Going to a medication review appointment can feel overwhelming-especially if you’re taking several pills a day, have seen multiple doctors, or aren’t sure why you’re on certain medicines. But this isn’t just another check-up. A medication review is your chance to make sure every drug you take is still necessary, safe, and working the way it should. If you’re on five or more medications, or if you’ve noticed new side effects, changes in how you feel, or trouble remembering when to take things, this appointment could literally save your life.
What Exactly Is a Medication Review?
A medication review is a formal conversation with your GP or a clinical pharmacist about everything you’re taking-prescription, over-the-counter, vitamins, herbal remedies, even creams and inhalers. It’s not about just checking if you’re taking your pills. It’s about asking: Do you still need all of them? Are they helping? Are they hurting?
In the UK, NHS guidelines recommend a full medication review at least once a year. But if you’re older, have chronic conditions like diabetes or heart disease, or take medicines from different specialists, you might need one more often. Some practices even stop sending out repeat prescriptions until you’ve had your review. That’s how seriously they take it.
Step 1: Gather Every Single Medicine You Take
This is the most important step-and the one most people mess up.
Don’t just list your prescriptions. Bring everything:
- Prescription tablets and liquids
- Over-the-counter painkillers like paracetamol or ibuprofen
- Vitamins, minerals, and supplements (even the ones you only take once a week)
- Herbal remedies (like St John’s Wort or ginkgo biloba)
- Inhalers, eye drops, creams, patches, and injections
Put them all in a clear plastic bag. Don’t just bring the bottle labels. Bring the actual items. Why? Because your pharmacist or doctor needs to see the strength, the expiry date, and how the medicine looks. A pill that says “5mg” on the bottle might actually be a 10mg tablet cut in half. They can’t know that unless they see it.
And yes-even the stuff you got from the supermarket or a chemist. If you take it, it counts.
Step 2: Make a Clear, Simple List
Write down each medicine with four key details:
- Name-what it’s called (e.g., “Atorvastatin 20mg”)
- Dose-how much you take (e.g., “one tablet daily”)
- Why you take it-what condition it’s for (e.g., “for high cholesterol”)
- Who prescribed it-which doctor or specialist
Also note any side effects you’ve noticed. Not just the big ones. Even small things like “I feel dizzy after lunch” or “I’ve been constipated since I started this pill” matter. These aren’t complaints-they’re clues.
For people with Parkinson’s, timing is critical. If you take levodopa every 3-4 hours, write down exactly when you take each dose. Missing by even 30 minutes can affect how well it works.

Step 3: Think About Your Goals and Concerns
Ask yourself:
- Is there a medicine you’d like to stop because it causes drowsiness or stomach upset?
- Are you confused about why you’re on a certain drug?
- Do you find it hard to swallow pills or open bottles?
- Have you missed doses because you forgot or couldn’t afford them?
Write these down. Don’t rely on memory. The appointment is only 20-45 minutes. You need to use that time wisely.
Some people worry about sounding like they’re questioning their doctor. But this isn’t about blame. It’s about teamwork. Your pharmacist or GP isn’t there to judge you. They’re there to fix what’s broken.
Step 4: Know What to Expect During the Appointment
During the review, your provider will likely:
- Check your list against your medical records
- Ask about side effects you’ve had
- Look for drug interactions (e.g., mixing blood thinners with certain painkillers)
- Check if any medicines are no longer needed
- Discuss alternatives-like switching from a pill to a patch if swallowing is hard
- Explain what each medicine does and why it’s still important
They might suggest stopping one medicine, lowering a dose, or adding something new. Don’t panic. This isn’t a surprise. It’s part of the plan.
If you’re unsure about a change, say so. Ask: “What happens if I don’t make this change?” or “What are the risks of keeping this medicine?”
Step 5: Prepare for Telehealth or Home Visits
If your review is online or over the phone, preparation becomes even more critical.
