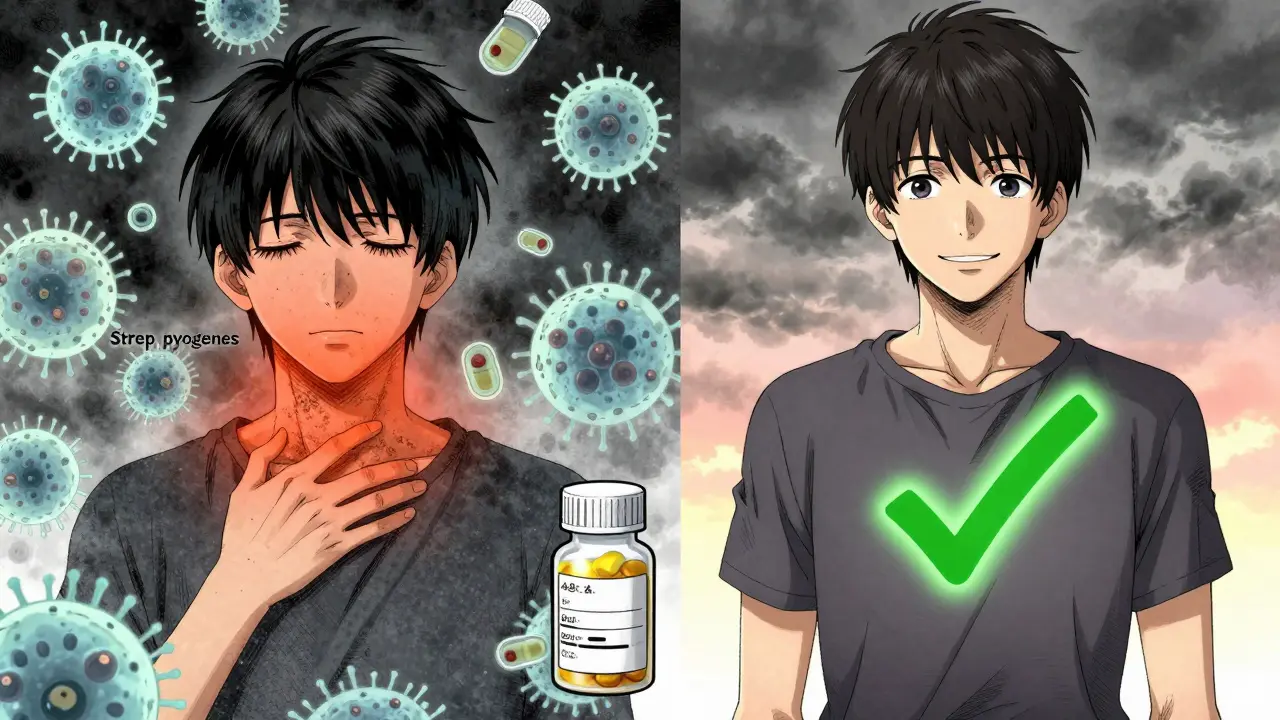
Strep throat isn’t just a bad sore throat. It’s a bacterial infection that can turn dangerous if ignored. You wake up with a throat that feels like sandpaper, a fever that won’t break, and no cough - that’s the classic sign. But here’s the catch: most sore throats are viral. If you treat them like strep, you’re adding to antibiotic resistance. If you ignore real strep, you risk rheumatic fever - a condition that can damage your heart. So how do you know for sure? And what happens once you start treatment?
How Doctors Diagnose Strep Throat
< p>Not every sore throat is strep. In fact, up to 85% of adult sore throats are caused by viruses like colds or flu. So doctors don’t just guess. They use a mix of symptoms and tests.The first clue is what’s not there. If you have a runny nose, cough, or red eyes, it’s probably not strep. Strep throat hits fast: sudden pain, fever over 100.4°F, swollen tonsils with white patches, and tender neck glands. No cough. No sneezing. That’s the pattern.
Doctors use the Centor score to estimate your risk: one point each for no cough, fever, swollen lymph nodes, and tonsil exudate. A score of 3 or higher means you’re likely to have strep - and need a test.
The go-to test is the rapid antigen detection test (RADT). A swab from your throat gives results in 10 to 30 minutes. It’s 95% accurate at spotting strep when it’s there - but it can miss 5-15% of cases. That’s why, especially in kids and teens, a negative RADT is followed by a throat culture. The culture takes 1-2 days but catches nearly all infections. It’s the gold standard.
