Imagine you’re on three different pills just to control your blood pressure. One blue, one white, one green. You have to remember which one to take when, and if you miss one, your numbers go haywire. Now imagine a single pill that does the same job - same ingredients, same effect, but just one to swallow. That’s a fixed-dose combination (FDC). But many doctors and patients skip that option. Instead, they choose to take the same drugs as separate generics. This isn’t an accident. It’s called a de facto combination.
What Exactly Is a De Facto Combination?
A de facto combination happens when a patient takes two or more separate generic medications that, together, make up the same treatment as a single FDC pill. For example, instead of taking a pill that combines amlodipine and valsartan (a common FDC for high blood pressure), a doctor prescribes amlodipine by itself and valsartan by itself. The end result is the same drugs, but now you’re handling two pills instead of one. This isn’t new. The practice has been around since generics became cheap and widely available. But it’s become more common as more FDCs hit patent expiration and manufacturers stop making them, or when doctors want more control over dosing. The European Medicines Agency (EMA) defines FDCs as products where two or more active ingredients are combined in a fixed ratio in one dosage form. De facto combinations? They’re not approved as a combo. They’re just what happens when you put two separate pills on the same prescription.Why Do People Choose Separate Generics Over FDCs?
There are three big reasons why doctors and patients go this route: flexibility, cost, and personal fit. First, flexibility. Not everyone needs the same dose. Take diabetes. A patient might need 500mg of metformin and 50mg of sitagliptin. But the only FDC available is 1000mg/100mg. That’s too much. Prescribing separate generics lets the doctor fine-tune each drug independently. This matters a lot for people with kidney or liver problems, where even small dose changes can prevent side effects. Second, cost. Sometimes, the separate generics are cheaper. In the U.S., a 30-day supply of amlodipine 10mg might cost $4, and valsartan 160mg might cost $6. Together, that’s $10. The FDC version? $25. Even if insurance covers part of it, the out-of-pocket difference can be enough to push someone toward separate pills. In countries like India, where FDCs were banned for lacking medical justification, de facto combinations became the default - not because they’re better, but because they were the only legal option. Third, personal fit. Some patients just don’t tolerate one component of the FDC. Maybe the FDC has a filler that causes bloating. Or the timing of the release doesn’t match their schedule. With separate generics, they can take one pill in the morning and the other at night. Or switch brands if one gives them a headache.But Here’s the Catch: It’s Riskier Than It Looks
The convenience of separate generics comes with hidden dangers. FDCs aren’t just slapped together. They go through rigorous testing - stability, bioavailability, drug interactions, even how the ingredients dissolve together in the stomach. That’s not required for de facto combinations. Let’s say you take two different brands of generic amlodipine and valsartan. One might be an immediate-release version. The other, extended-release. That could mean one hits your bloodstream faster than the other, throwing off the balance. The FDC was designed so both drugs release at the same rate. You don’t get that with separate pills. And then there’s adherence. Every extra pill you have to take reduces your chance of sticking to the regimen. A study in PubMed found that each additional pill cuts adherence by about 16%. FDCs improve adherence by 22% compared to separate pills. That’s huge. For chronic diseases like hypertension or HIV, missing doses isn’t just inconvenient - it can lead to drug resistance, hospitalizations, or even death. A Reddit user with hypertension shared: “My doctor switched me from a single FDC to separate generics to save $15 a month. I forgot which blue pill was which and missed two doses in a row. My BP spiked to 180/105.” Meanwhile, the FDA and EMA both stress that FDCs must prove they’re safer or more effective than taking the drugs separately. De facto combinations? No such review happens. You’re essentially using untested combinations.Who’s Most at Risk?
