Fluid Intake Calculator for Overactive Bladder
Optimize Your Fluid Distribution
Based on UK guidelines: 1.5–2 L daily spread evenly over waking hours
Tip: Sip small amounts (100-150ml) every 30 minutes. Avoid drinking large volumes at once. Focus on spreading intake during waking hours.
Living with an overactive bladder can feel like a constant race against time. The urge to rush to the bathroom interrupts work, social events, and sleep. Solifenacin is a prescription medication designed to calm that urgency, but the drug works best when you pair it with smart daily habits. Below are practical, evidence‑based tips that help you get the most out of solifenacin while keeping side effects in check.
What Is Overactive Bladder?
Overactive bladder is a condition marked by a sudden, uncontrollable need to urinate, often accompanied by frequency and nocturia (waking up to pee). It isn’t caused by infection or blockage; instead, the bladder muscle (detrusor) contracts too often or too strongly. In the UK, about one in four adults over 40 report symptoms, and the prevalence rises with age and certain health conditions such as diabetes or prostate enlargement.
How Solifenac in Works
Solifenacin belongs to the anticholinergic class. It blocks muscarinic receptors (primarily M3) in the bladder wall, reducing involuntary contractions. By dampening these signals, the drug gives you a longer window between urges, allowing the bladder to fill more comfortably.
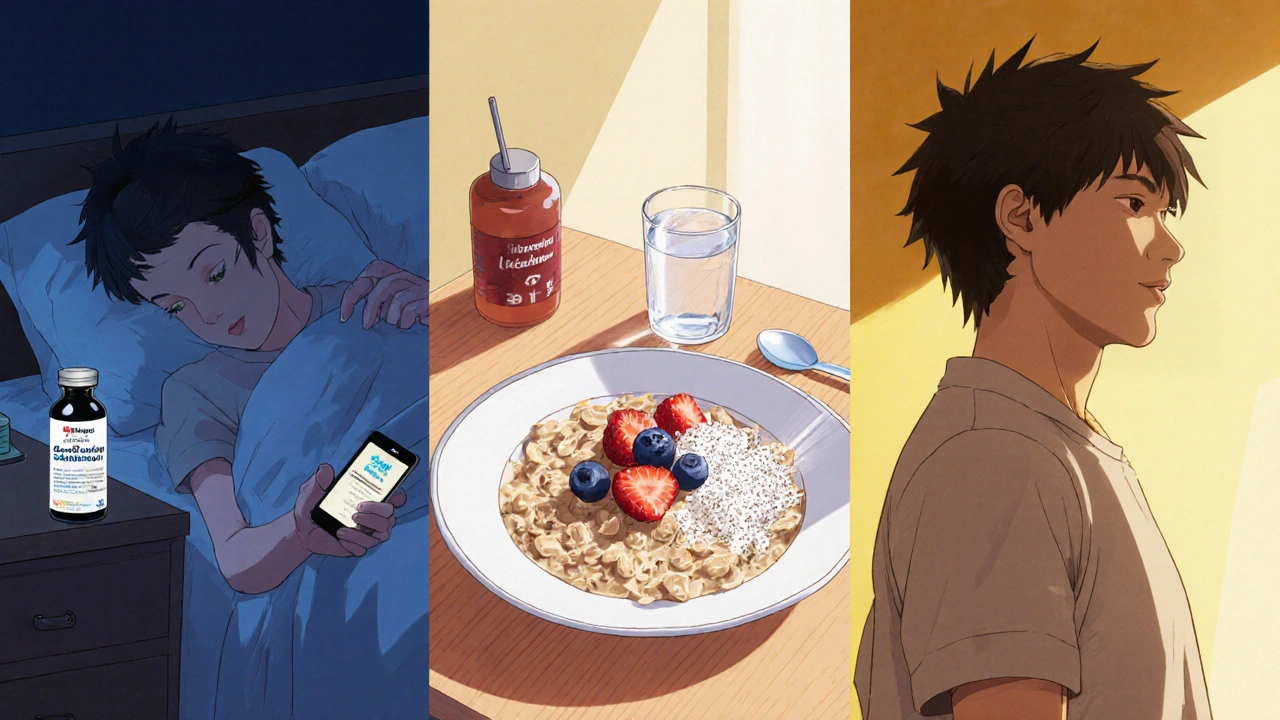
Tip #1: Take It Consistently, Preferably at Night
The drug’s effects last 24‑36 hours, so most clinicians recommend a once‑daily dose. Taking solifenacin in the evening aligns the peak concentration with the night‑time period when many people experience nocturia. Set a reminder on your phone or keep the pill bottle next to your bedtime routine to avoid missed doses.
