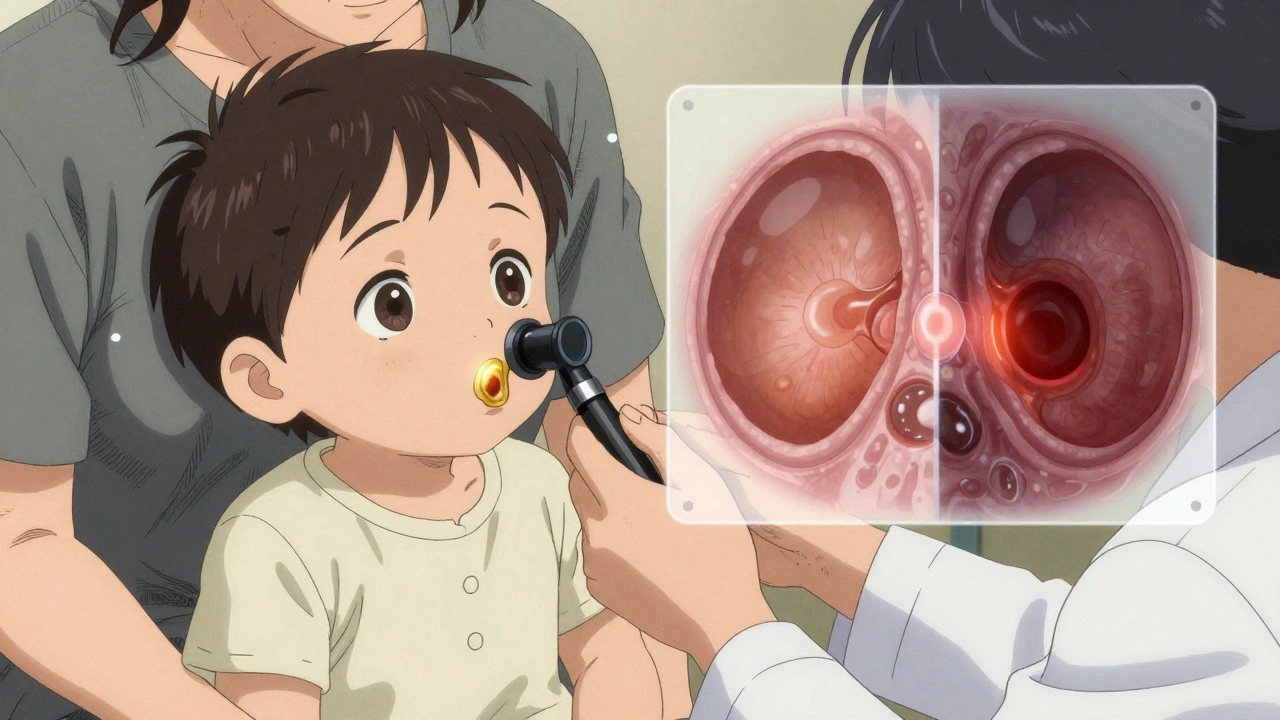
More than 80% of kids will have at least one ear infection by their third birthday. It’s one of the most common reasons parents rush to the doctor - the crying, the tugging at the ear, the fever that comes out of nowhere. But here’s the thing: otitis media doesn’t always need antibiotics. In fact, many ear infections get better on their own.
What Exactly Is Otitis Media?
Otitis media means inflammation or infection behind the eardrum. It’s not just an "earache" - it’s fluid trapped in the middle ear, often because the Eustachian tube, which drains fluid from the ear to the throat, gets blocked. That happens after a cold, allergies, or a respiratory infection. In kids, this is extra common because their tubes are shorter, more horizontal, and still developing. That makes it harder for fluid to drain, and easier for bacteria or viruses to grow. There are two main types: acute otitis media (AOM), which is the painful, infected version with fever and red, bulging eardrums, and otitis media with effusion (OME), which is just fluid sitting there after the infection clears. OME usually doesn’t hurt and often goes away on its own within a few weeks. But AOM? That’s when things get serious - and when treatment decisions matter.What Causes It?
