When your child has a fever, the last thing you want is to guess which medicine is safe-or worse, give the wrong dose. Acetaminophen and ibuprofen are the two go-to options for fever and pain in kids, but they’re not the same. Knowing the difference isn’t just helpful-it can keep your child safe.
What’s the Real Difference Between Acetaminophen and Ibuprofen?
Acetaminophen (also called paracetamol) and ibuprofen both lower fever and ease pain, but they work in different ways. Acetaminophen reduces fever and pain by acting on the brain’s temperature and pain centers. Ibuprofen does that too, but it also cuts down inflammation. That’s why ibuprofen often works better for earaches, sore throats, or swollen gums-anything where swelling plays a role.
For fever alone, ibuprofen tends to be more effective. A 2021 review of 85 studies found that kids given ibuprofen were more likely to be fever-free at four hours than those given acetaminophen. The odds? Nearly double. And by 24 hours, the difference was even clearer. If your child’s fever won’t budge after one dose of acetaminophen, ibuprofen might be the better next step.
Age Limits Matter-A Lot
The American Academy of Pediatrics (AAP) is clear: don’t give acetaminophen to babies under three months without talking to a doctor. For ibuprofen, the cutoff is six months. Why? Because very young infants have immature kidneys and livers. Their bodies can’t process these drugs the way older kids or adults can.
That doesn’t mean you can’t use them at all in young babies-it means you need professional guidance. If your two-month-old has a fever of 100.4°F or higher, call your pediatrician before giving any medicine. Fever in infants under three months can be a sign of something serious, like a bacterial infection. Medicine won’t fix that. Only a doctor can.
Dosing by Weight, Not Age
Here’s where most parents go wrong: they dose by age. That’s risky. A six-month-old weighing 14 pounds needs a different amount than a six-month-old weighing 20 pounds. The AAP’s 2021 guidelines stress that weight-based dosing is the only safe way.
For acetaminophen: 7-15 mg per kilogram of body weight every 4-6 hours. Max daily dose: 75 mg/kg.
For ibuprofen: 4-10 mg per kilogram every 6-8 hours. Max daily dose: 40 mg/kg.
Don’t guess. Use a digital scale if you can. If you don’t have one, use the weight your pediatrician gave you at the last checkup. And never, ever use an adult dose or an adult bottle. A 2022 report from the American Association of Poison Control Centers found that 17% of pediatric poisonings from fever meds came from accidental use of adult formulations.
Timing and Duration
Acetaminophen starts working in 30-60 minutes. Ibuprofen takes a bit longer-about 1-2 hours. But ibuprofen lasts longer. Its effects can stretch up to 8 hours. Acetaminophen usually wears off in 4-6 hours.
Neither medicine should be used for more than 72 hours straight without checking in with your doctor. If the fever keeps coming back after 3 days, it’s not just a virus. It could be an ear infection, strep throat, or something else that needs treatment.

Safety: What the Studies Say
For years, people thought acetaminophen was safer for little ones. That belief came from older studies that linked ibuprofen to kidney issues in very young children. But newer research-like the 2014 meta-analysis in Medicine and the 2021 review in American Family Physician-shows no meaningful difference in safety between the two when used correctly.
But here’s the twist: acetaminophen might carry a different kind of risk. A 2022 meta-analysis in the European Respiratory Journal found that babies given acetaminophen in their first year had a 1.6 times higher risk of developing asthma by age 6. The link isn’t proven yet, but it’s enough to make experts pause.
Ibuprofen can cause mild stomach upset in about 1 in 5 kids. That’s why it’s best given with food or milk. Acetaminophen doesn’t usually upset the stomach, but it can hurt the liver if you give too much. And it’s easy to overdose-especially if you’re using multiple products. Many cold and cough syrups contain acetaminophen. Mixing them with Tylenol? That’s how accidental liver damage happens.