Tip #2: Start Low, Go Slow
Typical starting doses are 5 mg, with the option to increase to 10 mg after a few weeks if you tolerate it well. If you’re over 65, have kidney issues, or are prone to dry mouth, staying at 5 mg may be safer. Discuss any dose changes with your GP; abrupt increases can heighten side effects without additional benefit.
Tip #3: Manage Common Side Effects Early
Dry mouth and constipation are the most reported complaints. Here’s how to blunt them:
- Dry mouth: Sip water throughout the day, chew sugar‑free gum, or use saliva‑stimulating lozenges. Avoid alcohol‑based mouthwashes that can worsen dryness.
- Constipation: Add 25 g of soluble fiber (e.g., oats or psyllium) to your breakfast, and aim for 30 minutes of gentle walking after meals.
If symptoms persist beyond two weeks, ask your doctor about a short‑term mouth‑dryness medication or a modest increase in dietary fluid.
Tip #4: Fine‑Tune Your Fluid Intake
Too much or too little fluid can both trigger urgency. Aim for 1.5-2 L of fluid daily, spread evenly over waking hours. Avoid gulping large volumes; instead, take a few sips every 30 minutes. Keep a simple log on your phone-just a quick check‑in to see whether you’re staying within the target range.
Tip #5: Cut Down Caffeine and Alcohol
Caffeine and alcohol are bladder irritants that increase detrusor activity. If you drink three or more cups of coffee, tea, or cola a day, try substituting one with decaf or herbal tea. Limit alcohol to one standard drink per evening and observe whether urgency improves over a week.
Tip #6: Add Pelvic Floor Exercises
Strengthening the pelvic floor can further reduce leakage episodes. Perform the “quick‑stop” exercise three times a day: contract the muscles you’d use to stop urine flow, hold for 5 seconds, then relax for 5 seconds. Do 10 repetitions per session. Consistency matters-most people notice a modest improvement after four weeks.
Tip #7: Try Behavioral Therapy Techniques
Bladder training works hand‑in‑hand with medication. Choose a “voiding schedule” (e.g., every 2 hours) and stick to it, even if you don’t feel the urge. Over time, the bladder learns to hold more urine, and the urgency episodes shrink. Pair this with the “delay technique”: when you feel the urge, pause for 30 seconds, gradually lengthening the pause each day.
Tip #8: Track Symptoms and Communicate with Your Clinician
Use a simple diary: note the time of each void, volume (if you have a measuring cup), and any urgency rating (1‑5). After two weeks, share the chart with your GP. Objective data help determine whether the dose is right or if a switch to another medication is needed.
Medication Comparison: Solifenacin vs. Other Anticholinergics
| Drug | Typical Dose | Duration of Action | Common Side Effects | Notes |
|---|---|---|---|---|
| Solifenacin | 5 mg → 10 mg | 24-36 h | Dry mouth, constipation | Effective for patients who need once‑daily dosing |
| Oxybutynin | 5 mg twice daily | 6-8 h | Dry mouth, blurred vision | Often split‑dose; higher peak‑to‑trough fluctuations |
| Trospium | 20 mg twice daily | 8-12 h | Constipation, headache | Less likely to cross blood‑brain barrier; good for cognitively vulnerable patients |
| Mirabegron | 25-50 mg daily | 24 h | Hypertension, nasopharyngitis | β‑3 agonist, non‑anticholinergic; useful if anticholinergics cause intolerable dryness |
When to Seek Medical Review
If you notice any of the following, contact your GP promptly:
- Sudden increase in urinary frequency (>15 times per day)
- Severe constipation persisting more than two weeks
- Blurred vision or difficulty urinating
- Signs of urinary tract infection (painful burning, fever)
These signals may indicate that the dose needs adjustment or that an alternative therapy is warranted.
