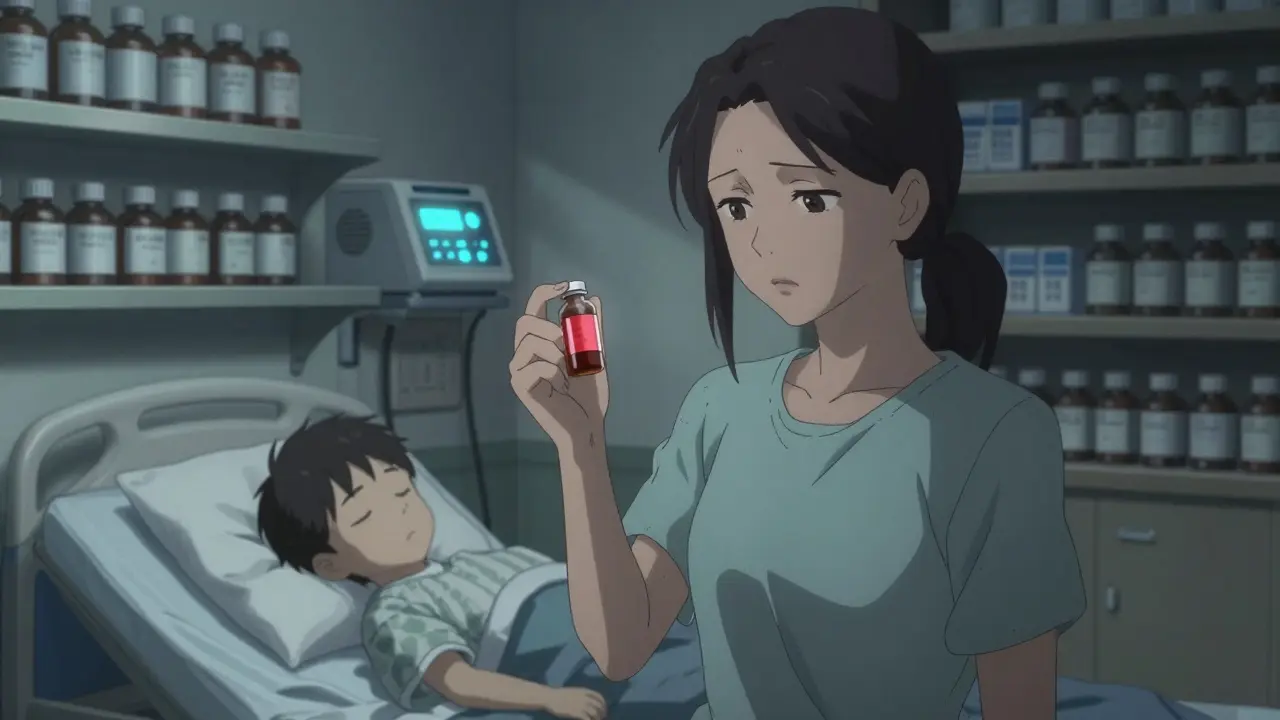
When your child needs a medicine that isn’t available in a store-bought bottle - maybe they can’t swallow pills, or they’re allergic to dyes, or they need a tiny dose that no manufacturer makes - compounded medications can feel like a lifeline. But behind that lifeline is a hidden risk. Compounded drugs aren’t tested by the FDA. They’re made one at a time, by hand, in a pharmacy. And for kids, even a small mistake can be life-changing.
Why Compounded Medications Are Used for Children
Most kids don’t need custom-made medicines. But some do. The reasons are specific and often urgent:- Children who can’t swallow pills need liquids - but no company makes a liquid version of their medicine.
- Some kids are allergic to preservatives, dyes, or alcohol found in commercial drugs. Compounding lets pharmacists remove those ingredients.
- Neonates in the NICU need ultra-small doses of powerful drugs like morphine or fentanyl. A single drop too much can be deadly.
- Diabetic children need sugar-free versions of medicines that normally contain syrup.
- Bitter-tasting drugs can be masked with flavorings like strawberry or bubblegum to help kids take them without a fight.
