What is lower GI bleeding?
Lower gastrointestinal (GI) bleeding means blood is coming from somewhere in your colon, rectum, or anus. You might notice bright red blood in your stool, maroon-colored stool, or even just see it on toilet paper. It’s not always painful, and sometimes it happens without warning. This isn’t the same as black, tarry stools-that usually points to bleeding higher up, like in your stomach or small intestine. When it’s lower, it’s called hematochezia.
Every year, about 20 to 27 people out of every 100,000 experience this kind of bleed. It’s rare in younger adults but becomes much more common after age 60. The good news? Most cases stop on their own. The bad news? It can be scary, confusing, and sometimes life-threatening if ignored.
Diverticula: The #1 Cause of Lower GI Bleeding
Diverticulosis is when small pouches form in the wall of your colon. These aren’t infections or inflammation-they’re just weak spots that bulge out. About half of people over 60 have them. Most never know they’re there. But sometimes, one of these pouches starts bleeding.
This bleeding is sudden, massive, and usually painless. You might wake up to see a lot of blood in the toilet or on your underwear. It can look alarming, but it often stops by itself in about 80% of cases. The reason it bleeds? Blood vessels that normally run deep in the colon wall get stretched over the top of a diverticulum. When they’re thin and exposed, they can rupture easily.
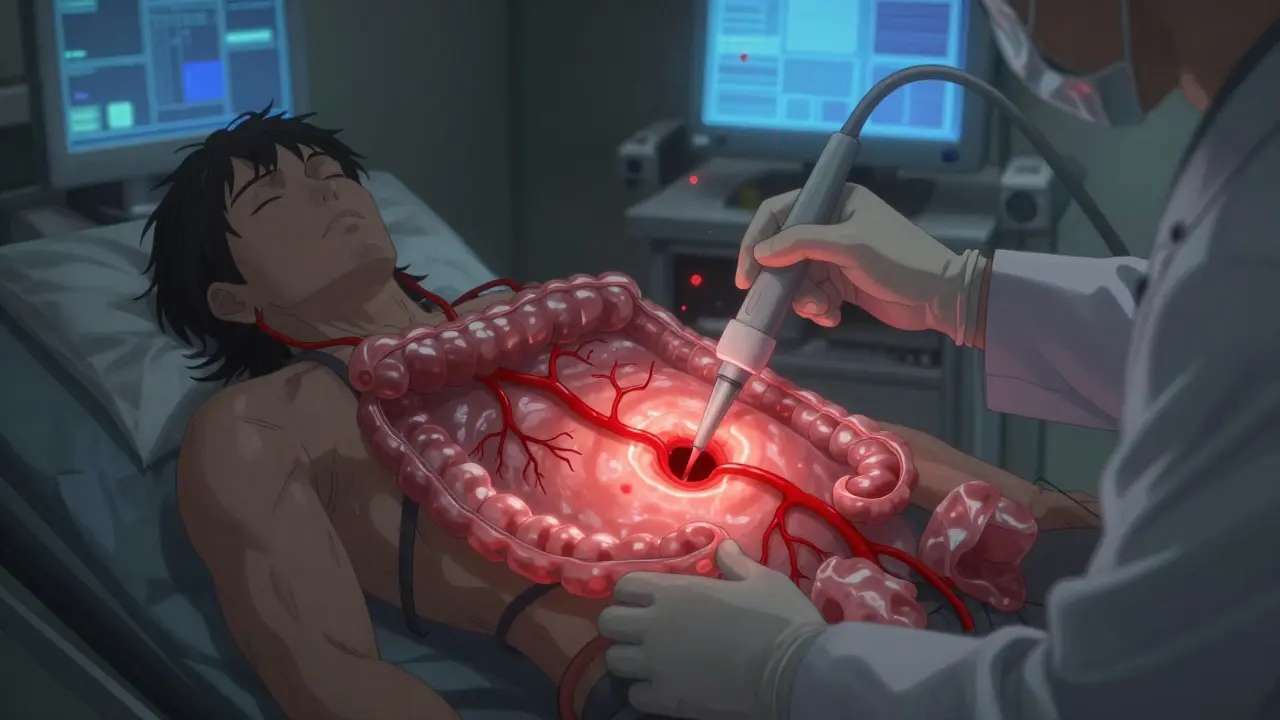
Doctors don’t treat the diverticula themselves. They treat the bleed. That means fluids, blood transfusions if needed, and close monitoring. If the bleeding doesn’t stop, they’ll do a colonoscopy. During the procedure, they can use heat, clips, or epinephrine injections to seal the vessel. Even with treatment, about 1 in 5 people will bleed again within a year.
