When your back or legs hurt every day, and nothing-no pills, no physical therapy, no injections-helps anymore, you start looking at options that sound like science fiction. That’s where spinal cord stimulation (SCS) comes in. It’s not a cure. But for many people with chronic pain that won’t quit, it’s the first real chance at getting their life back.
What Spinal Cord Stimulation Actually Does
Spinal cord stimulation doesn’t fix the damaged nerve or the herniated disc. Instead, it interrupts the pain signal before it reaches your brain. Tiny wires, placed in the space around your spinal cord, send gentle electrical pulses. These pulses don’t hurt-they usually feel like a soft buzzing or tingling. But they block the pain messages from getting through. This isn’t new. Doctors first tried it in 1967. But today’s systems are light-years ahead. Modern devices use advanced waveforms like high-frequency stimulation (1,000-10,000 Hz) or burst patterns that mimic how your nerves naturally fire. These newer styles don’t even need you to feel the tingling. That’s huge for people who hated the old buzz-and-zap feeling. The system has three parts: leads (the wires), a pulse generator (the battery), and a remote to control it. The generator is usually tucked under the skin in your belly or butt. It lasts 5 to 9 years before needing replacement. And yes, you can still get an MRI-with newer models like Boston Scientific’s Precision Montage™ or Medtronic’s Intellis™ 2, which are designed to be safe under full-body scans.Who Is a Good Candidate?
Not everyone with pain qualifies. SCS isn’t for back pain caused by an infection, tumor, or recent injury. It’s for chronic, stubborn pain that’s lasted at least a year, and nothing else worked. The best candidates usually have one of these conditions:- Failed back surgery syndrome (pain after spine surgery)
- Complex Regional Pain Syndrome (CRPS), types I or II
- Chronic leg or lower back pain that hasn’t responded to other treatments
The Trial: Your Test Drive
Before you agree to surgery, you get a trial. It’s not optional. It’s your only way to know if this will work for you. During the trial, thin wires are inserted through a needle into your back, under light sedation. They’re taped to your skin and connected to a small external box you carry in your pocket. You keep it on for 5 to 7 days. You’ll be asked to do your normal activities: walk, sit, bend, sleep. And you’ll rate your pain daily. Success? You need at least a 50% drop in pain. If you only feel 30% better, it’s not worth moving forward. The trial is free of permanent changes. If it doesn’t work, you just take the wires out. No big deal.
How It Compares to Other Treatments
Let’s say you’ve tried everything. Painkillers? You’re on opioids and they’re losing their effect. TENS units? They help for an hour, then you’re back to square one. Injections? They give you a few weeks of relief, then the pain comes roaring back. SCS beats opioids in the long run. A 2021 study of over 2,000 patients found those with SCS used 57% fewer opioids after one year-and 63% less after two years. That’s not just about pain. It’s about avoiding addiction, drowsiness, and constipation. Compared to TENS units (which cost $50-$200), SCS is expensive. But TENS doesn’t work for deep, chronic pain. SCS does. For people with pain that runs down their leg from their lower back, SCS works in 78% of cases. Peripheral nerve stimulation (another option) works better for pain in the foot or hand-but not for the spine. And unlike surgery that cuts or fuses vertebrae, SCS is reversible. If it stops working, you can turn it off and remove it. No permanent changes to your spine.What Can Go Wrong
