Phototoxicity Risk Calculator
Antibiotic Phototoxicity Risk Calculator
Select your antibiotic to see its phototoxicity risk level and specific protection recommendations.
Phototoxicity Risk Assessment
When you’re taking an antibiotic like doxycycline or ciprofloxacin, your skin becomes more sensitive to sunlight - not because you’re allergic, but because the drug reacts with UV light. This isn’t rare. About 1 in 5 people on these antibiotics get a painful sunburn-like reaction, even on cloudy days or through windows. Some end up with blisters, dark patches, or worse - and many stop their treatment early because of it. But you don’t have to. Preventing phototoxicity isn’t complicated. It’s about knowing which antibiotics are risky, when to take them, and how to protect your skin - the right way.
Know Which Antibiotics Cause Phototoxicity
Not all antibiotics do this. Some are safe. Others? High risk. If you’re prescribed one of these, you need to act:- Doxycycline - Highest risk among tetracyclines. Even at 100mg daily, it can trigger reactions in broad daylight.
- Ciprofloxacin - Commonly used for UTIs and respiratory infections. Moderate phototoxicity.
- Levofloxacin - Lower risk than ciprofloxacin, but still needs caution.
- Moxifloxacin and Gatifloxacin - Much safer. The chemical tweak at the C-8 position cuts photosensitivity by nearly 70%.
- Sulfonamides - Like Bactrim. Negligible risk. You can sunbathe safely here.
- Third-gen cephalosporins - Rare, but possible. Watch for unusual redness or spider veins after sun exposure.
If your doctor prescribes doxycycline for Lyme disease or pneumonia, don’t panic. But do ask: Is there a lower-risk option? For acne, minocycline is a gentler alternative to doxycycline - 6 times less likely to cause sunburn.
Take Your Antibiotic in the Evening
Timing matters more than you think. Taking your antibiotic at night - ideally 2 to 3 hours before bed - drops your phototoxic risk by nearly 40%. Why? Because your blood levels peak while you’re asleep, not when you’re outside at noon.This trick works best for fluoroquinolones like ciprofloxacin and levofloxacin. A 2017 study with 142 patients showed a clear drop in sunburns when doses were moved to evening. Even if you’re on doxycycline, shifting to bedtime helps. Your body clears the drug overnight. By morning, levels are lower. Less drug + less sun = less damage.
Sunscreen Isn’t Enough - Use SPF 50+
Most people think SPF 30 is fine. It’s not. With antibiotics, you need SPF 50 or higher. Why? Because SPF 30 blocks only about 55% of the UV rays that trigger phototoxicity. SPF 50+ blocks 92%. That’s a massive difference.And it’s not just about the number. You need broad-spectrum - meaning it protects against UVA (315-400 nm), not just UVB. UVA is the main culprit. It penetrates deeper, causes long-term damage, and passes through glass. Look for ingredients like zinc oxide, avobenzone, or ecamsule. Reapply every hour if you’re outside, even if it says "water-resistant." Antibiotics make sunscreen break down faster - up to 65% quicker than normal.
Clothing Matters More Than You Realize
A white cotton T-shirt? It’s basically useless. Standard cotton has a UPF (Ultraviolet Protection Factor) of only 5 to 10 - meaning it blocks just 60% to 80% of UV rays. That’s worse than sunscreen.Wear clothing labeled UPF 40 or higher. UPF 50+ blocks 98% of UV radiation. Look for tightly woven synthetics like polyester or nylon blends. Dark colors help, too. A black UPF 50 shirt is better than a white one, even if both are rated the same.
Don’t forget your head. A wide-brimmed hat (at least 3 inches) blocks 95% of UV from your face, neck, and ears. A baseball cap? Only 45%. If you’re outside for more than 15 minutes, wear a hat. Always.