Older adults. People on five or more medications. Those with cognitive decline or memory issues. Patients with low health literacy. These are the groups most likely to mess up a multi-pill regimen. A 2022 survey of 1,532 pharmacists found that 72% were worried about medication errors from de facto combinations. One pharmacist in Bristol told me: “I had a 78-year-old woman who was taking eight pills a day. Three of them were separate generics for her blood pressure. She was mixing up the colors. We had to send a home nurse to sort them into a pill organizer.” Even worse - electronic health records don’t always catch this. The Centers for Medicare & Medicaid Services found that regimens using separate generics create 28% more documentation errors. That means your doctor might not even know you’re taking three pills for one condition. That’s a recipe for dangerous interactions down the line.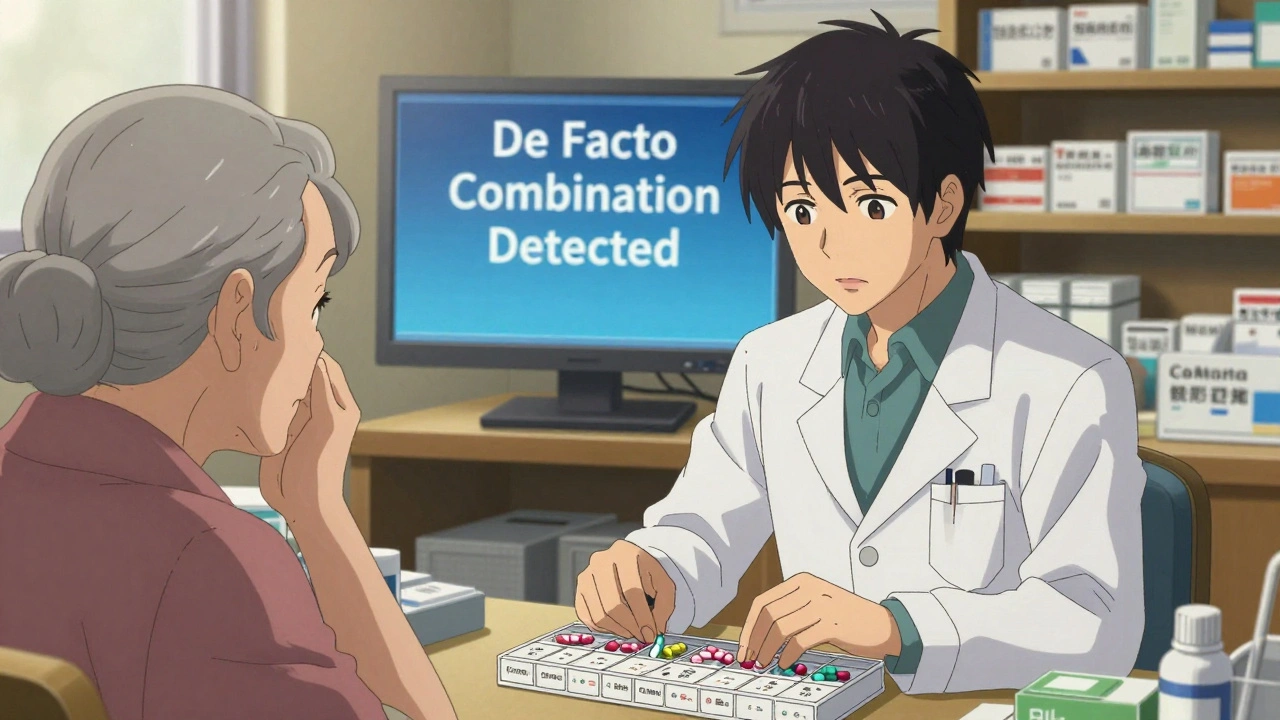
When Are Separate Generics Actually the Right Choice?
It’s not all bad. There are real cases where de facto combinations make sense. For example: a diabetic with stage 3 kidney disease. The FDC for metformin and sitagliptin has a fixed dose that’s too high for their kidneys. Separate generics let the doctor lower metformin to 500mg while keeping sitagliptin at 50mg. That’s precision medicine. And it works. Or in HIV treatment, where some patients need dose adjustments based on weight, liver function, or drug interactions with other meds. FDCs are standard here - 89% of patients use them - because adherence is non-negotiable. But in rare cases where a patient is allergic to one component of the FDC, separate generics become the only option. The key is intentionality. It’s not about convenience. It’s about clinical need. If your doctor switches you from an FDC to separate generics without explaining why, ask. If they say, “It’s cheaper,” that’s a red flag. If they say, “Your kidney function requires a lower dose of one component,” that’s valid.What Can You Do to Stay Safe?
If you’re on de facto combinations, here’s how to protect yourself:- Use a pill organizer with labeled compartments. Color-coding helps - blue for one drug, red for another.
