When you start taking opioids for chronic pain, you’re told to watch out for nausea, drowsiness, or dizziness. But one of the most common and frustrating side effects? Constipation. And it doesn’t go away. Unlike nausea, which fades after a few days, opioid-induced constipation (OIC) sticks around for as long as you’re on the medication. In fact, between 40% and 95% of people on long-term opioids develop it. That’s not rare. That’s the rule.
Why Opioids Make You Constipated (And Why Normal Laxatives Often Fail)
Opioids don’t just block pain signals in your brain-they also bind to receptors in your gut. These receptors control how fast food moves through your intestines, how much fluid gets absorbed, and how much mucus and digestive juices are produced. When opioids lock onto those receptors, your gut slows down. Everything gets stuck. Water gets sucked out of your stool. It becomes hard, dry, and painful to pass.
Here’s the catch: most people try to fix this the same way they’d fix regular constipation-eat more fiber, drink more water, take a stool softener. But that often makes things worse. Fiber ferments in a sluggish gut. That leads to bloating, gas, and even fecal impaction. A 2021 review in the Journal of Neurogastroenterology and Motility confirmed that high-fiber diets (like the standard 30g/day recommendation) can actually trigger discomfort in 25-40% of OIC patients. The American Pain Society now advises against routine high-fiber use for opioid users.
Standard laxatives like senna or bisacodyl work by stimulating the colon. But in OIC, the problem isn’t just slow movement-it’s a deep, opioid-driven shutdown of gut function. Studies show conventional laxatives only help about 25-50% of patients. That means more than half are stuck with painful, ineffective treatment.
What Works: First-Line Treatments That Actually Help
The best place to start isn’t with fancy drugs-it’s with simple, evidence-backed options that are safe and affordable.
- Polyethylene glycol (PEG) 3350 (like Miralax): This is the gold standard. It’s an osmotic laxative that pulls water into the bowel without irritating the gut. Dose: 17-34 grams daily. It’s gentle, doesn’t cause cramping like stimulants, and works even when the gut is sluggish. Multiple guidelines recommend it as the first choice.
- Bisacodyl (Dulcolax): A stimulant laxative. Use 5-15 mg daily. It kicks the colon into motion but can cause cramps if overused. Best for short-term use or when PEG isn’t enough.
- Senna: Another stimulant. 8.6-17.2 mg daily. Often combined with docusate (a stool softener), though evidence for docusate alone in OIC is weak.
