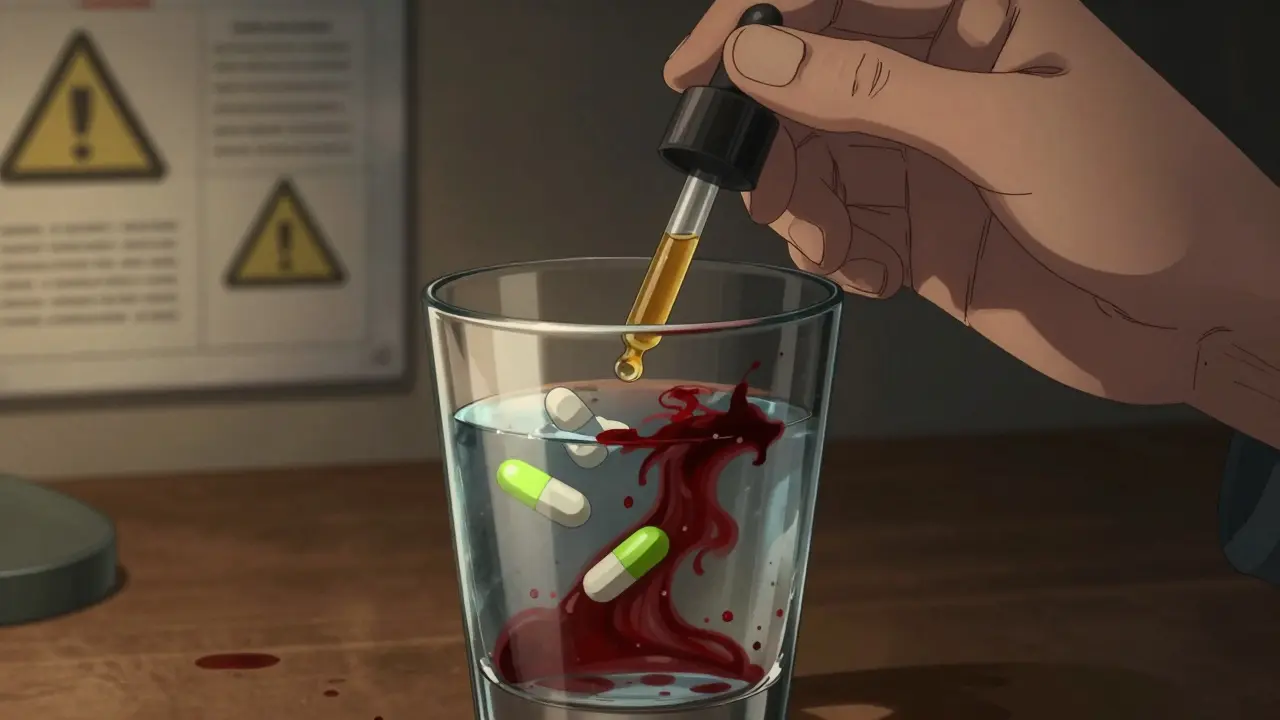
More people are using cannabis - whether it's CBD oil for anxiety, THC for chronic pain, or full-spectrum products for sleep - and many are taking prescription meds at the same time. But here’s the thing: cannabis doesn’t just sit quietly in your body. It talks to your medications. And sometimes, that conversation turns dangerous.
How Cannabis Changes How Your Medications Work
Your liver uses a group of enzymes called CYP450 to break down about 60% of all prescription drugs. CBD and THC, the main active compounds in cannabis, block these enzymes. When that happens, your meds don’t get processed the way they should. Some build up to toxic levels. Others get cleared too fast and stop working. For example, if you’re on warfarin - a blood thinner - and start taking CBD, your INR (a measure of how long it takes your blood to clot) can jump by nearly half in just a few days. That’s not a small bump. It means you could bleed internally without warning. One study tracked 17 cases where people on warfarin started CBD and ended up in the hospital with gastrointestinal bleeding. The same thing happens with clobazam, a seizure medication. CBD can make clobazam levels spike by up to 500%. Patients report feeling so drowsy they can’t walk. Neurologists have had to cut clobazam doses by 40% just to keep people safe. THC, meanwhile, affects different enzymes. It slows down how your body clears opioids like morphine and oxycodone. That doesn’t mean you’ll feel more pain relief - it means you’re at higher risk of slowed breathing, especially if you’re older or already taking other sedatives.Three Levels of Risk - Know Which Ones to Avoid
Not all interactions are created equal. Experts group them into three clear tiers. High-risk: Avoid or use extreme caution. These can kill you if ignored.- Warfarin: CBD raises INR levels dangerously fast. Some cases saw INR jump from 2.5 to over 6.0 in under 72 hours - a level where spontaneous bleeding becomes likely.