More clinics are now using PCR tests, which are even more sensitive. They’re accurate in 95-98% of cases, but take longer and cost more. Right now, RADT is still the first step for most patients. The CDC recommends confirming negative RADT results in children and teens because their risk of complications is higher.
Which Antibiotics Actually Work
Once strep is confirmed, antibiotics are non-negotiable. Not because they make you feel better faster (they do, but only by about a day), but because they stop the infection from spreading and prevent serious complications.
The first-line treatment? Penicillin or amoxicillin. Both are cheap, safe, and effective. For adults, penicillin V is 500 mg twice a day for 10 days. Kids get lower doses based on weight. Amoxicillin is often preferred for kids because it tastes better and is taken once a day. Both clear the bacteria in 95% of cases when taken fully.
If you’re allergic to penicillin, options include cephalexin, clindamycin, or azithromycin. But here’s the problem: resistance is creeping in. Macrolides like azithromycin have up to 15% resistance in some areas. Clindamycin resistance is rising too - up to 10% in certain communities. So doctors don’t just pick the first alternative. They consider local resistance patterns.
Antibiotics start working fast. Within 24 hours, you’re no longer contagious. That’s why you can go back to school or work after a full day on antibiotics - if your fever is gone. But you still have to finish the full 10-day course. Stopping early? That’s how relapses happen. About 5-15% of people who quit early get strep again.
And don’t use leftover antibiotics. A CDC survey found 12% of people do this. It’s dangerous. The dose might be wrong. The drug might not even be for strep. And it fuels antibiotic resistance. The WHO says 30% of outpatient antibiotics are unnecessary. Strep throat is one of the most common reasons for that mistake.

What to Expect During Recovery
With antibiotics, you’ll feel better fast. Most people notice improvement within 24 to 48 hours. The throat pain eases. The fever drops. Swallowing gets easier. That’s not magic - it’s the antibiotics killing the bacteria.
Complete recovery takes 7 to 10 days. Even if you feel fine after day 3, keep taking the pills. Relapse is real. And if symptoms don’t improve after 48 hours of antibiotics, you need to go back. It could mean the wrong antibiotic, a different infection, or a complication like a peritonsillar abscess - a pocket of pus behind the tonsil that happens in 1-2% of cases.
Without treatment, strep throat lasts about the same time - 7 to 10 days. But here’s the difference: you’re contagious the whole time. You’re spreading bacteria to family, coworkers, classmates. And your risk of rheumatic fever - which can permanently damage heart valves - jumps to about 3%. That’s why antibiotics aren’t optional. They’re preventive.
Children under 3 rarely get strep. Their immune systems don’t react the same way. So if your toddler has a sore throat, it’s almost certainly viral. Don’t push for a test unless there are other red flags.
When to Worry - Red Flags and Complications
Most people recover without issue. But some signs mean you need help right away.
- Difficulty breathing or swallowing - could mean swelling or an abscess
- High fever that comes back after improving
- Rash - especially a sandpaper-like one - could be scarlet fever, a complication of strep
- Joint pain, chest pain, or irregular heartbeat - signs of rheumatic fever
- Abdominal pain or vomiting - more common in kids, sometimes mistaken for stomach flu
These aren’t rare. About 15% of patients present with atypical symptoms. Abdominal pain in kids, for example, can delay diagnosis. Parents think it’s food poisoning. Doctors think it’s gastroenteritis. But if the sore throat is there too - test for strep.
And don’t ignore lingering symptoms. If your throat still hurts after 10 days of antibiotics, you might have a secondary infection, or the bacteria didn’t fully clear. Repeat testing or a different antibiotic may be needed.
Common Mistakes and How to Avoid Them
People make the same mistakes over and over.
- Stopping antibiotics early: 40% of parents do this when their child seems better. But the infection isn’t gone. Relapse rates jump from 5% to 25% with partial treatment.
- Sharing meds: A Reddit thread from January 2024 found 8% of adults have given leftover antibiotics to family members. That’s how resistant strains spread.
- Testing too late: Antibiotics only prevent rheumatic fever if started within 9 days of symptoms. Waiting a week? You’ve missed the window.
- Testing everyone: If you have a cough and runny nose, you don’t need a strep test. It’s a waste of time and money. The CDC estimates 15 million outpatient visits for sore throats every year - many unnecessary.