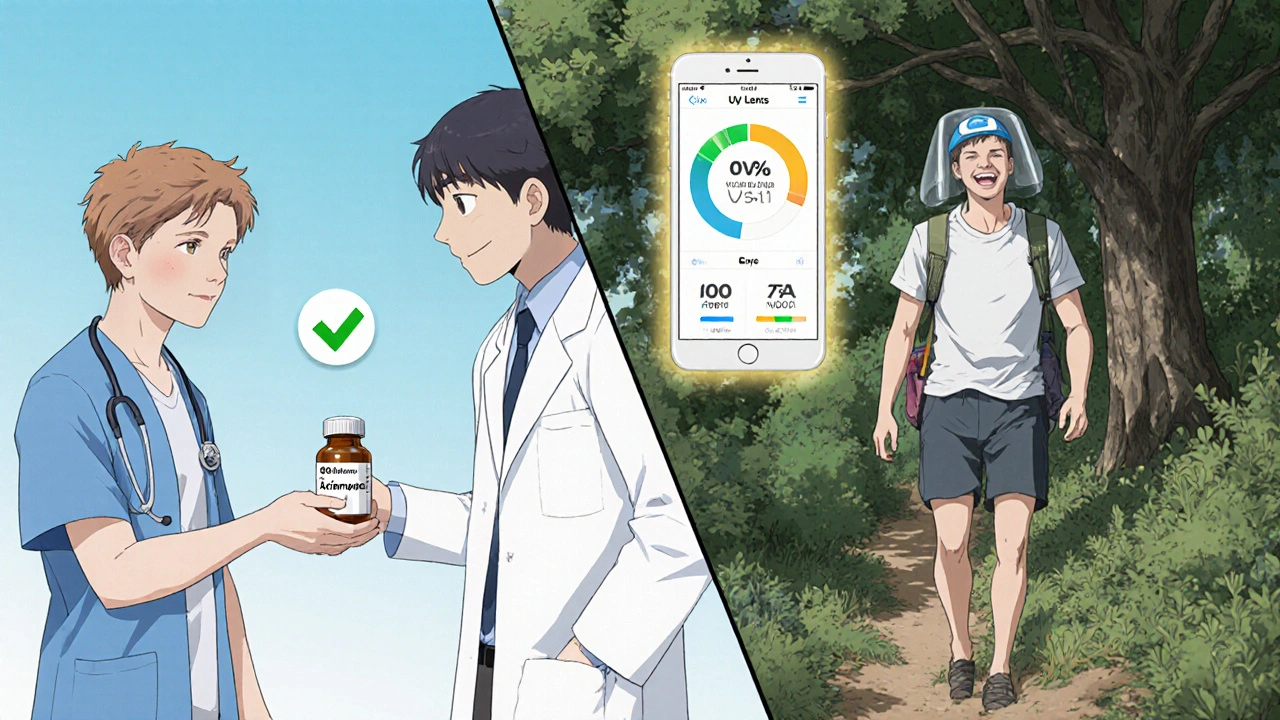
Use Technology to Stay Safe
Most people forget to reapply sunscreen. Or they think they’re safe on cloudy days. A 2022 survey found 68% of patients got the basics wrong.Fix that with a free app. UV Lens - downloaded over 12 million times - gives real-time UV index alerts and reminds you when to reapply sunscreen based on your medication. In a 2023 trial with 200 people, those using the app had 52% better adherence than those who didn’t. That’s the difference between getting burned and staying safe.
Set phone alarms: "Reapply sunscreen," "Wear hat," "Stay indoors 10 a.m.-4 p.m." Simple. Effective. Free.
When to Ask for a Different Antibiotic
If you’re an outdoor worker, gardener, athlete, or parent who spends hours outside, ask your doctor: Is there a non-phototoxic alternative?Studies show 28% of dermatologists change antibiotics for patients with high sun exposure. For example:
- Instead of doxycycline for Lyme disease? Azithromycin may work in early stages.
- Instead of ciprofloxacin for a UTI? Nitrofurantoin or fosfomycin have zero phototoxic risk.
Don’t assume your doctor knows. Bring up phototoxicity. Cite the risk: 5.7% of doxycycline users get sunburns. That’s more than 1 in 20. If you’re active outdoors, that’s unacceptable.
What About Long-Term Use? (Like for Acne)
Photoprotection works great for short courses - 7 to 14 days. But for acne treatment, where you’re on antibiotics for months? It fails. Even people who follow every rule - sunscreen, hat, evening dose - still get reactions 62% of the time.That’s why dermatologists now recommend switching to non-antibiotic options after 3 months: topical retinoids, azelaic acid, or spironolactone. Long-term antibiotics aren’t just risky for your skin - they’re bad for your microbiome and contribute to antibiotic resistance.
If you’ve been on doxycycline for acne for over a year, talk to your dermatologist about alternatives. There are better, safer ways to clear skin.
What About New Treatments?
There’s promising new science. In 2023, the FDA approved a supplement containing β-carotene and soybean trypsin inhibitor - taken with high-risk antibiotics - that cuts phototoxic reactions by 63%. It’s not a replacement for sun protection, but it’s a backup.Also, new antibiotics like gepotidacin are being developed with zero phototoxicity. By 2026, more of these will be available. But for now, the tools you have are enough - if you use them right.
