Respiratory Risk Calculator
Important Safety Notice
This tool estimates your risk of breathing suppression when combining gabapentinoids and opioids based on factors mentioned in medical literature. It is not a substitute for professional medical advice.
Results will appear here after calculation
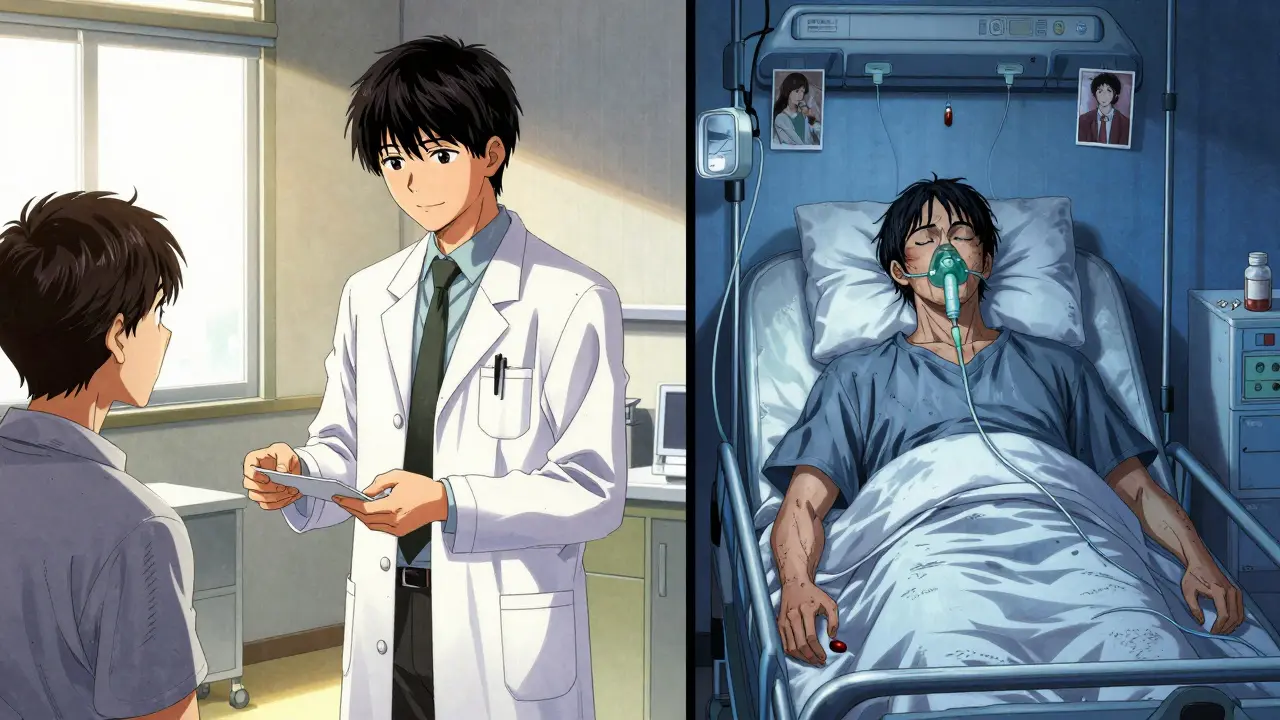
When you take gabapentin or pregabalin for nerve pain, and your doctor adds an opioid like oxycodone or morphine for extra relief, you might think you’re getting better pain control. But what you’re really doing is stacking two drugs that can slow your breathing to dangerous levels - even if you’ve taken them before without issues. This isn’t a rare side effect. It’s a well-documented, life-threatening interaction that’s been quietly killing people for years.
How Gabapentinoids and Opioids Together Can Stop Your Breathing
Gabapentinoids - gabapentin (Neurontin, Gralise) and pregabalin (Lyrica) - were never meant to be painkillers like opioids. They were developed to treat seizures and nerve pain by calming overactive nerves. But somewhere along the way, doctors started using them as opioid-sparing alternatives, hoping to cut down on addiction risk. The problem? Gabapentinoids don’t just calm nerves. They also depress the brain’s breathing center, especially when mixed with opioids.
The U.S. Food and Drug Administration (FDA) issued a formal warning in 2019 after reviewing over 49 cases of severe respiratory depression linked to gabapentinoids. Of those cases, 92% involved either another CNS depressant - like opioids - or a pre-existing condition like lung disease or advanced age. And 24% of those cases ended in death. Every single fatal case had at least one risk factor.
It’s not just about overdose. Even at normal doses, gabapentinoids can cause breathing to slow during sleep. One study with healthy volunteers showed that a single dose of gabapentin led to significantly more apnea episodes - pauses in breathing - than placebo. When combined with remifentanil, a powerful opioid, breathing slowed even more than either drug alone. The effect was additive, not just a little worse - it was multiplied.
Who’s at the Highest Risk?