- Tacrolimus: Used after organ transplants to prevent rejection. Cannabis can make its levels triple or even quadruple. That means kidney damage, nerve damage, or even organ failure.
- Protease inhibitors: These are HIV medications. THC can reduce their effectiveness by 30-40%. That’s not just a side effect - it’s treatment failure, and it can lead to drug-resistant HIV.
- Benzodiazepines (like alprazolam): Add cannabis and you’re 47% more likely to fall, especially if you’re over 65. Drowsiness lasts longer. Some people need to cut their Xanax dose by 25%.
- Opioids: Even if you’ve been on them for years, adding cannabis can increase drowsiness and breathing problems. One study showed morphine clearance dropped by 30%.
- Calcium channel blockers (like amlodipine): Your blood pressure can drop too low. Dizziness, fainting, falls - all real risks.
- SSRIs (like sertraline): CBD may raise levels by 10-15%. Most people feel nothing. But if you start feeling unusually dizzy or nauseous, talk to your doctor.
- Statins (like atorvastatin): Levels go up a bit, but no cases of muscle damage (rhabdomyolysis) have been confirmed.
Formulation Matters - Full-Spectrum Isn’t the Same as Isolate
Not all CBD products are equal. A full-spectrum CBD oil contains trace amounts of THC, terpenes, and other cannabinoids. That might sound good - and it can be - but it also means stronger enzyme inhibition. Research shows full-spectrum products inhibit CYP3A4 by 22-37% more than pure CBD isolate at the same dose. That’s because of the “entourage effect” - the compounds work together to amplify each other’s actions. So if you’re on a high-risk med, using a full-spectrum product isn’t just a minor detail. It’s a major risk factor. And don’t assume “natural” means safe. A 2023 patient survey found that 63% of people using CBD with clobazam had increased sedation - and nearly a third needed a dose change. Many didn’t tell their doctors because they thought “it’s just CBD.”
How You Take It Changes Everything
Smoking or vaping cannabis? THC hits your bloodstream in under 10 minutes. That means sudden, sharp interactions - especially with sedatives. You might feel dizzy, disoriented, or pass out within minutes. Oral products - oils, gummies, capsules - take 2 to 4 hours to peak. The effect lasts 6 to 8 hours. That’s why interactions with warfarin or tacrolimus are delayed but longer-lasting. You might feel fine on day one, then wake up on day three with a dangerously high INR. Even cannabis tea? It doesn’t affect the same enzymes as oils or smoke. One study showed it didn’t interfere with cancer drugs like docetaxel. So the delivery method isn’t just about how fast you feel high - it’s about what your body does to your meds.Real Stories - What People Are Actually Experiencing
Reddit’s r/MedicalCannabis has over 1,200 posts from people sharing their real experiences. Here’s what they’re saying:- “I started CBD for my anxiety and kept taking my Xanax. Two weeks later, I couldn’t get out of bed. My doctor cut my dose by 30%.” - u/AnxietyWarrior, 2022
- “I’ve been on warfarin for 12 years. Took CBD for arthritis. Started bruising everywhere. INR was 7.2. ER visit. They said I was lucky I didn’t have a stroke.” - u/WarfarinSurvivor, 2023
- “I use 50mg CBD daily with oxycodone. No drowsiness. No issues. Been doing it for 8 months.” - u/ChronicPainSufferer, 2022
What You Should Do - A Simple 5-Step Plan
If you’re using cannabis and taking any prescription meds, don’t guess. Follow this:- Be honest with your doctor. Say exactly what you’re using: CBD oil? THC gummies? How much? How often? Don’t say “I take a little CBD.” Say “I take 25mg of full-spectrum CBD oil every night.”
- Check your meds. If you’re on warfarin, tacrolimus, clobazam, or any opioid or benzodiazepine, you’re in the high or moderate risk zone. Don’t assume it’s safe.