Also, don’t use home remedies as a substitute. Honey and salt water help with discomfort, but they don’t kill bacteria. Antibiotics are the only thing that stops the infection from spreading.
What’s New in 2025
Things are changing. In March 2024, the FDA approved a new rapid molecular test called Strep Ultra. It gives results in 15 minutes with 98% accuracy - close to lab-grade PCR. It’s already showing up in urgent care centers and may replace traditional rapid tests soon.
The CDC is spending $15 million to track antibiotic resistance patterns. Meanwhile, researchers are testing whether a 5-day antibiotic course works as well as 10 days. Early results from a multi-center trial (NCT05678901) look promising. If confirmed, shorter courses could improve compliance and cut down on side effects.
But a vaccine? Still far off. Streptococcus pyogenes has over 200 strains. Making one vaccine that covers them all is like trying to hit 200 moving targets at once. For now, the best defense is smart testing and full antibiotic courses.
Strep throat is simple - but only if you treat it right. Test when needed. Take the full course. Don’t share pills. And don’t assume every sore throat is strep. That’s how you protect yourself, your kids, and the effectiveness of antibiotics for everyone.
Can you have strep throat without a fever?
Yes, but it’s uncommon. Fever is present in about 85% of confirmed strep cases. If you have a sore throat with no fever, it’s more likely viral. However, some adults - especially those with weaker immune systems - may have strep without a fever. If other signs are strong (no cough, swollen glands, white patches), testing is still recommended.
How long is strep throat contagious?
Without antibiotics, you’re contagious for up to 10 days. Once you start antibiotics, you’re no longer contagious after 24 hours - as long as your fever is gone. That’s why kids can return to school after one full day on antibiotics. But if you skip the meds, you’re spreading the bacteria for the whole duration of the illness.
Do you need a test if you have a sore throat?
Not always. If you have a cough, runny nose, hoarseness, or pink eyes, it’s probably viral - and you don’t need a strep test. Tests are recommended when you have sudden throat pain, fever, swollen tonsils with white patches, and no cough. The CDC advises testing children and teens with these symptoms, but not adults with clear viral signs.
Can strep throat come back after treatment?
Yes, but usually because the full antibiotic course wasn’t taken. About 5-15% of people who stop early get strep again. It can also happen if you’re re-exposed to someone still contagious. Rarely, you may carry the bacteria without symptoms and reinfect yourself or others. That’s why finishing all your pills matters - even if you feel fine.
Is strep throat more common in winter?
Yes. Strep throat peaks between November and April, with up to 30% more cases during winter months. Crowded indoor spaces, dry air, and school settings help the bacteria spread. That’s why outbreaks are common in classrooms and daycare centers. Cases are rare in summer, but climate change is causing a 12% increase in off-season cases, according to 2023 data.
Can you get strep throat from pets?
No. Group A Streptococcus only spreads between people - through coughs, sneezes, or sharing utensils. Pets don’t carry or transmit human strep. If your child gets strep after being around a dog or cat, it came from another person, not the pet.
What if I’m allergic to penicillin but the alternative antibiotics don’t work?
If first-line alternatives like cephalexin or azithromycin fail, your doctor may switch to clindamycin or a different class like a macrolide with lower resistance in your area. In rare cases, a throat culture and sensitivity test can identify which antibiotics the specific strain responds to. For severe or recurrent cases, an infectious disease specialist may be consulted.
Why not just treat everyone with antibiotics just in case?
Because most sore throats are viral. Antibiotics don’t help viruses - and they harm you. Every unnecessary dose increases the risk of side effects like diarrhea, yeast infections, and allergic reactions. More importantly, it fuels antibiotic resistance. The CDC says 30% of outpatient antibiotics are unnecessary. Treating without testing could make strep harder to treat for everyone in the future.






Adrienne Dagg
December 19, 2025 AT 04:44Glen Arreglo
December 19, 2025 AT 08:50shivam seo
December 20, 2025 AT 14:17benchidelle rivera
December 22, 2025 AT 14:03Andrew Kelly
December 22, 2025 AT 15:53Isabel Rábago
December 24, 2025 AT 02:23Anna Sedervay
December 24, 2025 AT 04:54Mike Rengifo
December 24, 2025 AT 22:22Ashley Bliss
December 26, 2025 AT 17:58Dev Sawner
December 27, 2025 AT 04:48Moses Odumbe
December 27, 2025 AT 15:02