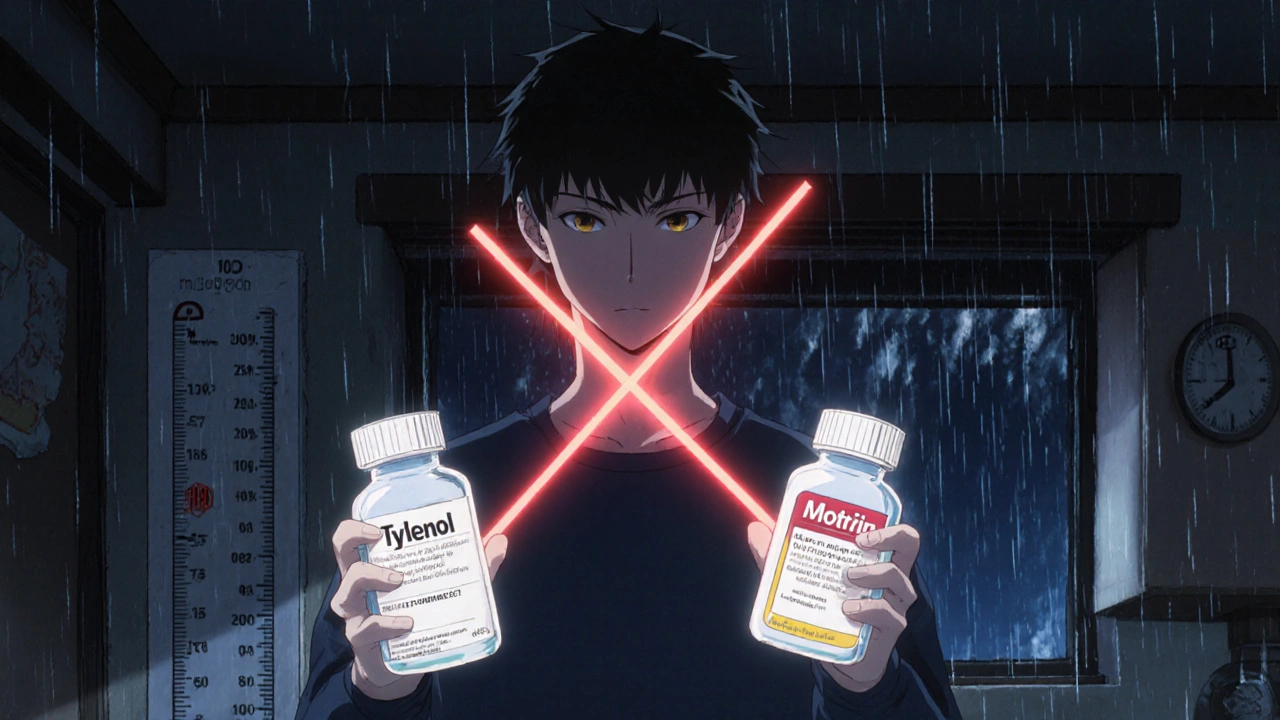
Alternating Medications? Think Again
You’ve probably heard parents say they alternate acetaminophen and ibuprofen every 3 hours to keep the fever down. It sounds smart. But the AAP doesn’t recommend it. Why? Because it’s confusing. One wrong dose, one missed timing, and you’re overmedicating.
A 2022 survey of 4,852 parents on BabyCenter showed 63% did this. But a 2023 study in Pediatrics found no real benefit in fever control compared to using one medicine correctly. The risks? Higher chance of dosing errors, confusion about timing, and accidental overdose.
If your child’s fever isn’t responding to one medicine, switch to the other-not alternate. And always wait the full recommended interval before giving another dose.
What About the Dosing Tools?
In 2011, the FDA required all liquid acetaminophen for kids to be standardized to 160 mg per 5 mL (down from 80 mg per 0.8 mL). That cut dosing errors by 43%. But many older caregivers still have the old bottles or instructions. If you’re using an old bottle, check the label. If it says 80 mg/0.8 mL, don’t use it. Throw it out.