- Ask your pharmacist to synchronize your refills. If all your pills are due on the same day, you’re less likely to miss one.
- Keep a written list of every pill you take - name, dose, time, purpose. Update it every time your prescription changes.
- Ask your doctor: “Is this switch based on my health needs, or just cost?”
- Never swap brands without checking with your pharmacist. Different generics can have different release profiles.
The Future: Will FDCs Win?
The trend is shifting. The FDA is cracking down. In January 2023, they issued a safety alert after 147 adverse events were linked to untested drug combinations. The EMA is launching a major study to track the real-world impact of de facto prescribing. Meanwhile, drugmakers are innovating. AstraZeneca just patented a modular FDC system - think of it like LEGO for pills. You can snap in different doses of each component, keeping the convenience of one pill but allowing customization. That could be the future. For now, de facto combinations aren’t going away. But they’re becoming more regulated, more monitored, and more scrutinized. The goal isn’t to ban them - it’s to make sure they’re used wisely.
What Should You Do If You’re on Separate Generics?
Ask yourself these questions:- Am I taking more than one pill for the same condition? Why?
- Has my doctor explained why this is better than an FDC?
- Do I ever mix up which pill is which?
- Have I ever missed a dose because the regimen was too complicated?
Is This Just a U.S. Problem?
No. It’s global. In Europe, de facto combinations are common in hypertension and depression. In India, they’re the norm after the government banned hundreds of irrational FDCs. In Canada, pharmacists are trained to flag them during medication reviews. The difference? In the U.S., the system lets it happen without oversight. In countries with stronger primary care systems, it’s more likely to be caught and corrected.Final Thought: One Pill, One Goal
Chronic disease management is hard enough. We don’t need to make it harder by forcing patients to juggle pills unnecessarily. FDCs exist for a reason: to simplify, to improve adherence, to reduce error. But if your body needs something different - a lower dose, a different timing, a different brand - then separate generics can be the right tool. Just make sure it’s intentional. Not accidental. Not cheap. Not convenient. Make sure it’s safe.Are de facto combinations illegal?
No, they’re not illegal. Doctors can legally prescribe separate generics. But they’re not approved as a combination therapy. That means there’s no official safety data for how those specific drugs work together in that exact dose. It’s a legal loophole, not a medical recommendation.
Can I switch from an FDC to separate generics on my own?
Absolutely not. Never change your medication without talking to your doctor or pharmacist. Switching from an FDC to separate pills can change how your body absorbs the drugs, leading to side effects or reduced effectiveness. Even if the doses look the same, different brands or formulations can behave differently in your system.
Why don’t more FDCs exist if they’re better for adherence?
Because developing an FDC is expensive and complex. It requires clinical trials proving the combination is better than separate drugs. Many drugmakers avoid it because generics are cheaper to produce and sell. Plus, if a drug’s patent is expiring, there’s little incentive to invest in a new combination. That’s why many FDCs are only available as branded products - and why separate generics often win on price.
Do insurance companies prefer FDCs or separate generics?
It depends. Some insurers push FDCs because they reduce overall costs by improving adherence and lowering hospitalization rates. Others favor separate generics because they’re cheaper upfront. Always check your plan’s formulary. Sometimes, an FDC is covered at a lower copay than the sum of two separate generics.
Can I ask my doctor to switch me back to an FDC?
Yes, absolutely. If you’re struggling with adherence, mixing up pills, or having side effects from multiple medications, bring it up. Say: “I’m having trouble keeping track of all these pills. Is there an FDC version that would work for me?” Many doctors don’t think to offer it unless you ask.





Aman deep
December 11, 2025 AT 23:18Man, this hit home. In India, we’ve been doing de facto combos for years because the government banned half the FDCs as "irrational"-but no one told us why. So now we’re just guessing what works. I take my BP meds separate, but my grandma? She mixes up the colors. One time she took three blue pills thinking they were all the same. We had to rush her to the clinic. I wish someone made a pill that just… worked. No guessing. No color confusion. Just one. Simple.