These aren’t luxury choices. They’re medical necessities. But that doesn’t mean they’re safe by default.
The Hidden Dangers of Compounding
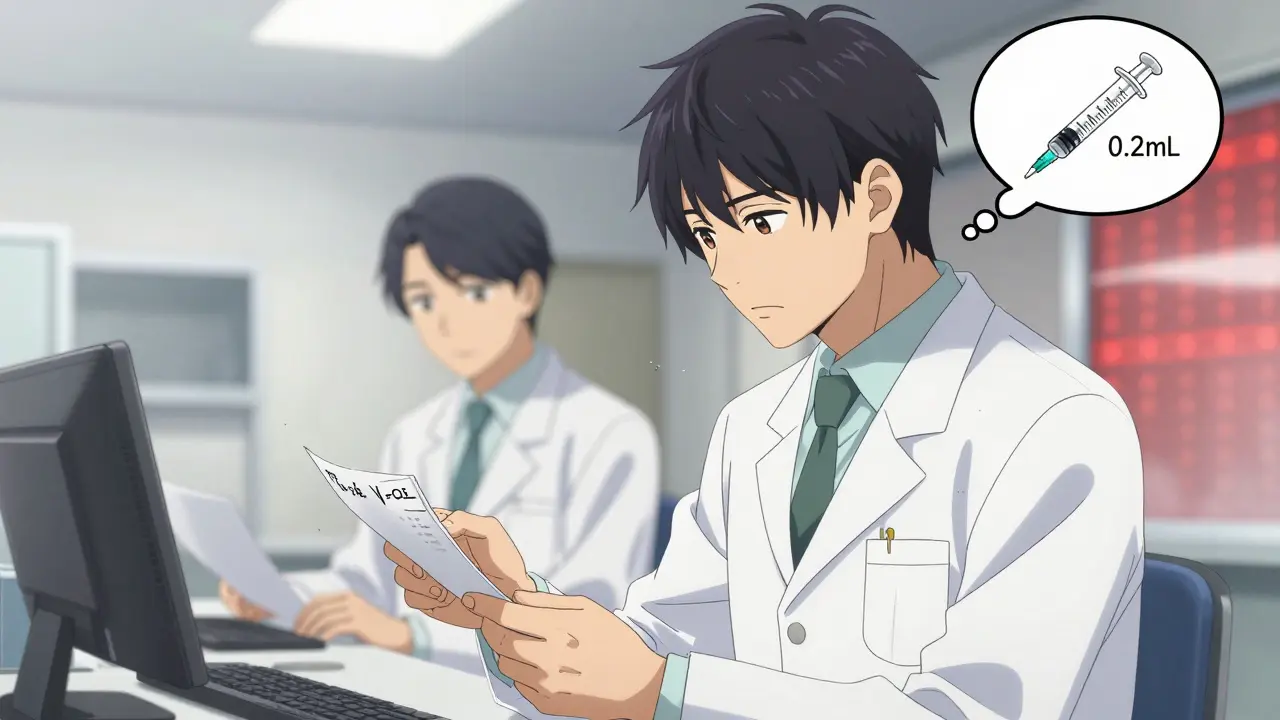
The biggest danger isn’t the medicine itself - it’s the process. Compounding is manual. One pharmacist, one scale, one syringe. No automated checks. No batch testing. No FDA oversight.Here’s what can go wrong:
- Dosing errors: A child weighing 12 pounds needs 0.2 mL of a drug. The pharmacist misreads the prescription and prepares 2 mL. That’s a tenfold overdose.
- Wrong concentration: A parent is told to give 5 mL of a liquid. But the label says 10 mg/mL - when it should’ve been 1 mg/mL. That’s a 10x overdose again.
- Contamination: In 2012, a compounding pharmacy in Massachusetts shipped contaminated spinal injections. 800 people got sick. 64 died.
- Inconsistent potency: One batch of compounded levothyroxine had 40% less active ingredient than prescribed. A child developed severe hypothyroidism and ended up in the ER.
According to the Institute for Safe Medication Practices, between 14% and 31% of pediatric medication errors involve compounded drugs. Most are dosing mistakes. Most are preventable.