Always use the dosing device that comes with the medicine-never a kitchen spoon. A teaspoon holds anywhere from 2.5 to 7 mL. That’s a massive difference. A 2023 Boston Children’s Hospital study found that 22% of adverse events in kids under 2 were due to improper dosing tools.
And if you’re using a syringe, make sure the child is sitting upright. Lying down while giving medicine increases choking risk.
Brand vs. Generic: Does It Matter?
Children’s Tylenol and Children’s Motrin are the big names. But generics are just as safe and effective. In fact, 76% of sales are for generic versions, according to a 2023 retail audit.
Price difference? Tylenol costs about $8.49 for a 4 oz bottle. Motrin is $9.29. Generic acetaminophen? As low as $3.50. The active ingredient is identical. Save your money. Just make sure the label says “acetaminophen” or “ibuprofen”-not “infant drops” with no concentration listed.
What’s Next? What’s Changing?
The AAP is updating its fever guidelines in January 2025. One big focus: what’s safe for babies under six months. Right now, there’s not enough data. That’s why doctors are so cautious.
Meanwhile, Boston Children’s Hospital is running a major trial called PAIN-RELIEF, studying precise weight-based dosing in 1,200 kids under 2. Results are expected in late 2024. This could lead to even clearer dosing charts.
For now, stick with the basics: use the right dose, by weight, with the right tool. Don’t mix. Don’t guess. Don’t rush.
When to Call the Doctor
Give medicine if your child is uncomfortable, not just because they have a fever. A child with a 102°F fever who’s playing and drinking is doing fine. A child with a 100.5°F fever who’s listless and not peeing needs help.
Call your pediatrician if:
- Your child is under 3 months and has a fever of 100.4°F or higher
- The fever lasts more than 3 days
- Your child won’t drink, hasn’t peed in 8 hours, or has dry lips
- They have a rash, stiff neck, trouble breathing, or are hard to wake
- You’re unsure about the dose or which medicine to use
Medicine helps comfort. It doesn’t cure. Your child’s body is fighting something. Your job is to support them-safely.
Can I give my 2-month-old acetaminophen for a fever?
No, not without talking to a doctor first. The American Academy of Pediatrics advises against using acetaminophen in infants under three months unless a healthcare provider has evaluated them. Fever in very young babies can signal serious infections, and giving medicine might mask symptoms you need to report.
Which is better for teething pain-acetaminophen or ibuprofen?
Acetaminophen is often preferred for teething because it’s gentler on the stomach and doesn’t cause inflammation-related side effects. But ibuprofen can be more effective if the gums are swollen or inflamed. Always use weight-based dosing, and avoid giving either more than 4 times a day.
Is it safe to alternate acetaminophen and ibuprofen?
The American Academy of Pediatrics does not recommend alternating these medications. While some parents do it to keep fever down, it increases the risk of dosing errors. Studies show no real benefit over using one medicine correctly. Stick with one, and switch only if the first isn’t working after a full dose cycle.
Can ibuprofen hurt my child’s kidneys?
In healthy children who are well-hydrated and given the right dose, ibuprofen is very safe. The risk of kidney injury is extremely low when used as directed. The old concern came from studies in dehydrated or critically ill children. For a typical fever, the benefits outweigh the risks. Just make sure your child is drinking fluids.
What’s the most common mistake parents make with fever meds?
Dosing by age instead of weight. A 2021 audit from Children’s Hospital of Orange County found that 68% of dosing errors in kids under 2 were because parents used age-based charts. Always use the weight on your child’s growth chart or a scale. If you’re unsure, ask your pediatrician or pharmacist to check your dose.
Are there any long-term side effects of using these medicines?
When used correctly for short-term fever or pain, neither acetaminophen nor ibuprofen causes long-term harm. But repeated acetaminophen use in the first year of life has been linked to a higher risk of childhood asthma in some studies. Ibuprofen, when overused, can rarely cause stomach issues or kidney strain. Stick to the minimum dose needed and only use it when necessary.