Angiodysplasia: Silent Bleeding in the Elderly
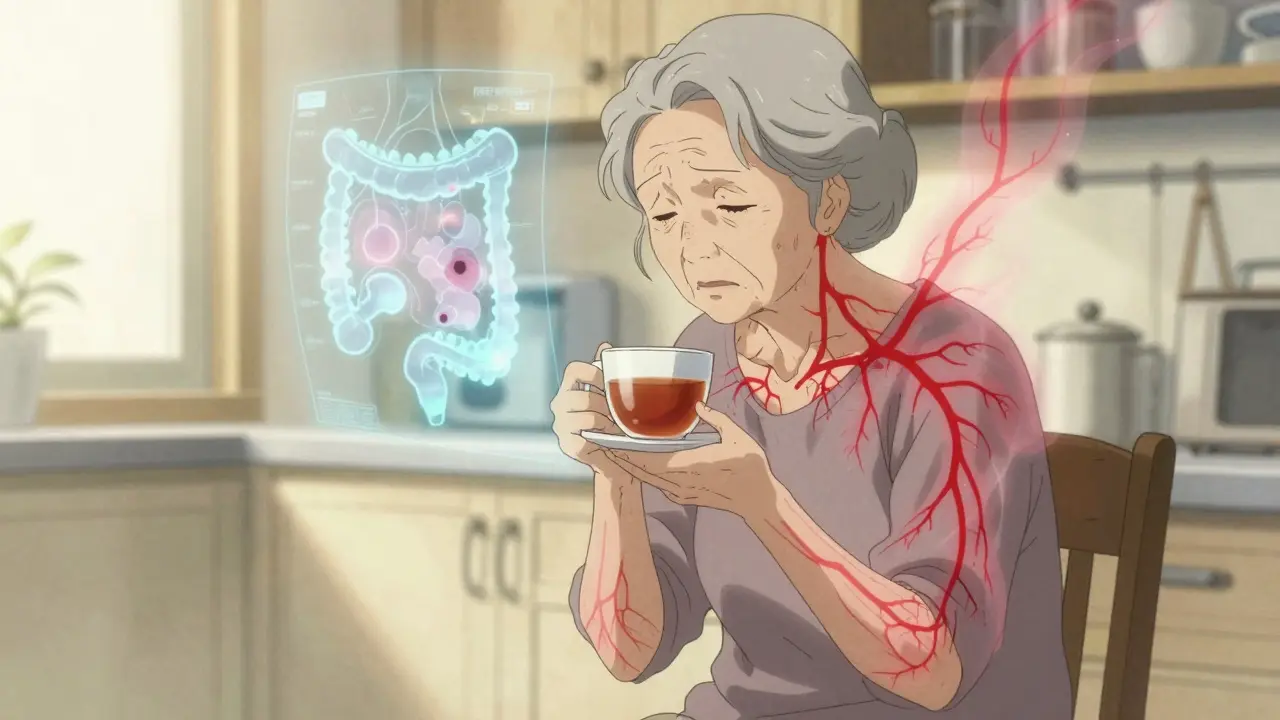
Angiodysplasia-also called vascular ectasia or AVM-is another top cause of lower GI bleeding, especially in people over 70. These are tiny, abnormal connections between arteries and veins in the colon lining. They’re not tumors. They’re just worn-out blood vessels that have stretched out over time.
Unlike diverticula, which bleed suddenly and heavily, angiodysplasia usually bleeds slowly and quietly. You might not even notice blood in your stool. Instead, you feel tired, weak, or short of breath. That’s because you’re slowly losing iron and developing anemia. Many patients are diagnosed only after routine blood tests show low hemoglobin.
These lesions are most common on the right side of the colon, near the cecum. They’re linked to aging, but also to conditions like aortic stenosis. When the heart’s aortic valve is narrowed, it damages a key clotting protein called von Willebrand factor. That makes it harder for blood to clot anywhere-even in your gut.
Endoscopy is the best way to find them. Once seen, doctors use argon plasma coagulation (APC) to burn them off. It works well right away-80 to 90% of bleeds stop. But the problem? They come back. Up to 40% of patients bleed again within two years.
How Do Doctors Figure Out What’s Causing the Bleed?
When someone shows up with GI bleeding, the first thing the team does is check their vitals. Is their blood pressure low? Is their heart racing? Are they dizzy? These signs tell them how serious it is. They’ll run blood tests: hemoglobin, clotting times, kidney function. They’ll check for anemia and see if they need a transfusion.
Then comes the big one: colonoscopy. It’s the gold standard. Done within 24 hours of arrival, it finds the source in 80% of cases and can often stop the bleeding at the same time. You don’t need a perfect bowel prep if you’re actively bleeding. Doctors may give you IV fluids and a drug called erythromycin to clear out the colon faster.
If the colonoscopy doesn’t show anything, and you keep bleeding, they’ll look further. That’s when capsule endoscopy comes in-you swallow a tiny camera that takes pictures as it moves through your small intestine. It finds the cause in about 6 out of 10 cases. But it’s not perfect. In 15% of cases, the capsule gets stuck if there’s a hidden narrowing.