This isn’t a risk that affects everyone equally. Certain people are far more vulnerable:
- Older adults - Lung function naturally declines with age. The brain’s response to low oxygen weakens. A 70-year-old taking gabapentin and oxycodone has a much higher risk than a 30-year-old.
- People with COPD, asthma, or sleep apnea - Their bodies are already struggling to maintain oxygen levels. Adding a breathing depressant pushes them past the edge.
- Those with kidney problems - Both gabapentin and pregabalin are cleared by the kidneys. If your kidneys aren’t working well, the drugs build up in your system. Even a standard dose can become toxic.
- People on high doses - The risk doesn’t rise linearly. It jumps. One study found that patients on very high doses of gabapentin had nearly double the risk of dying from an opioid-related cause compared to those on lower doses.
And here’s the scary part: many of these people didn’t know they were at risk. Their doctors didn’t warn them. The interaction wasn’t obvious - no vomiting, no confusion, no obvious signs until breathing stopped.
Why This Interaction Is So Hard to Spot
Unlike alcohol or benzodiazepines, gabapentinoids don’t always make you drowsy right away. You might feel fine. You might even feel more alert. But your body is still being suppressed at a cellular level. The brain’s automatic response to low oxygen - the reflex that makes you gasp for air - gets blunted.
There’s another hidden mechanism: gabapentinoids can reverse opioid tolerance. That means if you’ve been on opioids for a while and your body has adapted, adding gabapentin can suddenly make you sensitive to the same dose you used to tolerate. You’re not building tolerance - you’re losing it. That’s why some people die after taking the same dose they’ve taken for months.
Pharmacokinetics make it worse. Opioids slow down your gut. Gabapentin is absorbed mainly in the upper small intestine. If your gut is sluggish, gabapentin lingers longer in its absorption zone. That means more of it enters your bloodstream than expected. You’re not just adding two drugs - you’re accidentally overdosing on one.
The Numbers Don’t Lie
A landmark 2017 study in PLOS Medicine looked at over 16 years of real-world prescribing data. It found that about 8% of patients on opioids were also prescribed gabapentinoids. That might sound low - until you realize those patients had a 50% higher risk of dying from an opioid-related cause. For those on the highest gabapentin doses, the risk jumped to 98% - almost double.
In the UK, the Medicines and Healthcare products Regulatory Agency (MHRA) confirmed similar findings. In 2017, nearly one in four new prescriptions for pregabalin came with an opioid. And yet, most patients weren’t warned about the danger.
Even in hospitals, where monitoring is supposed to be tight, the risk is real. A 2020 study of 5.5 million surgical patients showed that respiratory depression after surgery ranged from 3% in obstetrics to 72% in general surgery when gabapentinoids were used. The evidence? The pain relief from gabapentinoids in these settings is weak at best. The risks? Severe.
What Doctors Should Be Doing - But Often Aren’t
Guidelines from the FDA, MHRA, and the Medical Letter all say the same thing: start low, go slow. If you must use gabapentinoids with opioids, begin with the lowest possible dose. Monitor closely. Avoid in patients with kidney disease, lung disease, or advanced age unless absolutely necessary.
But here’s the gap: most doctors don’t know the full risk. Or they assume their patient is fine because they’ve been on opioids for years. Or they think gabapentin is “safe” because it’s not a narcotic. It’s not. It’s a CNS depressant - and it’s just as dangerous when stacked with opioids.
Renal dosing is often ignored. Pregabalin needs a dose reduction if creatinine clearance is below 60 mL/min. Gabapentin needs adjustment below 70 mL/min. Many prescriptions are written without checking kidney function - especially in older patients.
And yet, the pressure to reduce opioid use led to a surge in gabapentinoid prescribing. The CDC’s 2016 opioid guidelines pushed doctors toward alternatives. Gabapentinoids were easy to prescribe. They weren’t controlled substances. They didn’t show up on drug screens like opioids. So they became the go-to. The unintended consequence? A quiet epidemic of respiratory deaths.
What You Should Do If You’re Taking Both
If you’re on gabapentin or pregabalin and an opioid - whether for pain, anxiety, or sleep - talk to your doctor today. Don’t wait for symptoms. Don’t assume it’s fine because you’ve been taking it for months.
Ask these questions:
- Is this combination really necessary? Is there another option?
- What’s my kidney function? Has it been checked recently?
- Am I on the lowest effective dose of both drugs?
- Have you warned me about breathing risks?
If you’re over 65, have COPD, sleep apnea, or kidney disease, and you’re on both drugs - you’re in a high-risk group. Consider switching to non-CNS depressant alternatives. Topical lidocaine, physical therapy, or certain antidepressants like duloxetine may help with nerve pain without touching your breathing.
If you’re a caregiver for someone on these drugs, watch for subtle signs: slower breathing, confusion, unusual drowsiness, or difficulty waking up. These aren’t normal side effects - they’re warning signs.