For video calls:
- Have all your medicines in front of you
- Test your camera and mic ahead of time
- Use a quiet room with good lighting
- Have your list printed out or open on a second screen
For phone calls:
- Read your list out loud before the call
- Keep your medicines on the table so you can describe them
- Ask if they can email you a summary after the call
If you can’t get to the clinic, ask about a home visit. Many NHS practices offer this for people with mobility issues or chronic illness. You have to request it-don’t wait for them to offer.
What Happens If You Don’t Go?
Some GP practices don’t just remind you-they stop prescribing.
At Godiva Group Practice, if you don’t respond to three reminders, they reduce your repeat prescriptions to a one-month supply. After that? No more prescriptions until you’ve had your review. That’s not punishment. It’s safety.
Medications can interact in dangerous ways. A pill you took for years might suddenly clash with a new one. A high blood pressure drug might make your kidneys work harder. Without a review, these risks build up silently.
What If You’re Still Confused?
You’re not alone. Many people leave their appointment with more questions than answers. That’s okay.
Ask for a written summary. Ask for a follow-up. Ask if you can speak to the pharmacist again. Some practices have medication review nurses who can answer questions between appointments.
And if you’re still unsure about a change-don’t stop the medicine on your own. Call your practice. Wait for guidance. Even small changes can cause big problems if done without advice.
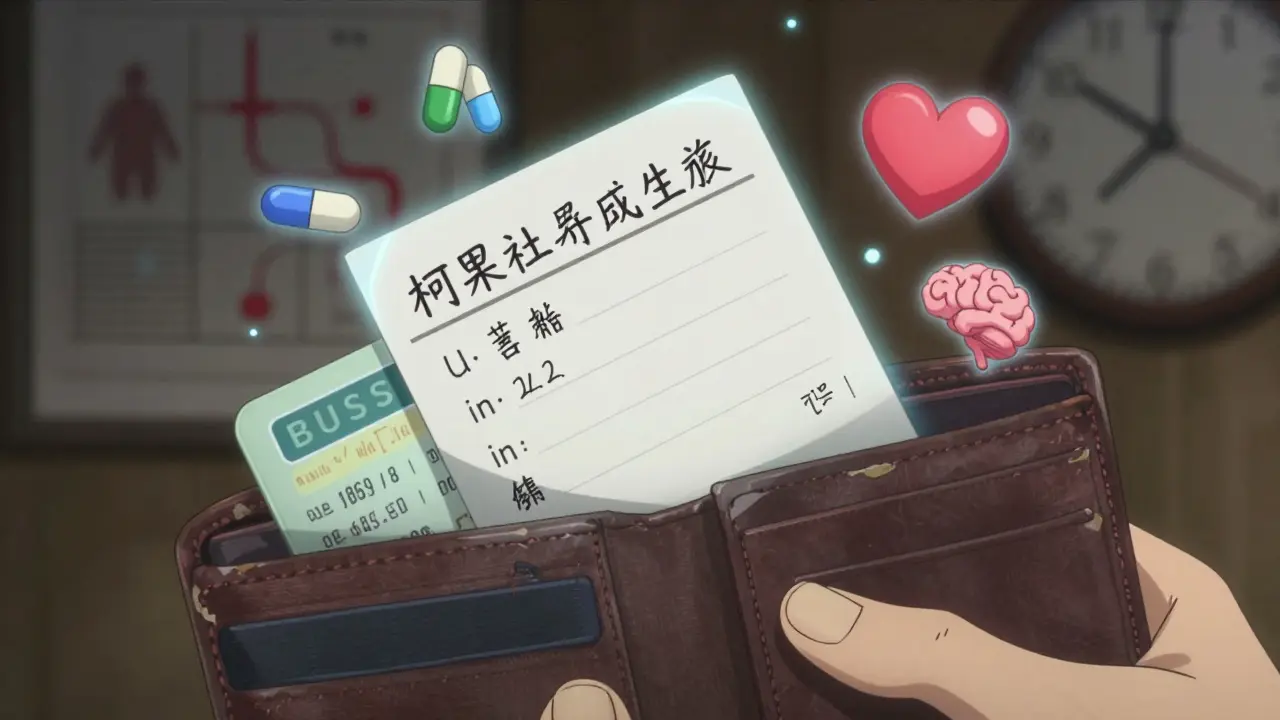
Final Tip: Keep Your List Updated
After your review, update your list. If you’re stopped from taking a medicine, cross it out. If you start a new one, add it immediately. Keep the list in your wallet, phone, or on your fridge.