Start with PEG. If after 3-5 days you’re still not having regular bowel movements, add a low dose of bisacodyl. Don’t wait. The earlier you act, the less likely you are to develop severe impaction or need hospitalization.
When Over-the-Counter Isn’t Enough: Prescription Options
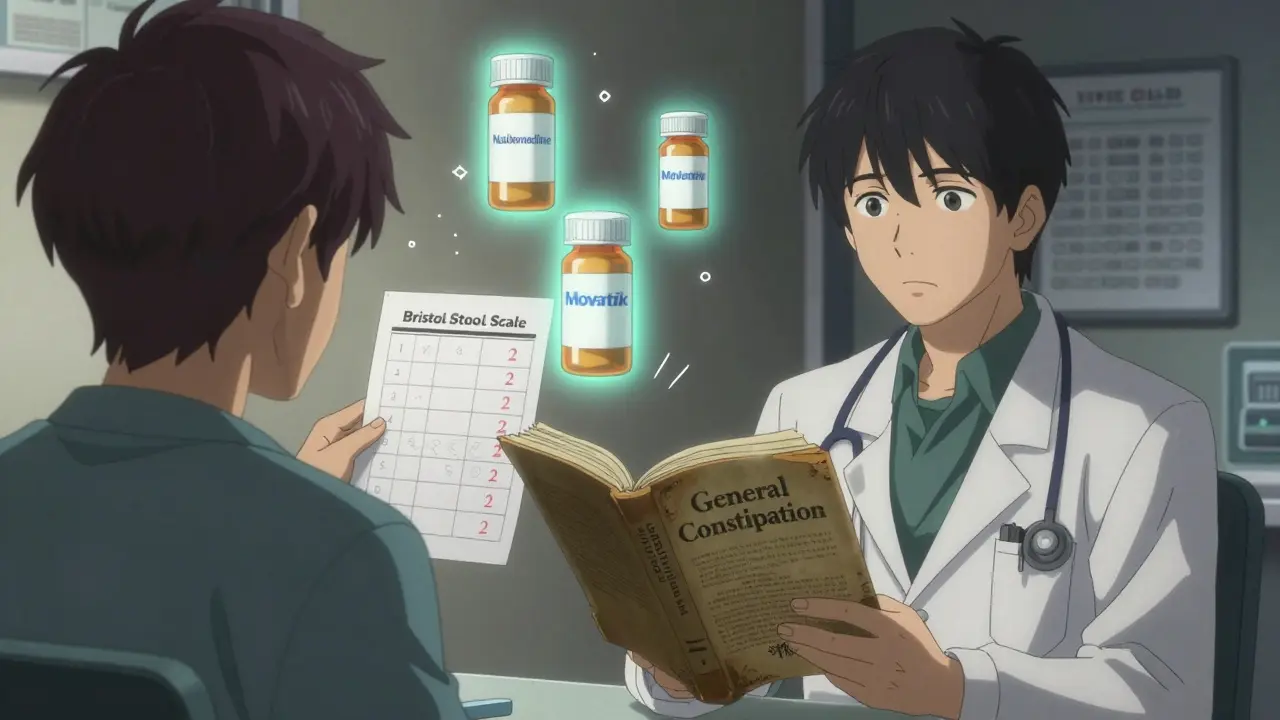
If you’ve tried PEG, bisacodyl, and senna-and still feel backed up-your body might need a different kind of help. That’s where peripherally acting μ-opioid receptor antagonists (PAMORAs) come in.
These drugs block opioids from acting on your gut receptors-without touching the pain relief in your brain. Because they don’t cross the blood-brain barrier well, your pain stays controlled, but your bowels wake up.
- Methylnaltrexone (Relistor®): Approved in 2008 for palliative care patients. Given as a daily injection under the skin. Works in as little as 30 minutes for some. But 47% of users report injection-site pain, and it costs $800-$1,200 a month. Often reserved for those with advanced illness.
- Naloxegol (Movantik®): An oral tablet taken once daily. Approved for chronic non-cancer pain. Works in 12-24 hours. Side effects: abdominal pain (20%), diarrhea (15%). Cost: $600-$900/month. Many insurers require trying PEG first.
- Naldemedine (Symcorza®): Also oral. Approved in 2017. Studies show 59% of users report moderate to significant improvement. Side effects: abdominal pain (38%), diarrhea (15%). Rated 6.8/10 by patients on Drugs.com. It’s one of the most tolerated PAMORAs.
Here’s the reality: PAMORAs aren’t magic. They don’t work for everyone. But when they do, they change lives. A 2023 review in Expert Review of Gastroenterology & Hepatology found response rates of 40-50% with PAMORAs versus 25-30% with placebo. That’s a real difference.
Lubiprostone: The Underused Option
Lubiprostone (Amitiza®) works differently. It activates chloride channels in the gut lining, pulling fluid into the bowel and making stool softer. Approved for OIC in 2013. But here’s the twist: it was initially approved only for women because early trials didn’t include enough men. Later data proved it works just as well in men. Still, many doctors don’t prescribe it to men because of outdated labeling.
Side effects? Nausea in about 30% of users. Diarrhea in 15-20%. It’s not a first-line choice, but for patients who can’t tolerate stimulants or PAMORAs, it’s a solid alternative. Dose: 24 mcg once daily.
What You Shouldn’t Do
Don’t increase your fiber. Seriously. If you’re on opioids, adding bran, psyllium, or whole grains might seem logical-but it’s a trap. Fiber needs movement to work. Opioids stop that movement. The result? Bloating, pain, and sometimes a dangerous blockage.
