When your immune system turns against your own body, things get messy fast. Autoimmune diseases like rheumatoid arthritis, lupus, and vasculitis don’t just cause pain-they can wreck organs, damage nerves, and shut down daily life. That’s where corticosteroids come in. These aren’t the muscle-building steroids bodybuilders use. They’re synthetic versions of cortisol, your body’s natural stress hormone, and they’re one of the fastest, most powerful tools doctors have to calm down runaway inflammation.
How Corticosteroids Work
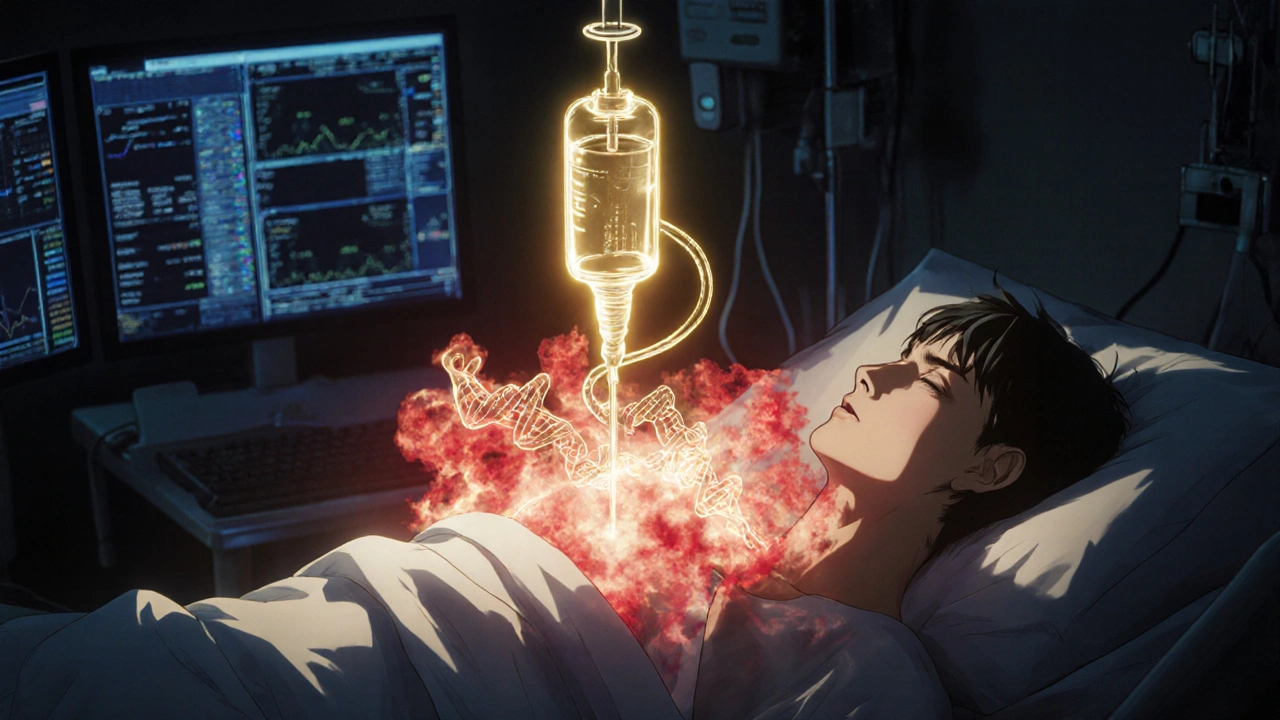
Corticosteroids like prednisone and methylprednisolone don’t just mask symptoms-they shut down the inflammation cascade at its source. Inside your cells, they bind to receptors that act like switches, turning off genes that produce inflammatory proteins. This means fewer cytokines like TNF-alpha and interleukins, less cyclooxygenase-2, and reduced activity of phospholipase A2, which is responsible for creating many of the chemicals that cause swelling and pain.
Unlike other immunosuppressants-like methotrexate or azathioprine-that take weeks to kick in, corticosteroids work in hours. A patient with sudden, severe lupus nephritis might go from bedridden to walking within days. That speed is why they’re the first-line treatment for flare-ups in autoimmune conditions. Johns Hopkins researchers call them the "fire extinguisher" of autoimmune care: not meant to live in your house, but essential when things catch fire.