Next time you see a specialist, or go to A&E, show them this list. It’s your most important health document.
Medication reviews aren’t about control. They’re about clarity. They’re about making sure your body isn’t fighting itself with too many pills, too many side effects, or too many unknowns. You don’t need to be perfect. You just need to be prepared.
Do I need to bring my medicines if I’m seeing my GP for a medication review?
Yes. Even if your GP has your prescription history, they need to see the actual medicines. Bottles can be mislabelled, doses can be changed, and you might be taking something not on your record-like a supplement or over-the-counter painkiller. Bringing everything ensures nothing gets missed.
Can I bring someone with me to the appointment?
Absolutely. Many people find it helpful to bring a family member or friend. They can help remember what was said, ask questions you might forget, and support you if you’re feeling overwhelmed. Some practices even encourage it, especially for older adults or those with memory issues.
What if I don’t know why I’m taking a certain medicine?
That’s normal-and exactly why the review exists. Write down the name of the medicine and say, “I’m not sure why I’m taking this.” Your GP or pharmacist will check your records and explain its purpose. Sometimes, medicines are prescribed for a short-term issue and never stopped. They might be able to remove it safely.
Are medication reviews only for older people?
No. While older adults are more likely to take multiple medications, anyone on five or more medicines should have a review. This includes people with diabetes, epilepsy, mental health conditions, or those taking painkillers long-term. Age isn’t the only factor-polypharmacy is.
Can my pharmacist do the medication review instead of my GP?
Yes. In many NHS practices, clinical pharmacists lead medication reviews. They’re specially trained in drug interactions, side effects, and dosing. In fact, some patients prefer seeing a pharmacist because they spend more time explaining how each medicine works. Your GP might refer you to one if they’re busy or if your case is complex.
What if I can’t afford my medicines?
Tell your GP or pharmacist. They can help you apply for free prescriptions if you qualify (e.g., through NHS Low Income Scheme), suggest cheaper alternatives, or switch you to generic versions. Cost shouldn’t stop you from taking what you need-but you need to speak up. They can’t help if they don’t know.
How often should I have a medication review?
At least once a year. But if you’ve recently started a new medicine, changed doses, had a hospital stay, or noticed new side effects, you should ask for one sooner. Some people need reviews every 3-6 months, especially if they’re on high-risk medications like blood thinners or strong painkillers.
What if I want to stop a medicine but my doctor says no?
You have the right to ask-and to get a clear reason why. If you’re concerned about side effects or feel the medicine isn’t helping, say so. Ask: “Can we try reducing the dose first?” or “Is there another option?” Sometimes, a slow taper is possible. Never stop suddenly without guidance, especially for antidepressants, steroids, or seizure meds. But your voice matters.






MARILYN ONEILL
January 20, 2026 AT 16:39I mean, why are we even doing this? Like, I brought my whole medicine cabinet to my last review and the pharmacist just sighed and said, 'You're fine.' I'm not even on five meds and I had to explain what a fish oil capsule is. This is a waste of time.
Coral Bosley
January 20, 2026 AT 16:45I cried during my medication review. Not because I was scared, but because for the first time in years, someone actually looked me in the eye and asked if I wanted to keep taking the thing that made me feel like a zombie. I stopped the antidepressant they prescribed me after my divorce. I’m not cured, but I’m alive. And I didn’t need a pill to prove it.