Quick Takeaways
- Take solifenacin nightly and set a reminder.
- Start at 5 mg; increase only after a few weeks if tolerated.
- Combat dry mouth with water, sugar‑free gum, and saliva lozenges.
- Limit caffeine/alcohol, spread fluid intake, and log your voids.
- Combine medication with pelvic floor exercises and bladder‑training techniques.
How long does it take for solifenacin to relieve symptoms?
Most patients notice a reduction in urgency within one to two weeks, but the full effect may take up to six weeks as the bladder muscle adapts.
Can I take solifenacin with other overactive bladder meds?
Combining two anticholinergics isn’t recommended because side‑effects amplify. If solifenacin alone isn’t enough, doctors may add mirabegron, which works via a different pathway.
Is solifenacin safe for people with glaucoma?
Anticholinergics can increase intra‑ocular pressure, so patients with narrow‑angle glaucoma should avoid solifenacin unless an eye specialist gives the green light.
What should I do if I miss a dose?
Take the missed tablet as soon as you remember, unless it’s close to the time of your next dose. In that case, skip the missed one and resume your regular schedule-don’t double‑dose.
Can lifestyle changes replace solifenacin?
Lifestyle tweaks (fluid timing, bladder training, pelvic floor work) can markedly improve symptoms, but many patients still need medication for reliable control. Discuss with your GP whether a trial without drugs is appropriate for your case.






Ashok Kumar
October 21, 2025 AT 18:06Hey, I get that waking up at 2 a.m. to dash to the loo is a nightmare, and a nightly pill might sound like the perfect cheat code. The good news is solifenacin’s once‑daily dosing does sync nicely with bedtime, so you won’t have to remember another alarm. Just set a phone reminder and keep the bottle by your pillow – it’s practically foolproof. If you miss a dose, don’t panic; just skip it and get back on schedule.
Esther Olabisi
October 21, 2025 AT 18:56Totally agree, a little reminder can be a lifesaver 🙃. I’ve found that putting the bottle on the night‑stand beats the “I’ll remember later” excuse every single time. Keep that water bottle handy too, because staying hydrated without over‑drinking is a tightrope walk. And hey, if the dry mouth kicks in, a sugar‑free gum is basically a superhero sidekick 😎.
John Price
October 21, 2025 AT 19:46Set the reminder, keep the pill by the bed, and you’re good.
Vivian Annastasia
October 21, 2025 AT 20:36Wow, what a revelation – a reminder and gum actually work. Who would have guessed that basic common sense could improve a medication routine? It’s almost as if the doctors expect us to be mind‑readers. Still, I suppose a little sarcasm makes the whole bladder‑training thing more bearable.
Jake Hayes
October 21, 2025 AT 21:26From a clinical standpoint, consistent dosing is the cornerstone of anticholinergic efficacy. Skipping nights creates fluctuating plasma levels, which can blunt the therapeutic window and worsen urgency. Moreover, aligning peak concentration with nocturnal hours reduces nocturia episodes, a fact supported by multiple trials. So, the reminder isn’t just convenience; it’s evidence‑based practice.
Casey Cloud
October 21, 2025 AT 22:16Yep the timing thing really matters especially for night‑time urgency it also helps keep side effects steady plus you don’t have to think about it during the day
Erika Thonn
October 21, 2025 AT 23:06i think we all chase the idea of control over our bladdr but the body has its own rhythm. solifenacin is like a gentle hand that tries to calm the storm, yet we keep pushing it with coffee and stress. maybe the real peace comes when we listen to that rhythm instead of fighting it.