Don’t wait for symptoms to get bad. Many patients delay treatment until they haven’t had a bowel movement in 5-7 days. That’s too late. By then, stool is hardened and packed. Prevention beats rescue every time.
Don’t assume your doctor knows about OIC. A 2023 AMA survey found only 22-35% of community doctors use standardized tools to screen for constipation in opioid patients. Most still think, “Just take a laxative.” They don’t know about PAMORAs. They don’t know fiber can hurt. You might have to educate them.
How to Talk to Your Doctor
Bring this up at your next appointment:
- “I’ve been on opioids for X months, and I haven’t had a regular bowel movement in over 3 days.”
- “I’ve tried Miralax and senna, but they’re not working.”
- “I’ve read about PAMORAs like Movantik or Symcorza. Can we discuss if one’s right for me?”
- “Can we use the Bristol Stool Scale to track my progress?”
Ask for a bowel function assessment. The Bristol Stool Form Scale (a chart showing 7 stool types) is simple, free, and widely used. Type 1-2 means constipation. Type 3-4 is ideal. Type 5-7 is diarrhea. Track it weekly.
If your doctor says, “Just drink more water,” push back. That’s not enough. You need targeted treatment.
Real Patient Experiences
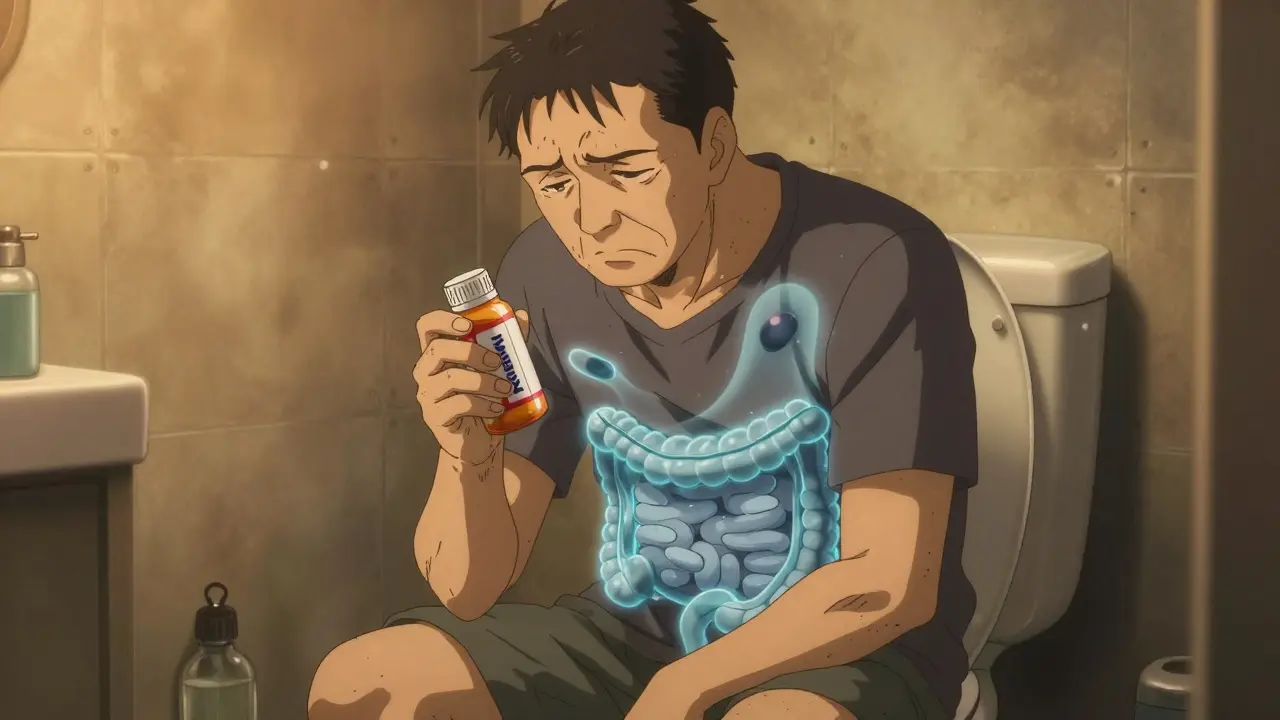
On Reddit’s r/ChronicPain, one user wrote: “I was on oxycodone for 18 months. I took Miralax every day. Nothing. Then my pain specialist switched me to naldemedine. Within 3 days, I had my first normal bowel movement in over a year. I cried.”