For stubborn cases, doctors may turn to CT angiography. This scan can spot active bleeding as slow as 0.5 mL per minute. It’s fast, non-invasive, and great when you’re unstable or can’t have an endoscopy. If they find the spot, they can sometimes treat it right away with embolization-a radiologist threads a catheter into the bleeding vessel and plugs it with tiny particles.
Treatment Differences: Diverticula vs. Angiodysplasia
Even though both cause bleeding, they’re treated differently.
- Diverticula: Most stop on their own. If they don’t, colonoscopy with clips or heat is the go-to. Surgery is rare-only if you’re bleeding from one specific segment and keep rebleeding.
- Angiodysplasia: APC is the standard. But because it keeps coming back, doctors are now using medications like thalidomide (100 mg daily) or octreotide (injections 3 times a day). Thalidomide, once known for birth defects, has been repurposed-it reduces bleeding in 7 out of 10 patients. Octreotide helps by narrowing blood vessels. Neither is a cure, but they cut down on hospital visits.
Right-sided angiodysplasia often requires a right hemicolectomy-removing the right side of the colon-if bleeding won’t stop. That’s major surgery, but it’s often the only way to stop chronic, recurring blood loss.
What Happens After the Bleed?
Survival rates after lower GI bleeding are mostly tied to your other health problems-not the bleed itself. If you’re otherwise healthy, your chances of living five more years are over 80%. But if you have heart disease, kidney failure, or cancer, your risk goes up.
People with diverticula bleeding have a 10-22% chance of dying within 30 days, but that’s usually because they’re older and sicker. Angiodysplasia has lower death rates-5-10%-but it’s a chronic battle. Many patients end up needing multiple transfusions over years. One study found patients with recurring angiodysplasia spent an average of 18 months going from first symptoms to a confirmed diagnosis. They had three or more negative colonoscopies before the real cause was found.
That’s why some experts now recommend AI-assisted colonoscopy. New software can highlight subtle vascular lesions that human eyes might miss. In one trial, detection rates jumped by 35%. There are also new endoscopic clips that seal bleeding vessels with 92% success-better than older methods.
When to Worry
Not all rectal bleeding is dangerous. Hemorrhoids are common and usually harmless. But if you’re over 60 and suddenly see a lot of blood, or if you’re feeling dizzy, weak, or short of breath-even without visible blood-you need to get checked. Don’t wait. Don’t assume it’s ‘just hemorrhoids.’
High-risk signs include:
- Blood pressure below 100 mmHg
- Heart rate over 100 beats per minute
- Hemoglobin under 10 g/dL
- History of liver disease or cancer
If you have any of these, you need urgent care. Hospitals with dedicated GI bleeding protocols have better outcomes. They act fast, coordinate between endoscopists, radiologists, and surgeons, and reduce delays.
What’s Next in Research?
The NIH is currently running a major trial (NCT04567891) testing thalidomide against placebo for recurrent angiodysplasia. Results are expected in late 2024. If it works, this could become a standard treatment-offering hope to people tired of repeated hospital stays.
Doctors are also studying whether long-term aspirin or NSAID use increases bleeding risk in people with angiodysplasia. Early data suggests yes. If you have this condition, talk to your doctor before taking daily painkillers.
Final Thoughts
Lower GI bleeding isn’t one thing. It’s a symptom with many causes. Diverticula and angiodysplasia are the two biggest culprits in older adults, but they behave completely differently. One hits hard and fast. The other creeps up slowly, stealing your energy before you even notice blood.
The key is early diagnosis. Don’t ignore symptoms. Don’t delay colonoscopy. And don’t assume the first negative test means nothing’s wrong. Sometimes, the bleeding source is tiny, hidden, or intermittent. You might need more than one test.
With modern tools-better scopes, AI, targeted meds, and faster imaging-the outlook has never been better. But it starts with you speaking up. If your stool looks wrong, or you feel off, get it checked. It could save your life.






Janette Martens
December 30, 2025 AT 21:18Manan Pandya
December 31, 2025 AT 04:01Aliza Efraimov
December 31, 2025 AT 11:55Nisha Marwaha
January 1, 2026 AT 16:31Duncan Careless
January 3, 2026 AT 15:16Henriette Barrows
January 4, 2026 AT 16:06Alex Ronald
January 5, 2026 AT 15:48Teresa Rodriguez leon
January 6, 2026 AT 21:46Louis Paré
January 8, 2026 AT 11:49Marie-Pierre Gonzalez
January 9, 2026 AT 21:49Paige Shipe
January 10, 2026 AT 08:36Tamar Dunlop
January 11, 2026 AT 06:11David Chase
January 12, 2026 AT 11:23