, renal function, BMI-is precisely what separates appropriate use from reflexive ordering.
As a teaching attending, I now require residents to justify NT-proBNP orders with a brief clinical rationale before submission. This has reduced inappropriate testing by over 40% in our department.
The VICTORIA trial data on serial measurements as a therapeutic guide is particularly compelling and deserves wider adoption.
Shannon Amos
November 29, 2025 AT 21:49So let me get this straight-we’re paying $18 for a test that tells us if someone’s heart is crying, but we still can’t tell why? And we’re acting like this is the holy grail?
Meanwhile, my grandma’s been on a low-sodium diet for 12 years and still can’t climb stairs. No test needed. Just listen to her.
Ryan C
November 30, 2025 AT 20:09Correction: The 2024 ACC/AHA/HFSA guidelines do not yet formally endorse NT-proBNP for therapy guidance-this is extrapolated from the VICTORIA trial subgroup analyses, which are not yet Level A recommendations.
Also, point-of-care devices have a 12% inter-assay variability in obese patients. The 95% accuracy claim is misleading without specifying confidence intervals.
And no, you cannot reliably rule out HF in a 78-year-old with CKD stage 3 using <1,200 pg/mL without clinical correlation. That’s not a cutoff-it’s a suggestion.
Dan Rua
December 2, 2025 AT 06:53Great breakdown. I’ve been pushing this in my rural clinic for years. We got a point-of-care machine last year and it’s been a game-changer.
One patient came in with fatigue and swollen legs. We tested, got a 1,750 result, and sent her to the hospital-turns out she had severe LV dysfunction. She’s on meds now and feels better.
Just don’t forget: the test helps, but the patient still has to tell you what’s wrong. Listen to them first.
Mqondisi Gumede
December 2, 2025 AT 20:55Western medicine always thinks it has the answer with a number on a screen
But in Africa we know the body speaks louder than labs
My uncle had no test but walked 50km to the clinic and said I can't breathe
They gave him water and he lived
NT-proBNP is just another way to sell tests to rich people
Real medicine is in the hands not the machine
And who pays for this anyway
Who gets rich from this test
Not the patient
Not the nurse
Not the old man who can't climb stairs
It's the lab and the hospital CEO
That's the truth
Not your guidelines
Not your numbers
Not your $18 test
That's just capitalism dressed in white coats
Douglas Fisher
December 3, 2025 AT 02:19I just want to say how much I appreciate the clarity and precision in this post. It’s rare to see such thoughtful, nuanced, and evidence-based guidance on something as commonly misunderstood as NT-proBNP.
And thank you for highlighting the obesity paradox-it’s so often overlooked, and I’ve seen too many clinicians dismiss a 400 pg/mL result in a patient with a BMI of 42, when that’s actually alarmingly high for them.
Also, the point about not ordering it for asymptomatic patients? Absolutely vital. I’ve seen patients panic over a mildly elevated level with zero symptoms, and it leads to unnecessary stress, imaging, and even invasive procedures.
It’s a tool, not a crystal ball. And we owe it to our patients to use it wisely.
Thank you again.
-Douglas
Albert Guasch
December 3, 2025 AT 14:45NT-proBNP remains the most robust, reproducible, and clinically actionable biomarker in the management of acute heart failure syndromes.
Its utility in risk stratification, diagnostic exclusion, and therapeutic monitoring is well-documented across multiple randomized controlled trials and real-world registries.
Implementation of standardized, protocol-driven ordering criteria-coupled with clinician education on age- and renal-adjusted thresholds-has demonstrated significant reductions in diagnostic delays, unnecessary imaging, and healthcare expenditures.
Further, the advent of point-of-care platforms has expanded access to this critical diagnostic tool in resource-limited settings, thereby improving equity in care delivery.
This is not theoretical. This is practice-changing. And it is here to stay.
Ginger Henderson
December 5, 2025 AT 00:23Yeah, but what if the patient just has anxiety? I had one last week with a 1,100 level-no heart issues, just panic attacks. We did five tests before we figured it out.
So now I just tell people to breathe and drink water first. Saves money and avoids a whole lot of drama.