Bottom Line: You Can Avoid This
Phototoxicity isn’t a side effect you have to live with. It’s preventable. You don’t need to stop your antibiotic. You don’t need to quit life outdoors. You just need to know:- Which drug you’re on - and its risk level
- Take it at night
- Use SPF 50+ broad-spectrum sunscreen - and reapply every hour
- Wear UPF 40+ clothing and a wide-brimmed hat
- Use a UV app to track exposure
- Ask for a safer alternative if you’re outside a lot
One study found that when patients got clear, structured advice, phototoxicity dropped by 43%. That’s not magic. That’s education.
Don’t let a prescription turn your summer into a hospital visit. Protect your skin like you protect your health - with smart choices, not just luck.
Can I still go outside if I’m on doxycycline?
Yes - but you need to be extra careful. Avoid direct sun between 10 a.m. and 4 p.m. Wear UPF 50+ clothing, a wide-brimmed hat, and SPF 50+ sunscreen. Reapply every hour. Take doxycycline at night. If you follow these steps, you can enjoy outdoor time without burning.
Is SPF 30 enough for antibiotics?
No. SPF 30 blocks only about 55% of the UV rays that cause phototoxic reactions. SPF 50+ blocks 92%. With antibiotics, your skin is more vulnerable. Using SPF 30 is like wearing a thin raincoat in a storm - you’ll get soaked. Stick to SPF 50+ and reapply often.
Does sunscreen wear off faster when I’m on antibiotics?
Yes. Studies show conventional sunscreens break down up to 65% faster under antibiotic-induced photosensitivity. That’s why reapplying every hour - not every two - is critical. Even "water-resistant" labels don’t mean much here. Set a phone reminder.
Can I use tanning beds while on antibiotics?
Absolutely not. Tanning beds emit concentrated UVA radiation - the exact type that triggers phototoxicity. Even one session can cause severe burns, blistering, or long-term skin damage. Avoid them completely while on high-risk antibiotics like doxycycline or ciprofloxacin.
Are there antibiotics that don’t cause sun sensitivity?
Yes. Sulfonamides like Bactrim, most penicillins, macrolides like azithromycin, and newer antibiotics like gepotidacin have little to no phototoxic risk. If you’re outdoors often, ask your doctor if one of these can replace a high-risk drug like doxycycline or ciprofloxacin.
How long does phototoxicity last after stopping the antibiotic?
The drug clears from your system in 1 to 3 days, but skin damage can linger. Redness and peeling may last a week. Dark spots (hyperpigmentation) can take weeks to months to fade - sometimes permanently. The best approach? Prevent it before it starts.
Should I avoid sunlight completely while on antibiotics?
No. You don’t need to become a hermit. Just avoid peak sun hours (10 a.m.-4 p.m.), wear protective clothing and hat, and use SPF 50+ sunscreen. You can walk the dog, go to the park, or sit on your porch - just protect yourself like you would in a desert.
Can children get phototoxicity from antibiotics?
Yes. Children on doxycycline (for Lyme disease or certain infections) are just as vulnerable. Use the same rules: SPF 50+, UPF clothing, hats, evening dosing. Avoid prolonged sun exposure. If your child is on antibiotics and plays outside, treat sun protection like a daily hygiene habit - like brushing teeth.
What to Do Next
If you’re currently on an antibiotic:- Check the name. Is it doxycycline, ciprofloxacin, or levofloxacin? If yes, proceed.
- Switch your dose to bedtime - tonight.
- Buy a broad-spectrum SPF 50+ sunscreen if you don’t have one.
- Get a UPF 50+ hat and a long-sleeve shirt for outdoor time.
- Download UV Lens and set daily reminders.
- Call your doctor: "Is there a non-phototoxic alternative for my condition?"
One week of these steps can save you from weeks of pain, healing, and scarring. Your skin will thank you - and so will your treatment plan.






Natashia Luu
November 25, 2025 AT 07:19While I appreciate the technical depth of this post, the casual tone undermines its medical credibility. Phototoxicity is not a lifestyle inconvenience-it is a pharmacological hazard requiring clinical-grade precautions. The suggestion to "just take it at night" is dangerously reductive. Patients with renal impairment or those on multiple medications may have altered pharmacokinetics that render this advice ineffective. Always consult a pharmacist before altering dosing schedules. This is not a blog post-it is a public health document.
akhilesh jha
November 27, 2025 AT 02:28Interesting. I took doxycycline for three weeks last year and never had a reaction. But I also never went outside after 6 p.m. Maybe it’s not the drug-it’s the timing of my life. I work night shifts. Sunlight was never an issue. Still, I never thought about UPF clothing. I wore a hoodie and called it a day. Maybe that’s why I got lucky.