Ericka Suarez
October 21, 2025 AT 23:56Oh please, as if a pill can fix a life that’s already on fire! The drama of “controlling” your bladder becomes a spectacle when you add national pride to the mix-our bodies are not a political battleground, they’re just trying to survive the caffeine onslaught. Yet, you’ll hear me say: take the medicine, sip the water, and stop blaming everything else.
parbat parbatzapada
October 22, 2025 AT 00:46they dont tell you that the pharma giants push solifenacin to keep us dependent while they profit from our panic. i swear the government knows the side effects but silences us, sooo maybe the best plan is to ditch the drug and just train the muscle like the ancients did.
Ivan Laney
October 22, 2025 AT 01:36Listen, folks, the United States has long been a beacon of medical innovation, and that includes the development and rigorous testing of drugs like solifenacin, which stands as a testament to our unparalleled pharmaceutical expertise. The pharmacodynamics of this anticholinergic agent are meticulously documented, and the fact that it targets the M3 muscarinic receptors with such precision is nothing short of a scientific triumph that only a nation with our resources could achieve. Moreover, the clinical trials conducted across multiple American research centers have demonstrated a consistent reduction in urgency episodes, thereby validating the drug’s efficacy beyond any reasonable doubt. It would be remiss not to mention the extensive post‑marketing surveillance data that continue to affirm its safety profile when prescribed responsibly, something that many other countries simply cannot guarantee. When you consider the sheer scale of our healthcare infrastructure, encompassing everything from primary care physicians to specialized urologists, the implementation of solifenacin therapy becomes a seamless component of a broader, well‑orchestrated treatment paradigm. The dosage flexibility, allowing a start at five milligrams with the option to titrate to ten, reflects a nuanced understanding of patient variability that is hallmark to American medical practice. Furthermore, the integration of behavioral strategies-fluid management, pelvic floor strengthening, bladder training-into the therapeutic regimen showcases a holistic approach that our healthcare system has championed for decades. Critics may argue that anticholinergic side effects such as dry mouth and constipation are burdensome, yet the United States has invested heavily in patient education resources to mitigate these issues effectively. The availability of over‑the‑counter saliva substitutes, fiber supplements, and even telemedicine consultations underscores a commitment to comprehensive care that borders on the altruistic. In addition, the comparative analysis tables that pit solifenacin against other agents like oxybutynin and mirabegron are a direct result of transparent, data‑driven research that proudly originates from American institutions. Such transparency ensures that clinicians can make informed decisions without the veil of corporate secrecy that plagues many foreign drug markets. And let us not overlook the regulatory rigor applied by the FDA, which enforces stringent labeling, dosage guidelines, and warning statements to protect the consumer. The very existence of these safeguards is a testament to the democratic ethos embedded within our healthcare legislation. Ultimately, the success of solifenacin in managing overactive bladder symptoms is a microcosm of the larger narrative that American medicine, when executed with diligence and integrity, delivers results that are both effective and patient‑centred. Therefore, embracing this medication, alongside the recommended lifestyle modifications, is not merely a personal health choice but a reflection of confidence in the American medical establishment.
Rachel Valderrama
October 22, 2025 AT 02:26Wow, a whole patriotic saga for a bladder pill-who knew urination could be so inspiring? But hey, if the American spirit can kick urgency to the curb, maybe we can all get our lives back on track, one giggle at the night‑time bathroom run at a time.
Brandy Eichberger
October 22, 2025 AT 03:16Indeed, the discourse surrounding solifenacin reflects both scholarly rigor and a touch of national pride, and it’s delightful to see such erudition applied to everyday health concerns.
Eli Soler Caralt
October 22, 2025 AT 04:06i suppose the bladder, like the cosmos, seeks equilibrium; solifenacin merely nudges the stars back into alignment 🌌. nonetheless, the true harmony arises from inside, not from a pill, isn’t it? 🤔