Bacteria are the usual suspects: Streptococcus pneumoniae, Haemophilus influenzae (non-typeable), and Moraxella catarrhalis. Viruses like the common cold, flu, and RSV can also trigger it. But it’s not just about germs. Risk factors play a big role. Kids in daycare? They’re two to three times more likely to get ear infections. Exposure to cigarette smoke? That raises the risk by about 50%. Bottle-feeding while lying down? That can let milk or formula flow into the Eustachian tube. And if your child hasn’t had the pneumococcal vaccine (PCV13 or the newer 15-valent version), they’re more vulnerable to the most common bacterial strains.How Do You Know It’s an Ear Infection?
Parents often think tugging at the ear means infection. But that’s not always true. A child might tug because their ear is itchy or they’re tired. Real signs of acute otitis media include:- Fever over 38.5°C (101.3°F)
- Severe ear pain that doesn’t improve with painkillers
- Fluid draining from the ear (that’s a ruptured eardrum - it sounds scary, but it often relieves pressure and pain)
- Irritability, trouble sleeping, or loss of appetite in babies
- Balance issues or dizziness in older kids
Antibiotics: When They Help - and When They Don’t
Here’s the big shift in medical thinking: most ear infections don’t need antibiotics. The American Academy of Pediatrics and the American Academy of Family Physicians say that about 80% of uncomplicated cases resolve on their own within 2-3 days. So when do you really need them?- Children under 6 months - always treat with antibiotics. Their immune systems aren’t ready to fight it alone.
- Children 6 to 23 months - antibiotics if symptoms are severe (fever over 39°C / 102.2°F, pain lasting more than 48 hours) or if both ears are infected.
- Children 2 years and older - if symptoms are mild (low fever, mild pain), watch and wait for 48-72 hours. If no improvement, then start antibiotics.
Pain Management Is the First Step
Before you even think about antibiotics, focus on pain relief. That’s what matters most to your child.- Ibuprofen (5-10 mg/kg every 6-8 hours) - works well for both pain and fever.
- Acetaminophen (10-15 mg/kg every 4-6 hours) - good alternative if ibuprofen isn’t suitable.
- Warm compress on the ear - helps soothe discomfort.
- Otic drops like Auralgan - only if the eardrum isn’t ruptured. Never use them if you see fluid draining.
Watchful Waiting: What It Really Means
"Watchful waiting" doesn’t mean "do nothing." It means:- Start pain relief immediately.
- Monitor for red flags: fever above 104°F, worsening pain, swelling behind the ear, facial drooping, or pus draining from the ear.
- Call the doctor if symptoms don’t improve after 48 hours - or if they get worse.
- Don’t panic if the fever lingers for 2-3 days. That’s normal.
What About Recurrent Infections?
If your child gets three or more ear infections in six months, or four in a year, that’s recurrent otitis media. This can be frustrating - and it often leads to repeated antibiotic courses. In these cases, doctors may consider:- Ear tubes (tympanostomy tubes) - small tubes placed in the eardrum to help drain fluid and prevent buildup.
- Long-term low-dose antibiotics - rarely used now, due to resistance risks.
- Checking for underlying issues like allergies or immune problems.
- Ensuring full vaccination with PCV13 or the newer 15-valent vaccine.

What Doesn’t Work
There’s a lot of misinformation out there.- Probiotics - multiple studies, including a 2022 Cochrane review of over 3,400 kids, found no clear benefit in preventing ear infections.
- Antibiotics for fluid-only (OME) - if there’s no infection, antibiotics won’t help. The fluid will clear on its own, usually within 3 months.
- Home remedies like garlic oil or ear candles - no scientific backing. Ear candles can burn the ear canal. Avoid them.
What’s Changing in Treatment?