Jeff Hicken
November 27, 2025 AT 06:43spf 50+?? come on. i mean, really? i used spf 30 and just stayed in the shade. no big deal. also who even has time to reapply sunscreen every hour? i work two jobs and i’m not some spa lady. also why are we all suddenly scared of the sun? it’s not like we’re in the desert. also my cousin got burned on doxy and she just used aloe and slept it off. problem solved.
Vineeta Puri
November 28, 2025 AT 03:23Thank you for this comprehensive and evidence-based guide. As a healthcare provider, I frequently encounter patients who discontinue essential antibiotics due to fear of phototoxicity-often because they were never properly counseled. Your breakdown of risk levels by drug class is invaluable. I especially appreciate the emphasis on non-antibiotic alternatives for chronic conditions like acne. This is exactly the kind of patient education that reduces unnecessary morbidity and antibiotic resistance. Please consider sharing this with your clinic’s patient portal.
Victoria Stanley
November 29, 2025 AT 22:52This is so helpful! I’ve been on doxycycline for Lyme and was terrified to go outside. I started taking it at night and bought a UPF 50 hat-game changer. I actually went hiking last weekend and didn’t burn once. Also, the UV Lens app is legit. I set a reminder to reapply and it saved me. You’re right-this isn’t about avoiding the sun, it’s about being smart about it. Thank you for writing this!
Andy Louis-Charles
November 30, 2025 AT 16:47SPF 50+ 🌞🧂
UPF 50+ 👕🧢
Evening dose 🌙
UV Lens app 📱
Don’t be a hero. Just protect your skin. You’re not invincible. I’ve seen too many people with permanent hyperpigmentation from this. Just do the five steps. It’s not hard. Your future self will high-five you.
Douglas cardoza
December 1, 2025 AT 05:15Man I just took my doxy in the morning and went to the beach. No biggie. I’m fine. I think this whole thing is overblown. My grandma took tetracycline in the 70s and she gardened every day. She’s 92 and still walks her dog. Maybe we’re just being too paranoid now? Also, sunscreen is expensive. Can’t we just wear a shirt?
steven patiño palacio
December 1, 2025 AT 21:46As a dermatology nurse in rural Appalachia, I see this every spring. Patients on doxycycline for acne show up with second-degree burns on their shoulders and necks, convinced they "didn’t do anything wrong." They wore a tank top, thought clouds meant safety, and skipped reapplication. This guide is not just helpful-it’s life-saving. I’ve printed copies for every patient on high-risk antibiotics. The ones who follow the five steps? Zero reactions. The ones who don’t? We’re treating them in the clinic for weeks. Education isn’t optional. It’s clinical care.
stephanie Hill
December 2, 2025 AT 05:44Wait-so you’re telling me the pharmaceutical companies knew about this for decades but never told us? And now we’re supposed to trust them enough to take a drug that turns our skin into a sunburned mess? And you want us to pay for SPF 50+ and UPF clothing while they profit off the antibiotics? This isn’t prevention-it’s corporate negligence dressed up as advice. Did you know the FDA approved doxycycline without requiring phototoxicity warnings until 2011? And now we’re supposed to be grateful for a blog post? I’m not taking anything until I see the full clinical trial data. And no, I won’t download an app. I’m not a beta tester for Big Pharma.
Akash Chopda
December 3, 2025 AT 17:02doxycycline is poison the sun is a weapon the government knows this they dont care you think sunscreen helps no it just makes you feel safe while they watch you burn
Sam Jepsen
December 5, 2025 AT 04:51Just wanted to say thank you for this. I’m a dad with two kids on antibiotics right now-one for Lyme, one for a bad ear infection. I’ve been stressing about them playing outside. This checklist? I printed it. Laminated it. Put it on the fridge. We’re doing evening doses, hats, and the UV app. My 8-year-old even reminds me now. You turned fear into action. That’s huge.
Yvonne Franklin
December 6, 2025 AT 00:30SPF 50+
Evening dose
UPF clothing
UV app
Ask for alternatives
Done. No drama. Just science.
Bartholemy Tuite
December 6, 2025 AT 13:49Look I’m from Ireland and we get maybe three sunny days a year so I never thought about this until my mate came back from Florida with his face looking like a lobster after taking cipro. He didn’t even know it was the antibiotic. We laughed at first. Then he had to take two weeks off work. That’s when I looked into it. Turns out the whole thing is wild-like, we’re told to take antibiotics and then told not to go outside? But nobody tells you how to do it right. This guide? It’s the first thing that actually made sense. I showed it to my GP. She said she’d start handing it out. Honestly? I think this should be mandatory reading with the prescription. Not a pamphlet. Not a warning label. A real guide. Like this one. You did good.