When to Avoid Compounded Medications
Not every “custom” medicine is necessary. The FDA says clearly: Don’t use compounded drugs if an approved version exists.For example:
- If a child needs an antibiotic, there are FDA-approved liquid versions available. Use those.
- If a child needs insulin, premixed, pre-filled syringes exist. Don’t ask a pharmacy to compound it from powder.
- If a child needs GLP-1 drugs like semaglutide (used for obesity or diabetes), the FDA has documented over 900 adverse events - including 17 deaths - linked to compounded versions as of December 2024. These are not safe for children.
Compounding should be a last resort, not a shortcut. If your doctor suggests a compounded drug, ask: “Is there an FDA-approved version?” If the answer is yes, push for it.
How to Choose a Safe Compounding Pharmacy
Not all pharmacies are created equal. Some are clean, trained, and accredited. Others cut corners.Here’s how to pick the right one:
- Look for PCAB or NABP accreditation. The Pharmacy Compounding Accreditation Board (PCAB) and the National Association of Boards of Pharmacy (NABP) are the only two groups that certify compounding pharmacies for quality and safety. Only about 1,400 of the 7,200+ compounding pharmacies in the U.S. have this accreditation.
- Ask if they use gravimetric analysis. This is a high-tech weighing system that measures ingredients to the milligram. It’s far more accurate than manual measuring. Hospitals that use it cut pediatric dosing errors by 75%. But only 7.7% of U.S. hospitals use it - because it costs $25,000 to $50,000 per station.
- Check if they do double-checks. For every pediatric dose, two trained staff members should independently verify the recipe, the measurement, and the final product. Ask: “Do you have a second pharmacist check every child’s dose?”
- Ask about their training. Pharmacists who compound for kids need 40+ hours of special training in pediatric calculations. Ask if their staff is certified.
Don’t be shy. This is your child’s life. If the pharmacy hesitates or can’t answer, find another one.
What Parents Must Do Before Giving the Medicine
Even the best pharmacy can make a mistake. You are the last line of defense.Before you give your child any compounded medicine:
- Ask for the exact concentration. Always. Write it down. Is it 5 mg/mL? 10 mg/mL? 0.5 mg/mL? If they say “it’s the same as the pill,” ask them to show you the label.
- Verify the dose with your doctor and pharmacist. Don’t assume they’re on the same page. Call the doctor’s office and say: “I have a compounded liquid for my child. The prescription says 0.3 mL twice daily. The bottle says 10 mg/mL. Is that correct?”
- Use the right measuring tool. Never use a kitchen spoon. Use the syringe or dosing cup the pharmacy gives you. If they don’t give you one, ask for it. If they say “just use a teaspoon,” walk out.
- Check the color, smell, and texture. If the liquid looks cloudy, smells off, or has particles in it - don’t use it. Call the pharmacy immediately.
- Store it correctly. Some compounded meds need refrigeration. Others must be used within 14 days. Ask for written storage instructions.
68% of pediatric compounding errors happen because the parent didn’t understand the concentration. That’s not their fault. It’s the system’s failure. But you can stop it.

The Tragedy That Changed Everything
In 2006, two-year-old Emily Jerry died after receiving a compounded chemotherapy dose that was 100 times too strong. The error happened because a pharmacist misread a decimal point. The technology to prevent it - gravimetric analysis - was already available. But the pharmacy didn’t use it.Her father, Jerry, turned grief into action. He founded the Emily Jerry Foundation and pushed for “Emily’s Law.” As of April 2025, 28 states have introduced legislation requiring gravimetric verification for all pediatric compounded sterile preparations.
Emily’s story isn’t just a warning. It’s a blueprint. If your child needs a compounded drug, ask: “Would you have used gravimetric analysis if this were your child?”
What’s Changing in 2025
The FDA is cracking down. In May 2025, they issued a warning that compounding pharmacies are exploiting drug shortages to mass-produce unapproved drugs - even after the shortages are over. They’ve seen more than 900 adverse events linked to compounded semaglutide and tirzepatide, including 17 deaths.The National Academy of Medicine called the rise in compounding “a significant threat” to children’s health. The ISMP is developing new pediatric safety metrics for 2025. And more hospitals are finally investing in gravimetric systems.