No medical device is perfect. SCS has risks. The most common problem? Lead migration. That’s when the wires move slightly out of place. It happens in about 15% of cases within six months. You’ll notice your pain comes back in a new spot-or the tingling shifts. It’s fixable, but you’ll need another minor procedure to reposition the leads. Infection happens in 4-7% of cases. If you get redness, swelling, or fever near the implant site, call your doctor right away. You might need to remove the whole system and wait months before trying again. Battery replacement is another surgery. Every 5 to 9 years, you’ll need another operation to swap out the generator. Some newer models, like Boston Scientific’s WaveWriter Alpha™ Prime, last up to 24 months before needing a recharge. But recharging means plugging in a charger every night-something not everyone wants to do. And then there’s cost. Even with Medicare or insurance, you might pay $5,000-$10,000 out of pocket. The whole system-device, surgery, follow-ups-can run $25,000 to $45,000 in the U.S. That’s why many patients delay it until they’re desperate.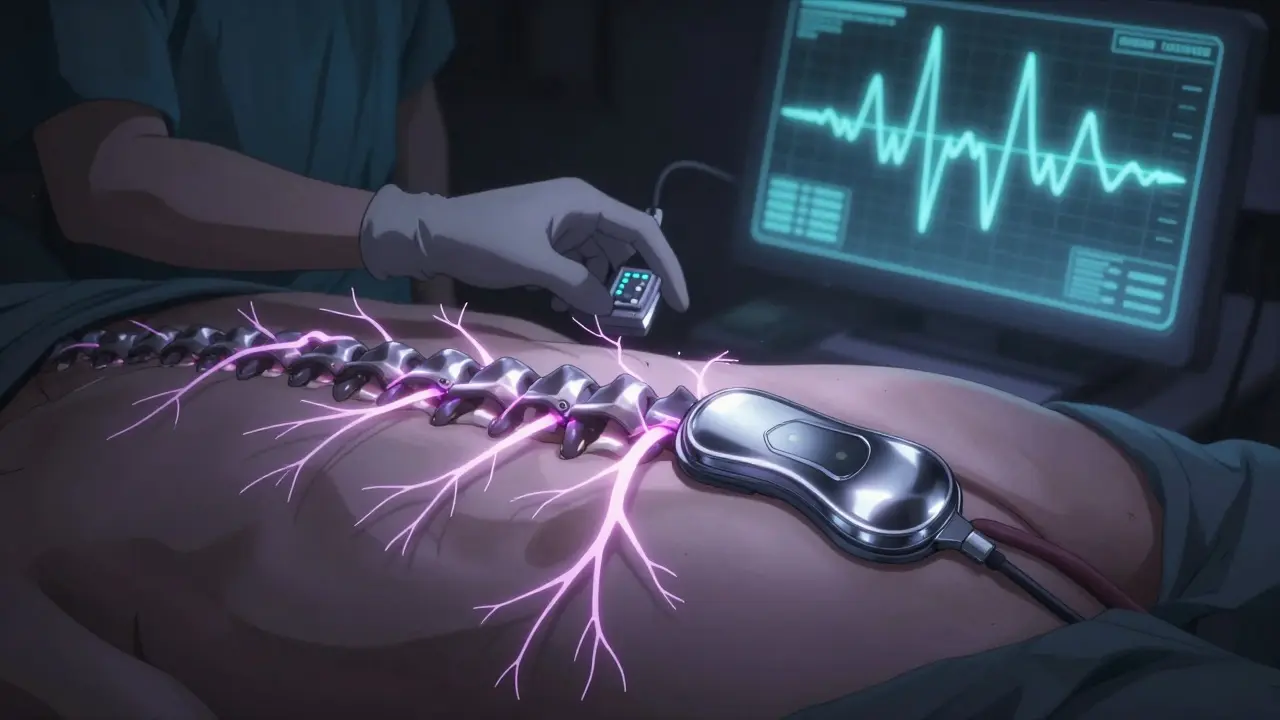
Real People, Real Results
On forums like Reddit and Healthgrades, stories vary. Some say SCS gave them back their life. One man, 67, said he went from using 6 oxycodone pills a day to zero. He walks his dog every morning now. Another woman, 52, said she could finally sleep through the night for the first time in 12 years. But others aren’t so lucky. One user on the r/ChronicPain subreddit said she had two revision surgeries in 18 months because the wires kept moving. Another complained his battery died after just 4 years, and his insurance wouldn’t cover the replacement until another year passed. The average rating across review sites is about 3.8 out of 5. Not perfect. But for people who’ve tried everything else? It’s often the best shot they’ve had.What’s Next for SCS
The future is getting smarter. New systems like Boston Scientific’s Evoke® are testing closed-loop technology-devices that adjust stimulation automatically based on your body’s signals. No more fiddling with the remote. The device learns your pain patterns and responds on its own. Medtronic’s Intellis™ 2, released in early 2023, senses when you stand up or lie down and changes the pulse strength to match your position. That’s a big deal for people whose pain changes with movement. And the market is growing fast. With an aging population and the opioid crisis still raging, SCS is becoming more common. Medicare approved it for more conditions in recent years, and insurers are slowly following. But here’s the catch: success still depends on picking the right person. If you’re not screened properly-physically or mentally-the odds of failure rise to over 40%. That’s why experts say: don’t rush. Get the trial. Talk to a pain psychologist. Make sure you understand the commitment.Final Thoughts
Spinal cord stimulation isn’t magic. It’s a tool. A powerful one, but only if used correctly. It doesn’t fix your spine. It doesn’t erase your pain history. But it can give you back control. The ability to walk without fear. To sleep without pills. To live without being defined by your pain. If you’ve been told there’s nothing else to try, ask about SCS. Get the trial. Talk to patients who’ve been through it. Learn what the device can-and can’t-do. And don’t let cost scare you off. Many insurance plans cover it. And if you qualify, the payoff-your life back-is worth more than any price tag.Is spinal cord stimulation the same as a pacemaker?
It works similarly in that both use implanted devices to send electrical signals. But a pacemaker regulates your heartbeat, while spinal cord stimulation blocks pain signals to your brain. The leads are placed in your back, not your chest, and the purpose is completely different.
Can I still get an MRI with a spinal cord stimulator?
Yes-but only with newer, MRI-conditional models. Systems like Boston Scientific’s Precision Montage™ or Medtronic’s Intellis™ 2 are designed to be safe under full-body 1.5T and 3.0T MRI scans. Older devices may only allow limited scans or none at all. Always check your device’s manual and talk to your doctor before scheduling an MRI.
Does SCS work for neuropathic pain in the hands or feet?
It can, but it’s less effective than for lower back or leg pain. For pain limited to the hands or feet, peripheral nerve stimulation (PNS) is often a better choice. SCS is strongest for pain that radiates from the spine-like sciatica or failed back surgery syndrome.
How long does it take to adjust to the device?