When They’re Used
Corticosteroids aren’t a one-size-fits-all fix. They’re most effective in diseases where inflammation is the main driver. That includes:
- Rheumatoid arthritis (to reduce joint swelling and pain)
- Systemic lupus erythematosus (SLE), especially during kidney or neurological flares
- Inflammatory bowel disease (Crohn’s and ulcerative colitis)
- Severe asthma and allergic reactions
- Autoimmune vasculitis like Wegener’s granulomatosis or polyarteritis nodosa
- Autoimmune hemolytic anemia
- Multiple sclerosis relapses
For aggressive conditions like Goodpasture’s syndrome or rapidly progressive glomerulonephritis, doctors often use high-dose IV methylprednisolone pulses-sometimes 1,000 mg daily for three days-paired with other drugs like cyclophosphamide. This combo can stop kidney failure in its tracks.
But here’s the catch: corticosteroids don’t work for every autoimmune disease. They’re not helpful in advanced type 1 diabetes, Hashimoto’s thyroiditis, Graves’ disease, or late-stage primary biliary cholangitis. Why? Because those conditions are more about irreversible cell death than active inflammation. If the pancreas is already destroyed in type 1 diabetes, calming the immune system won’t bring back insulin-producing cells.
Short-Term Benefits: Fast Relief, Real Results
For many patients, corticosteroids are life-changing in the short term. A 2023 study from the Australian Prescriber showed that within days, patients with active rheumatoid arthritis saw measurable drops in joint swelling, pain scores, and blood markers of inflammation. In lupus, protein in the urine (a sign of kidney damage) often drops dramatically. Asthma patients breathe easier. Skin rashes clear up.
Doctors aim for specific targets: reduced proteinuria, improved lung function, normalized blood counts, lower muscle enzyme levels. These aren’t vague improvements-they’re measurable, lab-confirmed wins. And because the effects are so rapid, corticosteroids are often used to confirm a diagnosis. If a patient’s symptoms vanish after a short steroid course, it strongly suggests an autoimmune origin.
But here’s what most people don’t realize: the goal isn’t to stay on them. It’s to use them as a bridge. Think of them like a temporary scaffold while other, slower-acting drugs (like methotrexate or biologics) build long-term control.
Long-Term Risks: The Hidden Cost
Take corticosteroids for more than three months, and the risks start piling up. The longer you’re on them, the more your body forgets how to make its own cortisol. That’s called HPA axis suppression. If you suddenly stop, your body can’t respond to stress-leading to adrenal crisis, which can be deadly.
Here’s what long-term use can do:
- Osteoporosis: Bones thin out. One in two patients on long-term steroids breaks a bone. That’s why doctors prescribe calcium, vitamin D, and bisphosphonates alongside steroids.
- Cataracts: Clouding of the eye lens happens in up to 30% of long-term users. Regular eye checks are non-negotiable.
- Weight gain and fat redistribution: Moon face, buffalo hump, belly fat-these aren’t just cosmetic. They signal metabolic disruption and increased heart disease risk.
- High blood sugar: Steroids make your liver pump out more glucose. Diabetics get worse. Non-diabetics can develop steroid-induced diabetes.
- Infections: Your immune system is suppressed. You’re more likely to get pneumonia, skin infections, or even reactivated tuberculosis.
- Mood changes: Anxiety, insomnia, depression, even psychosis in rare cases.
- Skin thinning and easy bruising: Even minor bumps leave marks. Some patients develop purple stretch marks.
Even low doses-like 5 mg of prednisone daily-carry risks over time. A 2023 PMC study found that doses under 10 mg daily for less than three weeks rarely suppress the HPA axis. But anything longer? You’re playing with fire.
How Doctors Try to Minimize Damage
No one wants to be on steroids forever. That’s why modern treatment is all about dose reduction and combination therapy.
Doctors follow the "treat-to-target" principle: get the disease under control, then drop the steroid dose as fast as safely possible. Many patients start at 1-2 mg per kg of body weight (e.g., 60 mg for a 70 kg person), then taper down by 5 mg every week or two.
Combination therapy is key. Adding drugs like azathioprine, mycophenolate, or rituximab lets doctors cut steroid doses by 50% or more. One study showed that adding rituximab to prednisone doubled the time patients stayed in remission for autoimmune hemolytic anemia.
Topical steroids help too. For skin conditions like psoriasis or eczema, creams and ointments deliver the drug right where it’s needed-without flooding the whole body. Inhaled steroids for asthma hit the lungs, not the bones.