But change is slow. The cost, training, and paperwork are still barriers. Until every pharmacy uses the same safety standards, you have to be your child’s advocate.
Final Checklist for Safe Use
Before giving your child a compounded medication:- ✅ Is there an FDA-approved version available? If yes, use it.
- ✅ Is the pharmacy PCAB or NABP accredited?
- ✅ Do they use gravimetric analysis for pediatric doses?
- ✅ Do they do a double-check by two trained staff members?
- ✅ Do you have the exact concentration written down? (e.g., 5 mg/mL)
- ✅ Did you confirm the dose with both the doctor and pharmacist?
- ✅ Did you get the correct measuring device?
- ✅ Did you check the medicine’s appearance and smell?
- ✅ Do you know how to store it and when it expires?
If you can answer yes to all nine, you’ve done everything you can to keep your child safe. If even one is no - stop. Call your doctor. Find a better pharmacy. Don’t guess. Don’t rush. This isn’t just medicine. It’s your child’s health.
Are compounded medications FDA-approved?
No. Compounded medications are not reviewed or approved by the FDA. This means the agency does not check their safety, effectiveness, or quality before they’re given to patients. They’re made by individual pharmacies under state regulations, not federal drug standards.
Can I trust any pharmacy that says they compound for kids?
No. Only pharmacies with PCAB or NABP accreditation follow strict safety standards. About 80% of compounding pharmacies in the U.S. don’t have this accreditation. Always ask to see their certification. If they can’t show it, find another pharmacy.
What should I do if my child has a bad reaction to a compounded medicine?
Stop giving the medicine immediately. Call your doctor or go to the ER. Report the reaction to the FDA’s MedWatch program. Also, contact the pharmacy and ask for a copy of the batch record. This helps track if others had the same issue.
Why is concentration so important in pediatric compounding?
Children’s doses are based on weight and age, not adult standards. A concentration of 10 mg/mL might be fine for an adult, but for a 20-pound child, it could be a deadly overdose. If the label doesn’t clearly state the concentration (e.g., 1 mg/mL, 5 mg/mL), don’t use it. Always confirm it with the pharmacist.
Is it safe to use compounded GLP-1 drugs like semaglutide for children?
No. The FDA has documented over 900 adverse events - including 17 deaths - linked to compounded versions of semaglutide and tirzepatide as of December 2024. These drugs are not approved for children, and compounded versions have caused severe gastrointestinal problems, pancreatitis, and hospitalizations. Avoid them completely.
How can I tell if a compounded medicine has gone bad?
Look for changes in color, cloudiness, particles, or unusual odor. If the liquid looks different than when you first got it, or if it smells sour or chemical, don’t use it. Also check the expiration date - many compounded meds only last 14 to 30 days, even if refrigerated.
Do I need to refrigerate my child’s compounded medicine?
It depends. Some compounded liquids need refrigeration to stay stable. Others can be stored at room temperature. Always ask the pharmacist for written storage instructions. If they don’t give you any, ask again. Improper storage can reduce potency or cause contamination.





Kayla Kliphardt
December 31, 2025 AT 11:45I never realized how much goes into compounded meds for kids. I thought it was just mixing stuff up, but the dosing errors? Holy cow. I’m so glad I asked my pharmacist for the concentration last time - they were surprised I even knew to ask.
Still, I’m scared to use them at all now. What if I miss something?
Joy Nickles
January 2, 2026 AT 09:10OMG I JUST FOUND OUT MY KID’S MED IS COMPOUNDED AND THE PHARMACY HAS NO ACCREDITATION??!!?? I’M GOING TO CALL THEM RIGHT NOW AND THROW A FIT!! THEY DIDN’T EVEN GIVE ME A SYRINGE JUST A TEASPOON??!! I’M SO ANGRY I’M CRYING RN 😭😭😭
Emma Hooper
January 3, 2026 AT 16:14Honey, you’re not alone - I’ve been there. I once gave my daughter a compounded antibiotic that smelled like burnt plastic. I almost didn’t notice until she started vomiting. Turned out the batch was contaminated.