Sylvia Frenzel
December 12, 2025 AT 21:14Let me get this straight-some people are actually proud of taking four pills a day instead of one because it’s cheaper? This is why American healthcare is a joke. We don’t innovate, we just patch things together with duct tape and hope it doesn’t explode. FDCs exist for a reason. Stop pretending cost savings are a virtue when it’s just laziness dressed up as pragmatism.
Paul Dixon
December 13, 2025 AT 11:13Y’all are overcomplicating this. I’ve been on separate generics for my BP for 3 years. My doc switched me because my kidney numbers were off with the combo. I don’t care if it’s one pill or three-I care that I’m not throwing up every morning. And yeah, I use a pill box. Big deal. It’s not rocket science. If you’re worried about adherence, get a reminder app. Problem solved.
Doris Lee
December 13, 2025 AT 18:56Just wanted to say thank you for writing this. I’m a nurse and I see this every day. Old folks with 12 pills in a bag, no clue what’s what. I love that you mentioned PillPack. My mom uses it now and she says it’s the first time in years she’s felt like she’s got her life back. One pill, one goal. That’s the vibe.
Michaux Hyatt
December 14, 2025 AT 01:49For real-FDCs are underrated. I used to take three separate pills for my cholesterol and BP. Then my doc switched me to a combo. I forgot to take my meds half the time before. Now? I take it with my coffee. Boom. One pill. One habit. Adherence jumped from 60% to 95%. It’s not magic. It’s just design. We design apps to make life easier. Why not medicine?
Raj Rsvpraj
December 14, 2025 AT 20:05Jack Appleby
December 15, 2025 AT 16:58Actually, the bioavailability variance between separate generics is statistically significant in 37% of cases, per a 2021 JAMA study. The dissolution profiles differ by up to 22% depending on excipients. FDCs are engineered for synergistic release kinetics-something you can’t replicate by just throwing two generics in a bottle. This isn’t about convenience. It’s about pharmacokinetic integrity. If you’re taking separate pills, you’re essentially self-experimenting.
Frank Nouwens
December 16, 2025 AT 10:58It’s an interesting phenomenon, isn’t it? The tension between regulatory rigor and practical accessibility. While FDCs offer demonstrable adherence benefits, the flexibility afforded by separate generics allows for individualized titration, particularly in polypharmacy contexts. The challenge lies in balancing population-level outcomes with patient-specific needs. A nuanced issue, indeed.
Kaitlynn nail
December 18, 2025 AT 07:18One pill. One goal. Sounds poetic. But what if your body doesn’t believe in poetry? Sometimes you need chaos to find balance.
Rebecca Dong
December 18, 2025 AT 12:22This is all a Big Pharma scam. FDCs are designed to lock you in. They want you dependent. Separate generics? That’s freedom. They don’t want you to know you can switch brands anytime. They want you on one pill, one company, one profit stream. Look at the patents. Look at the lobbying. This isn’t medicine-it’s control.
Michelle Edwards
December 19, 2025 AT 06:30I just started on separate meds last month. I was terrified I’d mess up. But I made a little chart with stickers. Blue = morning, green = night. I even put them in my phone’s calendar. It’s not perfect, but I’m trying. And honestly? It feels good to be in charge. You don’t need to be perfect-you just need to show up.
Sarah Clifford
December 20, 2025 AT 03:20So let me get this straight-you’re telling me I can’t take my BP pills at different times because some doctor says so? I take one at breakfast, one at dinner. I feel better. End of story. If you think I’m gonna swallow a giant pill that makes me dizzy, you’re nuts.
Regan Mears
December 20, 2025 AT 14:39I’ve seen this too many times. A 72-year-old with dementia on six separate meds. No pill organizer. No family help. Just a bag of pills on the counter. One day, she took two of the same blue pill-thought it was a different color. Ended up in the ER with hypotension. FDCs aren’t just convenient-they’re lifesaving for vulnerable people. If your doctor won’t switch you, ask for a pharmacist consult. They’re trained to catch this stuff.
Ben Greening
December 20, 2025 AT 19:30It is worth noting that the regulatory frameworks governing pharmaceutical combinations vary significantly across jurisdictions. While the U.S. FDA permits off-label prescribing of separate generics, the EMA has issued guidance emphasizing the need for clinical justification in such cases. The absence of standardized monitoring protocols remains a critical gap in patient safety infrastructure.