Another said: “Relistor worked fast-but the cost was insane. My insurance denied it twice. I had to appeal. Took 6 weeks. By then, I was in pain from impaction.”
These aren’t outliers. A 2022 survey in Pain Management Nursing found 73% of opioid users stopped at least one OIC treatment because it didn’t work-or made them feel worse.
What’s Coming Next
The future of OIC treatment is looking better. In March 2023, the FDA approved naldemedine for children as young as 10. That’s a big step.
Phase III trials are now testing a fixed-dose combo of naloxone (a weak opioid blocker) and polyethylene glycol. The idea? One pill that softens stool and reverses gut slowdown. Results are expected in mid-2024.
Meanwhile, the global market for OIC treatments is projected to hit $3.4 billion by 2028. More options are coming. But for now, you still have to fight for them.
Bottom Line: You Don’t Have to Suffer
Opioid-induced constipation isn’t something you just have to live with. It’s a medical problem with proven solutions. Start with polyethylene glycol. Don’t add fiber. Track your stools. If that doesn’t work after a week, ask for a PAMORA. Naldemedine is often the best balance of effectiveness and tolerability. Methylnaltrexone works fast but costs more and requires shots. Lubiprostone is underused but valid.
And if your doctor doesn’t know about these options? Bring the research. Show them the guidelines. Your quality of life matters as much as your pain control. You deserve both.”
Can I just take more fiber to fix opioid-induced constipation?
No. Increasing fiber intake is not recommended for opioid-induced constipation (OIC). While fiber helps with general constipation, opioids slow gut movement so much that fiber ferments in the colon, causing bloating, gas, and even fecal impaction. Studies show 25-40% of OIC patients get worse symptoms with high-fiber diets. The American Pain Society and other guidelines now advise against routine fiber increases for opioid users.
What’s the best over-the-counter laxative for opioid-induced constipation?
Polyethylene glycol (PEG) 3350, sold as Miralax, is the most effective and safest first-line OTC option. It draws water into the colon without irritating the gut, making stools softer and easier to pass. Dose: 17-34 grams daily. Unlike stimulant laxatives (like senna or bisacodyl), PEG doesn’t cause cramping and works even when gut motility is suppressed by opioids.
Do PAMORAs stop pain relief from opioids?
No. PAMORAs (like naldemedine, naloxegol, and methylnaltrexone) are designed to block opioid receptors only in the gut-not in the brain. Because they don’t cross the blood-brain barrier effectively, they reverse constipation without reducing pain control. This is why they’re preferred over other treatments when standard laxatives fail.
How long does it take for PAMORAs to work?
It varies. Methylnaltrexone (injection) can work in as little as 30 minutes. Oral options like naloxegol and naldemedine usually take 12-24 hours. Most patients report a bowel movement within 24-48 hours of starting treatment. Consistent daily dosing is key-these aren’t rescue medications, they’re maintenance.
Why do some doctors not treat OIC properly?
Many doctors still think OIC is just “normal” constipation and recommend generic advice like “eat more fiber” or “drink water.” A 2023 AMA survey found only 22-35% of community providers use standardized tools to assess bowel function in opioid patients. Awareness of PAMORAs and updated guidelines is low outside of pain clinics. Patients often need to bring research or ask specifically about options like naldemedine or Movantik.
Is it safe to use PAMORAs long-term?