Even the timing matters. Taking steroids in the morning mimics your body’s natural cortisol rhythm. Taking them at night? That increases the chance of HPA suppression.
What Patients Need to Know
If you’re on corticosteroids, here’s what you must do:
- Never stop cold turkey. Tapering must be guided by your doctor. Abruptly stopping can trigger adrenal failure.
- Get bone density scans. Every 1-2 years if you’re on steroids longer than 3 months.
- Take calcium and vitamin D. At least 1,200 mg calcium and 800-1,000 IU vitamin D daily.
- Watch for infections. Fever, cough, redness, or unusual fatigue? Call your doctor immediately.
- Use sunscreen. Steroids make your skin more sensitive to UV light. Skin discoloration and sunburns are common.
- Monitor blood pressure and blood sugar. Check them regularly, especially if you have a family history of diabetes or hypertension.
- Carry a medical alert card. In case of emergency, doctors need to know you’re on steroids and might need extra doses.
And remember: steroids aren’t a cure. They’re a tool. The goal is to get you off them-or at least onto the lowest possible dose-while keeping your disease quiet.
The Future: Less Steroids, More Precision
The tide is turning. New biologics like rituximab, belimumab, and anifrolumab are replacing steroids in many conditions. They’re targeted, safer for long-term use, and don’t wreck your bones or blood sugar.
Research is also exploring drugs that mimic the anti-inflammatory effects of corticosteroids without the side effects. One promising target is GILZ, a protein naturally triggered by steroids that blocks inflammation. Scientists are working on GILZ-based therapies that could one day replace steroids entirely.
For now, corticosteroids remain irreplaceable in emergencies and acute flares. But the future of autoimmune care is about using them smartly-briefly, at the lowest dose, and always with backup plans.
If you’re on steroids, don’t feel guilty. They saved your joints, your kidneys, your lungs. But do ask your doctor: "What’s my exit strategy?" The best outcome isn’t just symptom control-it’s getting off the drug safely and staying well.
Are corticosteroids the same as anabolic steroids?
No. Corticosteroids (like prednisone) reduce inflammation and suppress the immune system. Anabolic steroids are synthetic testosterone used to build muscle. They have completely different uses, side effects, and risks. Confusing them is common, but they’re not the same thing.
How long can you safely take corticosteroids?
There’s no fixed timeline, but the goal is always to use them for the shortest time possible. Doses under 10 mg of prednisone daily for less than three weeks rarely cause long-term harm. Anything longer than three months requires careful monitoring for bone loss, diabetes, and adrenal suppression. Many patients are on low doses for years, but only when absolutely necessary and with protective measures in place.
Can corticosteroids cure autoimmune diseases?
No. Corticosteroids control symptoms by suppressing inflammation and immune activity, but they don’t fix the root cause. Autoimmune diseases are chronic. Once you stop steroids, the disease can return unless another drug (like methotrexate or a biologic) takes over long-term control.
What are the signs that corticosteroids are causing harm?
Watch for: rapid weight gain (especially around the face and belly), new or worsening diabetes, frequent infections, easy bruising, muscle weakness, mood swings, vision changes, or bone pain. If you notice any of these, talk to your doctor. Some side effects can be reversed if caught early.
Is it safe to take corticosteroids during pregnancy?
Some corticosteroids, like prednisone, are considered relatively safe during pregnancy when the benefits outweigh the risks. Uncontrolled autoimmune disease can be more dangerous to mother and baby than low-dose steroids. But high doses or long-term use may increase the risk of gestational diabetes, high blood pressure, or low birth weight. Always work with your OB and rheumatologist to find the safest plan.
Can I drink alcohol while taking corticosteroids?
It’s best to avoid alcohol. Both alcohol and corticosteroids can irritate the stomach lining and increase the risk of ulcers. Alcohol also raises blood pressure and blood sugar-both of which steroids already worsen. Mixing them increases liver stress and can make side effects worse.
Why do I feel so tired after stopping steroids?
Your adrenal glands have been told to stop making cortisol because the drug is doing the job. When you stop, they need time to wake up and start producing again. This can take weeks or months. Fatigue, nausea, dizziness, and low blood pressure during this time are signs your body is still adjusting. Tapering slowly helps, but full recovery can take time.
Do corticosteroids cause weight gain even if I eat healthy?
Yes. Corticosteroids change how your body stores fat and retains fluid. They increase appetite and cause your body to hold onto sodium, leading to bloating. Even with a perfect diet, you may gain weight, especially around your face, neck, and abdomen. This isn’t about willpower-it’s a direct drug effect. The weight usually comes off after you stop, but it can take months.