The Bottom Line
Gabapentinoids are not harmless. They are not “safe alternatives.” When combined with opioids, they create a perfect storm for respiratory failure. The data is clear. The warnings are out. The deaths have happened.
There’s no magic benefit from combining them. The pain relief isn’t significantly better. The risk is. And that risk doesn’t go away with time. It grows with every dose.
If you’re taking both, don’t panic - but do act. Talk to your doctor. Get your kidney function checked. Question whether you really need both. And if you’re not sure - ask for a second opinion. Your breathing is worth more than convenience.






Mario Bros
January 9, 2026 AT 08:04Bro this is wild. I had no idea gabapentin could mess with breathing like this. My grandpa’s on it for nerve pain and oxycodone for back issues. Gonna call his doc tomorrow. Thanks for the wake-up call.
Paul Bear
January 11, 2026 AT 03:15Let’s be clear: this isn’t ‘hidden danger’-it’s a predictable pharmacokinetic interaction documented since at least 2012. The FDA’s 2019 warning was merely a formality after years of peer-reviewed literature. The real failure is in clinical inertia. Prescribers treat gabapentinoids as ‘safe’ because they’re not Schedule II, ignoring their GABAergic CNS depression profile. When combined with mu-opioid agonists, the respiratory drive suppression is additive, not synergistic-yet still lethal. Renal dosing? Often ignored. Age? Disregarded. This is systemic negligence dressed as compassionate care.
McCarthy Halverson
January 12, 2026 AT 20:02Check kidney function. Lower doses. Ask questions. Don’t wait for symptoms.
Bradford Beardall
January 14, 2026 AT 04:07I’m from the U.S. but my cousin in Mumbai was prescribed this combo for diabetic neuropathy. No one warned her. She almost didn’t wake up one morning. I showed her this post-she’s switching to pregabalin at half dose and got a referral to PT. Real talk: this isn’t just an American problem. Global prescribing habits are dangerously lazy.
neeraj maor
January 15, 2026 AT 13:24Big Pharma pushed gabapentin as the ‘safe’ opioid alternative because it’s cheaper to make and has no DEA reporting. The FDA knew. Doctors knew. But they kept writing scripts because insurance paid for it and patients didn’t complain-until they stopped breathing. This is a profit-driven massacre disguised as medical progress.
Christine Milne
January 16, 2026 AT 14:10Oh please. This is just another fear-mongering article from overzealous medical bureaucrats trying to control patient autonomy. My uncle has been on gabapentin and oxycodone for 12 years. He’s 78. Runs marathons. Breathes fine. If you’re going to scare people, at least cite studies with actual mortality rates-not cherry-picked case reports.
anthony martinez
January 18, 2026 AT 07:35So… we’re supposed to stop using two widely prescribed meds because some people die? What’s next? Banning water because people drown?
Ashlee Montgomery
January 19, 2026 AT 21:44It’s not just about the drugs. It’s about how we treat pain as a problem to be solved with chemicals instead of a signal to be understood. We’ve turned bodies into machines with sliders-turn up the opioid, add the gabapentin, call it a day. But pain isn’t linear. And neither is safety.
Jake Kelly
January 20, 2026 AT 18:06Thanks for sharing this. I’ve been on both for years and never knew. I’m scheduling a kidney panel and asking my doctor about alternatives. Better safe than sorry.
Kunal Majumder
January 21, 2026 AT 15:33Man I’m from India too and this is so real here. Doctors give gabapentin like candy. No labs, no questions. My aunt took it with tramadol for back pain and slept through a fire alarm. Scary stuff. Gotta spread the word.
Jaqueline santos bau
January 22, 2026 AT 00:04THIS IS WHY WE CAN’T HAVE NICE THINGS. The medical establishment is a corrupt circus and you’re all just sheep swallowing pills while the pharmaceutical CEOs laugh all the way to the bank. My cousin died from this exact combo and they called it ‘natural causes.’ LIES. LIES. LIES.
Ritwik Bose
January 23, 2026 AT 18:44Thank you for this deeply informative post 🙏 I am from India and have seen many patients on this combination without proper monitoring. The lack of awareness among both physicians and patients is alarming. I urge everyone to consult a pain specialist and consider non-pharmacological options like acupuncture or mindfulness-based therapy. Safety first, always 💙
Michael Marchio
January 24, 2026 AT 04:43Look, I get it. You’re scared. You read a scary article and now you’re panic-scrolling through Reddit like it’s the end times. But let’s be honest-most people on this combo are fine. The ones who die? Usually have three other comorbidities, drink like a fish, and don’t tell their doctor about their 10 mg of oxycodone they’re stealing from their neighbor. You want to save lives? Stop demonizing medications and start holding patients accountable for their choices. This isn’t a pharmacological conspiracy-it’s a behavioral failure wrapped in medical jargon.