Now I demand to see the PCAB sticker, the double-check log, and the gravimetric report. If they blink? I’m out. Your kid’s life isn’t a lab experiment.
And yes, I’ve walked out of three pharmacies this year. No regrets.
Martin Viau
January 4, 2026 AT 11:48Canada’s system is way more regulated. We don’t let some guy in a basement pharmacy wing it with pediatric doses. FDA’s a joke - they’re asleep at the wheel. If you’re in the US, you’re playing Russian roulette with your kid’s neurology.
Gravimetric analysis? That’s a luxury. We have mandatory batch testing, real-time QC, and pharmacists who’ve done 200+ pediatric compounding cases. You’re lucky if your pharmacy even knows what ‘milligram’ means.
Marilyn Ferrera
January 5, 2026 AT 00:48Always confirm concentration. Always. Write it down. Say it out loud. Then say it again.
If it’s not in writing, it doesn’t exist.
Robb Rice
January 6, 2026 AT 20:50I appreciate this article - it’s thorough, well-researched, and desperately needed. I’ve seen too many parents assume ‘custom’ means ‘better.’ It doesn’t.
My son needed a sugar-free version of his seizure med. We spent three months tracking down a PCAB-accredited pharmacy. Worth every minute.
Don’t rush. Don’t accept ‘it’s fine.’ Ask. And ask again.
Harriet Hollingsworth
January 8, 2026 AT 06:30This is why we can’t have nice things. Pharmacies are cutting corners. Doctors are lazy. Parents are too tired to ask. And kids pay the price.
Emily Jerry’s father should’ve sued every single pharmacy in America. This is negligence. Criminal negligence. And nobody’s going to jail.
Deepika D
January 9, 2026 AT 17:17As a mom of two kids with rare conditions, I’ve lived this. I’ve called 17 pharmacies in one week. I’ve driven 3 hours to get a compounded med that was correctly made. I’ve cried in pharmacy parking lots.
But I’ve also seen the difference - when a pharmacist takes the time to explain, when they use gravimetric, when they call you back.
Don’t give up. You are your child’s best advocate. And you’re not alone. There’s a whole community of us out here - we swap pharmacy names, batch numbers, horror stories, and hope.
Reach out. DM me. I’ll send you the list of 5 trusted compounding pharmacies in the Midwest. No judgment. Just love.
Bennett Ryynanen
January 11, 2026 AT 14:40Man, I used to think compounding was just for rich people or weird cases. Then my niece got sick and they needed a custom dose. I watched the pharmacist measure it with a syringe and then double-check it with another guy. I was like, ‘Wait, that’s actually normal?’
Turns out it’s not. And that’s terrifying.
Thanks for the checklist. I’m printing this out and taping it to the fridge.
Chandreson Chandreas
January 13, 2026 AT 05:43So many parents don’t even know to ask about concentration 😔
But you? You’re already ahead. 🙌
Keep asking. Keep pushing. You’re doing better than most. 💪❤️
Darren Pearson
January 15, 2026 AT 00:26The proliferation of unregulated compounding pharmacies represents a systemic failure in pharmaceutical governance. The absence of federal oversight, coupled with the commodification of pediatric therapeutics, constitutes a profound breach of the Hippocratic imperative. One must question the epistemic authority of state-licensed pharmacists who operate without standardized validation protocols. The gravimetric disparity is not merely a technical issue - it is an ethical one.
Jenny Salmingo
January 16, 2026 AT 14:27I’m from the Philippines and we don’t have much access to this stuff. But I read this and I cried. My cousin’s son needed a special medicine and they had to order it from the US. I never knew how dangerous it could be. Thank you for sharing this. I’m sending it to everyone I know.
Aaron Bales
January 18, 2026 AT 01:09Accreditation matters. Gravimetric matters. Double-check matters.
Ask. Don’t assume. Document.
That’s the whole checklist in three lines.