Most people need 2 to 4 weeks to get used to programming their stimulator. It’s not like flipping a switch-you’ll need to tweak settings for different activities: sitting, walking, sleeping. About 89% of patients need at least one follow-up visit with a specialist to fine-tune the settings.
Will I still need pain medications after SCS?
Many patients reduce or stop opioids entirely. One study showed 72% of SCS users achieved at least 50% pain relief without increasing meds. But you may still need occasional NSAIDs or nerve pain medications like gabapentin, especially in the first few months. SCS doesn’t replace all treatment-it reduces your dependence on drugs.
What happens if the device stops working?
If the stimulation fades or stops, it could mean the battery is low, the leads moved, or there’s a connection issue. First, check your remote and charging setup. If that doesn’t help, contact your pain clinic. You’ll likely need an X-ray or scan to check lead position. Most problems are fixable with a minor adjustment or replacement.






Lauren Wall
January 22, 2026 AT 05:49SCS isn't magic, but it's the only thing that didn't make me feel like a lab rat.
Ryan Riesterer
January 22, 2026 AT 12:16Neuromodulation via epidural leads modulates dorsal horn nociceptive transmission through gate control theory and supraspinal descending inhibition. Modern high-frequency waveforms (10 kHz) demonstrate superior efficacy over tonic stimulation in RCTs, with reduced paresthesia dependency. Lead migration remains the primary technical failure mode, occurring in 12-18% of cases within 6 months per ISNS guidelines.
Akriti Jain
January 23, 2026 AT 14:16They don't want you to know this... but SCS is just a fancy way to distract your brain while Big Pharma sells you a $40k gadget 😏💰
Next they'll implant microchips in your spine to make you buy more meds. #MindControl #SCSisACult
Malik Ronquillo
January 23, 2026 AT 21:20Look I get it, you’re desperate, but this isn’t a magic wand
People spend years chasing this thing then end up with wires moving and insurance denying the next battery
Just say no to expensive toys that make you feel like a cyborg
And no, I’m not mad, I just watched my cousin go through it
Chiraghuddin Qureshi
January 25, 2026 AT 18:13In India, this tech is still a luxury. Most people rely on Ayurveda or just endure. But I’ve seen patients in Bangalore who got SCS through NGO programs - life-changing. The real issue isn’t the device, it’s access. We need global equity in pain care, not just for the wealthy.
Also, the tingling? Feels like a gentle vibration from a temple bell. Not scary. Just… there.
Kenji Gaerlan
January 26, 2026 AT 04:11so u mean to say u put wires in ur spine and then u get to turn it on like a video game??
why dont u just take more tylenol lmao
Oren Prettyman
January 26, 2026 AT 22:51While the clinical literature suggests a statistically significant reduction in opioid consumption and improvement in functional outcomes, one must critically evaluate the methodological limitations inherent in the majority of prospective cohort studies cited, including selection bias, lack of long-term blinded controls, and conflating patient-reported outcomes with objective physiological metrics. Furthermore, the economic burden, though substantial, is often misrepresented as a barrier rather than a reflection of the resource-intensive nature of neurostimulatory interventions in a fee-for-service healthcare model.
Mike P
January 28, 2026 AT 07:22Y’all act like this is some newfangled scam. I got mine in ’19. No opioids. Walked my dog again. Slept through the night. My kid said I stopped yelling at the TV. That’s worth every penny.
And yeah, the battery died early - so what? I paid out of pocket. My pain didn’t wait for insurance.
This ain’t about being rich. It’s about being alive.
Liberty C
January 28, 2026 AT 12:14How tragic that we’ve reduced human suffering to a $45,000 hardware upgrade. You’re not healing - you’re outsourcing your biology to corporate tech. The real failure isn’t the device. It’s a medical system that lets chronic pain fester for years, then offers a $40k band-aid instead of addressing root causes: trauma, inflammation, systemic neglect.
SCS isn’t the future. It’s a symptom of our collapse.
Sarvesh CK
January 29, 2026 AT 07:06One cannot overlook the epistemological dimension of chronic pain - it is both physiological and phenomenological. The success of spinal cord stimulation, therefore, is not merely a matter of electrical impedance or lead placement, but of the patient’s subjective reintegration into a world that has long excluded them. The trial period, in this light, is not a diagnostic tool, but a hermeneutic space - a liminal threshold where the self is reconstituted through technological mediation. One must ask: does the device restore agency, or merely mask the absence of social and psychological support?
Hilary Miller
January 30, 2026 AT 08:11My mom got SCS last year. She’s 71. Now she dances in the kitchen. That’s all you need to know.
Margaret Khaemba
January 31, 2026 AT 23:28Does anyone know if these devices interfere with yoga poses? I do a lot of downward dog and was worried the leads might shift. Also, how’s the charging situation if you travel a lot?
Brenda King
February 2, 2026 AT 18:39Just want to say - if you’re reading this and thinking about the trial, please do it. Even if you’re scared. Even if you think it won’t work. The worst case? You take out the wires and go back to where you started.
But the best case? You get to hug your grandkid without crying.
You’re worth that chance.
And you’re not alone.