Steve Hesketh
January 22, 2026 AT 03:47Bro, this guide is everything. I’m from Nigeria and my uncle in Lagos just started on seven meds after his stroke. I printed this out, translated it into Pidgin, and sat with him for an hour going through each bottle. He didn’t know why he was taking the blood thinner-thought it was for his back pain. We called his clinic, they were shocked. Now he’s got a follow-up next week. This isn’t just advice-it’s a lifeline for people who don’t speak English or trust the system. Keep sharing this.
shubham rathee
January 23, 2026 AT 21:00MAHENDRA MEGHWAL
January 25, 2026 AT 11:01Thank you for this comprehensive and meticulously structured guide. I have been practicing clinical pharmacy in rural India for over a decade, and I can confirm that the majority of patients, particularly those with multimorbidity, are unaware of the cumulative pharmacological burden they carry. The practice of bringing actual medications to the consultation, as emphasized here, is not merely recommended-it is indispensable. I have witnessed preventable hospitalizations due to misidentified tablets and unreported herbal supplements. This document should be mandated in all primary care settings.
Sangeeta Isaac
January 26, 2026 AT 14:57so i brought my meds to my review and the pharmacist said ‘oh wow you’re on like 12 things’ and i said ‘yeah and i’m 32’ and she just stared at me like i’d confessed to being a vampire. turns out i was on a med for a condition i never had and another one that made me feel like my brain was full of wet cotton. now i’m down to 4 and i haven’t cried in 3 months. also i still take melatonin because i’m a chaos gremlin and sleep is a myth.
Ben McKibbin
January 27, 2026 AT 22:38This is the most important health advice I’ve ever read. I’ve seen too many people get prescribed a new drug for every new symptom instead of stepping back and asking: ‘What’s really going on?’ My mom was on six antidepressants because she was lonely-not depressed. Once they took her off them and connected her with a community group, she started painting again. Medications aren’t magic. They’re tools. And sometimes the best tool is silence, rest, or a friend who shows up with soup.
Melanie Pearson
January 28, 2026 AT 03:04This guide is dangerously naive. The NHS doesn’t care about your safety-they care about reducing liability. Every time someone dies from a drug interaction, they blame the patient for not ‘being prepared.’ Meanwhile, the pharmaceutical lobby funds their training programs and pushes polypharmacy as standard. You think they want you to stop your meds? They want you to keep paying for them. This isn’t healthcare. It’s corporate compliance dressed in a white coat.
Uju Megafu
January 29, 2026 AT 00:37Oh my GOD. I’m so mad right now. I’ve been taking that stupid blood pressure pill for 8 years because my doctor said ‘it’s fine’ and then I got dizzy and fell and broke my hip and no one asked me if I was taking anything else. I had a herbal tea for ‘calm’ that my cousin gave me and it was literally interacting with my heart med. I could’ve died. And now they want me to bring my bottles? That’s not helpful-that’s trauma. But I did it anyway. And now I’m off two drugs. So… thank you? I guess? I still hate the system.
Barbara Mahone
January 29, 2026 AT 08:00I brought my list to my appointment and the pharmacist smiled and said, ‘You’ve done more than 90% of patients.’ I didn’t know that was a thing you could do. I just didn’t want to be the person who forgot why they were taking something. I keep the list on my phone and on my fridge. I even showed it to my dentist last week. He said, ‘You’re a legend.’ I just wanted to live.
Kelly McRainey Moore
January 30, 2026 AT 10:41my grandma brought her meds in a shoebox and the pharmacist laughed and said ‘this is why we need a system’ and then spent 45 minutes helping her sort them into pill organizers. now she’s got a routine and she’s not falling down anymore. i cried in the parking lot. this stuff matters.
Ashok Sakra
January 31, 2026 AT 15:43lokesh prasanth
February 1, 2026 AT 18:45Samuel Mendoza
February 3, 2026 AT 13:09Glenda Marínez Granados
February 5, 2026 AT 03:14So I brought my 11 pills, 3 patches, and 2 bottles of ‘natural energy boost’ (aka sugar water with glitter) to my review. The pharmacist looked at me and said, ‘You’re not a pharmacy. You’re a person.’ And then we took away 5 things. I feel like I got my body back. Also, I cried. Again. 😭