- Get baseline labs. Before starting cannabis, ask for a blood test. For warfarin users: INR. For transplant patients: tacrolimus trough level. For seizure meds: clobazam level.
- Test again after 48-72 hours. That’s when interactions peak. If your INR jumped from 2.8 to 4.5, your doctor needs to know - fast.
- Adjust slowly. Never change your med dose on your own. If you need to reduce your clobazam or warfarin, do it in 10-25% steps, under supervision.




Jacob Hill
January 19, 2026 AT 18:58Wow, this is terrifying-and so under-discussed. I’ve been on warfarin for AFib, and my cousin started CBD for back pain without telling anyone. Three weeks later, she was in the ER with a GI bleed. I printed out this whole post and gave it to my pharmacist. He had no idea. We need better education, not just warnings.
Christi Steinbeck
January 20, 2026 AT 04:16Thank you for writing this. As a nurse who’s seen too many patients self-medicate with ‘natural’ stuff, I’m so glad someone laid this out clearly. I’ve had to adjust doses for patients on clobazam after they started CBD-no one ever thinks to mention it until they’re falling over. You’re right: it’s not magic. It’s pharmacology. Treat it like a drug. Because it is.
Erwin Kodiat
January 20, 2026 AT 14:06I’ve been using full-spectrum CBD for chronic pain for 3 years now, on amlodipine and sertraline. No issues. But I also get my labs checked every 3 months and tell my doctor everything. I think the key isn’t avoiding cannabis-it’s being smart. I’ve seen people panic over this and quit meds cold turkey. That’s way more dangerous than the interaction.
Lydia H.
January 22, 2026 AT 01:39It’s wild how we treat weed like it’s harmless because it’s ‘plant-based,’ but we’d never take a new synthetic pill without checking interactions. Why the double standard? We’re not being consistent with how we view medicine. It’s not about fear-it’s about respect for the chemistry inside our bodies.
sujit paul
January 23, 2026 AT 15:49Let us not forget the deeper truth: the pharmaceutical-industrial complex fears plant medicine because it cannot be patented. The CYP450 inhibition? A distraction. The real agenda is control. CBD is not the villain-corporate greed is. The FDA's silence? Complicity. We are being manipulated into believing we need their approval to heal. The truth is in the leaf. The system fears what it cannot monetize.
Aman Kumar
January 24, 2026 AT 13:51As a pharmacologist trained in enzymology, let me clarify: CBD is a potent competitive inhibitor of CYP3A4 and CYP2C19-this is not speculative, it's in vitro and clinical pharmacokinetic fact. The 500% clobazam elevation? Documented in Epilepsia 2021. The INR spike? Confirmed in Thrombosis Research 2022. The problem isn't anecdotal-it's systemic. Yet, 76% of pharmacists remain untrained. This is malpractice waiting to happen. Stop romanticizing; start rationalizing.
Astha Jain
January 24, 2026 AT 18:59ok but like… i tried cbd for my anxiety and i swear it made my xanax work better?? i didnt change my dose and i felt way calmer?? maybe its just me?? idk maybe my liver is magic??
Phil Hillson
January 26, 2026 AT 00:32So let me get this straight… you’re telling me that a plant that’s been used for thousands of years is suddenly a silent killer because it messes with some lab numbers? Meanwhile, Big Pharma’s pills kill 100k people a year and nobody bats an eye? This is fearmongering dressed up as science. I’m not scared of CBD-I’m scared of people who profit off scaring me.
Josh Kenna
January 27, 2026 AT 04:13my mom took cbd with her blood pressure med and her bp dropped to 80/50 and she passed out in the shower. i was like ok this is real. now she only uses isolate and checks her levels. i dont get why people dont just ask their drs instead of googling and hoping for the best. also typo but i meant drs not dr. sorry
Valerie DeLoach
January 28, 2026 AT 05:40What’s missing here is the human cost of silence. People don’t disclose cannabis use because they fear judgment, legal repercussions, or being told to stop. But the real tragedy isn’t the interaction-it’s the lack of trust between patient and provider. We need compassionate, non-punitive education. Not just lists of risks. We need dialogue. We need to meet people where they are, not where we think they should be. Healing isn’t binary. It’s nuanced. And it requires listening.