After a kidney transplant, your body doesn’t know the new organ isn’t a threat. It sees it as an invader and tries to attack it. That’s where tacrolimus, mycophenolate, and steroids come in. Together, they form the most common immunosuppression plan used worldwide-used in about 7 out of 10 new kidney transplant patients. But this isn’t just about popping pills. It’s about balancing survival and side effects, day after day, year after year.
Why This Three-Drug Combo Exists
Before the late 1990s, most transplant patients got cyclosporine, steroids, and azathioprine. It worked, but rejection rates were high-over 20% in the first year. Then came tacrolimus and mycophenolate mofetil (MMF). These drugs were more powerful, more targeted, and had fewer cosmetic side effects than cyclosporine. By the early 2000s, studies showed that adding mycophenolate to tacrolimus and steroids slashed acute rejection rates from 21% down to just 8.2%. That’s a 61% drop. Suddenly, this triple combo became the gold standard.It’s not magic. Each drug hits a different part of the immune system. Tacrolimus blocks T-cells from sounding the alarm. Mycophenolate stops them from multiplying. Steroids calm the whole system down like a fire extinguisher. Together, they’re stronger than any two alone. That’s why even today, despite new drugs and smarter monitoring, this trio still dominates transplant centers across the U.S. and Europe.
How Each Drug Works-And What It Does to Your Body
Tacrolimus (also called FK506) is the backbone. You take it twice a day, usually with food or without-your doctor will tell you which. It starts working within 12 to 24 hours. But here’s the catch: your body absorbs it differently every day. One day, you might need 5 mg. The next, 7 mg. That’s why blood tests are non-negotiable. Doctors track your trough level-the lowest concentration in your blood before your next dose. For the first year after transplant, that number should stay between 5 and 10 ng/mL. Too low? Rejection risk spikes. Too high? You risk kidney damage, tremors, headaches, or even diabetes.
Mycophenolate mofetil (MMF) is the second pillar. It’s taken as a pill, usually 1 gram twice a day. It stops immune cells from making DNA, so they can’t multiply. Simple. Effective. But it’s rough on the stomach. About 25 to 30% of patients get diarrhea, nausea, or vomiting. About 15% develop low white blood cell counts (leukopenia), which raises infection risk. Many people end up cutting their dose to 500 mg twice a day-or stopping it altogether. That’s not failure. It’s adaptation. Your body tells you what it can handle.
Steroids-usually prednisone or methylprednisolone-are the quick fix. You get a big IV dose (1,000 mg) right in the operating room. Then, over the next few weeks, doctors slowly turn it down. By week 3 or 4, you’re on 15 mg a day. By 2 to 3 months, it’s 10 mg. Some patients stay on this for life. Others get weaned off completely. Steroids cause weight gain, acne, mood swings, and higher blood sugar. They also increase your risk of osteoporosis and cataracts. That’s why so many doctors now try to ditch them entirely if they can.
When Steroids Can Be Dropped
For years, steroids were mandatory. But in 2005, a major study showed something surprising: patients who skipped steroids entirely-using tacrolimus, mycophenolate, and an induction drug called daclizumab-had the same rejection rates as those who took steroids. That’s when the game changed.
Today, about 1 in 3 transplant centers offer steroid-free regimens for low-risk patients: younger recipients, those with no history of rejection, or those who can’t tolerate steroids. About 89% of those patients stayed steroid-free at six months. No more moon face. No more belly fat. No more sleepless nights from anxiety. But it’s not for everyone. High-risk patients-those who got a kidney from a deceased donor, or who had previous transplants-still need steroids. The risk of rejection is too high without them.
Even when steroids are stopped, the first 3 months are critical. You’re still vulnerable. That’s why your doctor watches you like a hawk during this time. Blood tests. Ultrasounds. Biopsies if something looks off. It’s not paranoia-it’s protection.

The Hidden Costs: Side Effects You Can’t Ignore
This combo saves lives. But it doesn’t come free.
One in five people on this regimen develops post-transplant diabetes. That’s 18 to 21%. Tacrolimus messes with insulin production. Steroids make your body ignore insulin. Together, they turn your pancreas into a broken machine. You might need metformin. Or insulin. Or both. And once you’re on it, you’re often on it for life.
Then there’s kidney toxicity. Tacrolimus is great at stopping rejection-but it can also slowly damage the very organ it’s trying to protect. That’s why your kidney function (creatinine, eGFR) is checked every week at first, then monthly. If your numbers creep up, your dose gets lowered. It’s a tightrope walk.