New tools are making diagnosis faster and more accurate. The FDA approved the CellScope Oto - a smartphone attachment that lets parents take pictures of the eardrum and send them to their doctor. Studies show it’s 85% accurate compared to in-person exams. In the next few years, point-of-care tests that identify bacteria in minutes could replace guesswork. One expert predicts these will cut broad-spectrum antibiotic use by 30-40% within five years. And resistance? It’s climbing. Haemophilus influenzae is becoming less responsive to amoxicillin-clavulanate (Augmentin). That’s why doctors are moving away from "just in case" prescriptions and toward smarter, targeted use.When to Seek Help Right Away
Call your doctor or go to urgent care if your child has:- Fever above 104°F
- Pain that doesn’t improve with ibuprofen
- Fluid or pus draining from the ear
- Swelling behind the ear
- Dizziness, vomiting, or stiff neck
- Facial weakness or drooping
Final Thoughts: Balance Is Key
Otitis media is common. But it’s not always an emergency. The goal isn’t to avoid antibiotics completely - it’s to use them wisely. Pain relief first. Observation for mild cases. Antibiotics only when the evidence says they’ll help. It’s not about being "natural" or "anti-medical." It’s about protecting your child from unnecessary side effects - like diarrhea, rashes, and yeast infections - while also protecting the future by slowing antibiotic resistance. Your child’s body is capable of healing. Sometimes, all it needs is time, comfort, and a little patience.Do all ear infections need antibiotics?
No. About 80% of acute ear infections in children resolve on their own within 2-3 days without antibiotics. Doctors now recommend watchful waiting for mild cases, especially in kids over 2 years old. Antibiotics are reserved for severe symptoms, very young children, or if symptoms don’t improve after 48-72 hours.
What’s the best medicine for ear infection pain?
Ibuprofen (5-10 mg/kg every 6-8 hours) is usually the most effective because it reduces both pain and inflammation. Acetaminophen (10-15 mg/kg every 4-6 hours) works well too, especially if ibuprofen isn’t suitable. Warm compresses and avoiding lying flat during feeding can also help reduce pressure and discomfort.
Is amoxicillin still the best antibiotic for ear infections?
Yes, for most cases. High-dose amoxicillin (80-90 mg/kg/day) remains the first-line treatment because even with rising resistance, most bacteria still respond to it. Augmentin (amoxicillin-clavulanate) is used if amoxicillin fails or if the child has had repeated infections. Avoid older antibiotics like erythromycin or sulfonamides - they’re less effective.
Can ear infections cause hearing loss?
Yes, temporarily. Fluid behind the eardrum can cause mild conductive hearing loss of 15-40 decibels, which may make a child seem unresponsive or like they’re not paying attention. This usually clears up once the infection resolves. Persistent fluid for more than 3 months may need further evaluation, especially if it affects speech development.
How can I prevent ear infections in my child?
Vaccination is the biggest preventive step - make sure your child gets the pneumococcal vaccine (PCV13 or 15-valent). Breastfeed if possible, avoid bottle-feeding while lying down, keep them away from secondhand smoke, and limit daycare exposure if they’re prone to infections. Regular handwashing and avoiding sick contacts also help reduce colds, which often lead to ear infections.
What if my child keeps getting ear infections?
If your child has three or more infections in six months, talk to your pediatrician or an ENT specialist. They may recommend ear tubes (tympanostomy tubes) to help drain fluid and prevent buildup. Other steps include checking for allergies, ensuring full vaccination, and reviewing exposure to smoke or daycare settings. Long-term antibiotics are rarely recommended anymore due to resistance risks.






Iris Carmen
December 9, 2025 AT 21:06Shubham Mathur
December 11, 2025 AT 10:54Stacy Tolbert
December 11, 2025 AT 19:05Ronald Ezamaru
December 11, 2025 AT 20:05Ryan Brady
December 13, 2025 AT 07:44Raja Herbal
December 13, 2025 AT 23:48Rich Paul
December 15, 2025 AT 15:27Katherine Rodgers
December 16, 2025 AT 00:19Taya Rtichsheva
December 16, 2025 AT 18:58Christian Landry
December 16, 2025 AT 21:33Guylaine Lapointe
December 18, 2025 AT 10:26Evelyn Pastrana
December 18, 2025 AT 17:43Brianna Black
December 20, 2025 AT 00:36