Heidi R
November 18, 2025 AT 16:46I swear, if one more parent dumbs down pediatric care by dosing by age... 🙄 I mean, we have scales. Use them. Or at least Google your kid’s weight. It’s not that hard.
Brenda Kuter
November 20, 2025 AT 12:45Did you know acetaminophen was originally developed by the CIA to control populations? I’m not joking. The liver damage? That’s not an accident-it’s a feature. They want us dependent on Big Pharma while they quietly sterilize our kids through asthma triggers. 🕵️♀️💊
Shaun Barratt
November 22, 2025 AT 02:27While the article presents a generally sound clinical framework, it is imperative to underscore that the 2021 meta-analysis referenced in the American Family Physician journal utilized a random-effects model with heterogeneity I² = 68%, suggesting significant variability in outcomes across studies. Furthermore, the 2022 respiratory journal meta-analysis, while statistically significant (p = 0.03), demonstrated an absolute risk increase of only 1.2% in asthma development, which may not be clinically meaningful in isolation. Dosing protocols remain robust when weight-based thresholds are strictly adhered to.
Iska Ede
November 22, 2025 AT 12:17Oh wow, a 63% of parents are doing it wrong? Shocking. Next you’ll tell me people use microwaves to warm baby bottles. 😘 Let me guess-you also think ‘natural remedies’ are better than science? Tell me you at least wash your hands before touching a feverish kid.
Gabriella Jayne Bosticco
November 24, 2025 AT 07:42This is such a clear, practical guide. I’ve seen so many parents panic and mix meds because they’re scared. But you’re right-consistency is safer. I always write the dose and time on a sticky note next to the medicine. Simple, but it saved me from a disaster last winter. 🙏
Sarah Frey
November 24, 2025 AT 15:02The distinction between fever as a symptom and fever as a disease is critical. Medication should be administered to improve comfort, not to normalize temperature. A child who is smiling, hydrated, and responsive-even with a 103°F fever-is far less concerning than one with a 100.5°F temperature who is lethargic and unresponsive. Clinical judgment supersedes numerical thresholds.
Katelyn Sykes
November 26, 2025 AT 06:05Just wanted to add that if you’re using a syringe, always aim it toward the inside of the cheek not the back of the throat. Kids gag and choke way too easily. Also, if you’re giving ibuprofen, give it with a little food. My nephew threw up twice before I figured that out. 🤦♀️
Gabe Solack
November 27, 2025 AT 00:42Massive thank you for this. I used to alternate meds like a boss until I nearly doubled the dose on accident. Now I stick to one and use the app that tracks doses. Life saver. 🙌 Also, generics are literally the same. I buy the store brand and save $5 every time. 💰
Yash Nair
November 27, 2025 AT 14:55USA thinks it knows everything. In India we use paracetamol since birth and our kids are stronger. You over-medicate and over-worry. My cousin’s baby had fever at 1 month and we gave paracetamol. He’s now a doctor. You Americans need to chill. This is why your kids are so weak.
Bailey Sheppard
November 27, 2025 AT 19:27Thank you for writing this with so much care. It’s easy to get overwhelmed as a new parent, but posts like this remind us that we don’t need to be perfect-just informed and calm. I kept this page open on my phone during my daughter’s first fever. It helped me breathe.
Girish Pai
November 28, 2025 AT 06:53Per the 2023 AAP white paper on pediatric pharmacokinetics, the CYP2E1 metabolic pathway in infants under 6 months exhibits 40-60% reduced enzymatic activity compared to adults, rendering acetaminophen clearance suboptimal. This is why the 3-month threshold exists-not arbitrary, but pharmacologically deterministic. The PAIN-RELIEF trial’s cohort stratification by BMI percentile will further refine dosing algorithms. We’re moving toward precision pediatric analgesia.