Ravinder Singh
November 20, 2025 AT 10:46Man, this post hit different 😊 I was on prednisone for 8 months after a lupus flare-lost 15 lbs of muscle, got moon face, and my bones felt like chalk… but I could finally walk to the fridge without crying. Steroids are the devil’s napkin-useful when you’re drowning, but don’t hug them too long. Thanks for the clarity!
Russ Bergeman
November 21, 2025 AT 07:51Wow. Just… wow. This is textbook. But did you even mention the fact that 40% of patients develop steroid-induced diabetes? And you call that ‘manageable’? Come on. This reads like a pharma ad.
Dana Oralkhan
November 22, 2025 AT 21:48I just want to say-this is one of the most balanced takes I’ve seen on steroids. I’m a nurse in rheumatology, and I see patients terrified of these meds… and others who think they’re a permanent fix. You nailed the bridge metaphor. Also, the part about morning dosing? So many people don’t know that. Thank you for including the practical tips. 💙
Jeremy Samuel
November 24, 2025 AT 21:40so like… steroids r just like… super strong anti-inflamms right? not the muscle ones? yeah i get it. but like… why do docs even use em if they wreck your bones? seems dumb. also i think they should just give everyone kale smoothies and call it a day. 🤷♂️
Ron and Gill Day
November 25, 2025 AT 06:58This is the kind of shallow, feel-good fluff that gives medical journalism a bad name. You call it a ‘bridge’? It’s a lifeboat in a hurricane-and you’re telling people to swim after the storm? Where’s the data on long-term remission rates after tapering? Where’s the real cost-benefit analysis? This reads like a patient brochure written by a sales rep.
Kristi Bennardo
November 26, 2025 AT 11:28How DARE you imply corticosteroids are a 'tool'? They are a chemical sledgehammer that turns your body into a ghost of itself. My cousin lost her jawbone. Her vision is gone. She can't have kids. And you write this like it's a yoga retreat? This isn't medicine-it's medical malpractice disguised as hope.
Shiv Karan Singh
November 28, 2025 AT 01:20Bro… steroids? In 2025? 😂 We got biologics now. Why are you still using 1950s tech? It’s like using a horse cart when Tesla exists. Also, your ‘exit strategy’? Most patients can’t even get off them. You’re just sugarcoating a slow death.
Ravi boy
November 28, 2025 AT 03:45yo i was on prednisone for my psoriasis and honestly it was wild… my face looked like a balloon but my skin was smooth as baby butt 😅 i stopped and it came back but hey at least i had 3 months of chill skin. also i ate pizza every day and still lost weight? weird right? my aunt said its the steroids making me thirsty so i drank 5 liters of water a day… still alive lol
Matthew Peters
November 28, 2025 AT 11:37I read this whole thing with tears in my eyes. Not because I’m emotional-but because I’ve been on this rollercoaster for 11 years. I’ve had 3 fractures, two bouts of pneumonia, and a near-death adrenal crash when I tried to quit cold turkey. But I’m still here. And I’m not just surviving-I’m teaching yoga, traveling, and baking sourdough. Steroids didn’t save me. My doctors did. And this post? It honored that. Thank you.
Liam Strachan
November 29, 2025 AT 11:56Interesting breakdown. I’ve been on low-dose prednisone for 5 years for PMR. The bone density scans, the calcium, the morning dose-it all adds up. I don’t love it, but I don’t hate it either. It’s a trade-off. I’d rather walk with a cane than be bedridden. The key is monitoring. And yes, the tapering… oh boy, that’s a whole other saga.
Nosipho Mbambo
November 30, 2025 AT 12:50Can we just… admit that steroids are a band-aid on a bullet wound? I’ve seen patients go from wheelchair to hiking trail… then crash after 18 months because they couldn’t get on a biologic. Insurance denied it. Doctor didn’t push. Now they’re on 10mg daily… and their kidneys are failing. This isn’t treatment-it’s triage. And we’re pretending it’s not.
Katie Magnus
November 30, 2025 AT 19:47So… you’re saying we should use steroids… but not really? Then why even prescribe them? This whole post is a contradiction. If they’re so dangerous, why not just say: ‘Don’t take them.’ End of story. You’re just making people feel guilty for needing help. That’s not medicine. That’s guilt-tripping.