Yes. Clinical trials lasting up to 12 months show naldemedine and naloxegol are safe for long-term use in chronic non-cancer pain patients. Side effects like abdominal pain and diarrhea are usually mild and decrease over time. The FDA has approved these drugs for ongoing use, and they’re not addictive. The main concern is cost and insurance barriers-not safety.
What should I do if my laxatives aren’t working?
If you’ve taken polyethylene glycol daily for 5-7 days with no improvement, talk to your doctor about switching to a PAMORA. Don’t increase the dose of stimulant laxatives-this can cause cramping or dependency. Keep a bowel diary using the Bristol Stool Scale. Show your doctor your progress (or lack of it). If they refuse to consider PAMORAs, ask for a referral to a gastroenterologist or pain specialist.





Mussin Machhour
December 24, 2025 AT 17:53Just wanted to say this post saved my life. Been on oxycodone for 3 years and thought I was just stuck with the misery. Started with Miralax like you said, then added naldemedine after a week. First normal BM in over a year. No more crying in the bathroom. Thank you.
Sophie Stallkind
December 26, 2025 AT 15:48Thank you for this meticulously researched and clinically grounded exposition. The distinction between centrally and peripherally acting agents is not only scientifically accurate but also profoundly empathetic to the lived experience of chronic pain patients. I shall be sharing this with my department as a reference document.
Lindsay Hensel
December 27, 2025 AT 03:06I cried reading this. Not because I’m sad-because someone finally said it out loud: you don’t have to suffer. And that’s not just medical advice. It’s a human right.
Jason Jasper
December 28, 2025 AT 05:39PEG works. I’ve tried everything. Senna made me feel like I was being gut-punched. Miralax? Just… works. No drama. No panic. Just a quiet, gentle relief. I wish more doctors knew this.
Winni Victor
December 29, 2025 AT 10:55So now we’re supposed to trust Big Pharma’s $900/month miracle pill over fiber? Next they’ll tell us to inject caffeine into our colon. This is all just a money grab. I’m going back to prune juice and a hot water bottle. And no, I don’t care what the ‘guidelines’ say.
Justin James
December 30, 2025 AT 20:07Let me tell you what they don’t want you to know. Opioid constipation? It’s not just the drugs. It’s the glyphosate in your bread, the fluoride in your water, and the fact that the FDA approved PAMORAs because the pharmaceutical lobby paid off the review board. They don’t want you to know that fiber works if you do it right-just not the way they sell it. The gut microbiome is a complex ecosystem, and they’re poisoning it with synthetic laxatives while hiding the real solution: detox protocols, colonics, and magnesium chloride. I’ve been off opioids for 2 years and I still use this. No pills. No injections. Just raw garlic, Epsom salt baths, and cold showers. The system is rigged. Wake up.
Oluwatosin Ayodele
December 31, 2025 AT 16:31You Americans think you invented medicine. In Nigeria, we’ve been treating opioid constipation with papaya seeds, ginger tea, and a daily walk since the 1980s. You pay $800 for a pill? We use what grows in the backyard. Your ‘evidence-based’ guidelines are just colonial science repackaged. Read the WHO’s 1997 report on traditional remedies for GI motility. It’s all there. You just chose to ignore it because it doesn’t have a patent.
Harbans Singh
January 2, 2026 AT 09:27As someone who’s been on long-term opioids after a spinal injury, I can say this: PEG + naldemedine changed everything. I used to avoid leaving the house because I was scared of being stuck. Now I go to the park with my kids. The real win? My doctor finally listened when I showed him the Bristol chart. We track it every Sunday. It’s not glamorous-but it’s real. If you’re reading this and still stuck? Don’t give up. You’re not broken. The system is just slow.
Zabihullah Saleh
January 2, 2026 AT 21:24There’s a quiet dignity in suffering with dignity. We don’t talk about this enough-how constipation steals your sense of self. You stop being a person and become a symptom. This post doesn’t just list drugs. It says: you’re still whole. Even when your gut won’t move. Even when your doctor shrugs. You’re not a burden. You’re a human being who deserves relief. And that’s the most powerful prescription of all.