Infections are the silent enemy. You’re more likely to get CMV (cytomegalovirus), urinary tract infections, or even pneumonia. That’s why you get antiviral pills for the first 3 to 6 months. Why you’re told to avoid crowds in winter. Why your doctor checks your blood for signs of trouble before you even feel sick.
And then there’s the long game: chronic allograft injury. Even if you don’t reject the kidney in year one, it can still slowly fail over time. The immune system doesn’t always attack with a bang-it whispers. And right now, no drug combo stops that whisper completely. That’s why 25% of adult kidney transplant patients end up back on dialysis within five years.
Monitoring: It’s Not Just About Blood Tests
For years, doctors only checked your trough level-the lowest point of drug concentration in your blood before your next dose. But that’s like guessing how much gas is in your tank by looking at the needle at 6 a.m. after you’ve driven 100 miles. It’s not accurate.
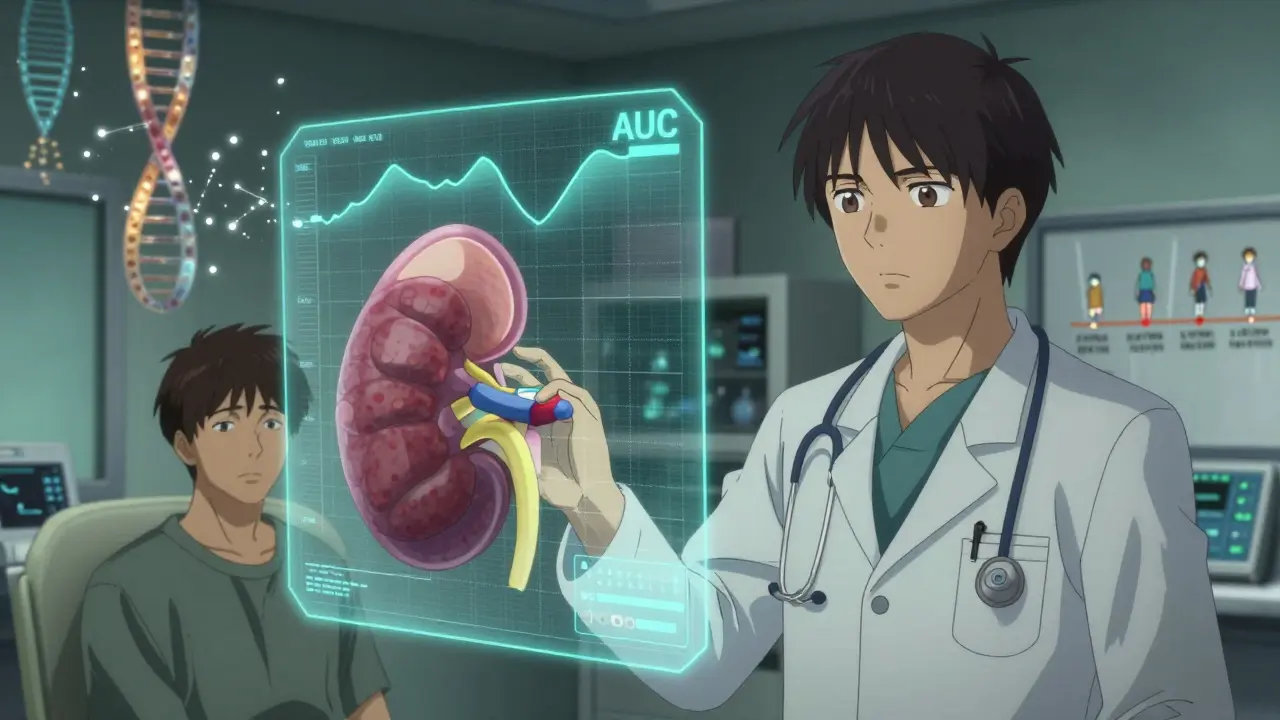
Now, top centers use AUC monitoring-Area Under the Curve. This tracks how much drug is in your system over a full 12-hour period. It’s more precise. It tells you if you’re getting enough, too much, or just right. It’s not perfect, but it’s better. And it’s becoming the new standard.
For mycophenolate, AUC monitoring helps avoid under-dosing (which leads to rejection) or over-dosing (which causes low blood counts). For tacrolimus, it helps prevent kidney damage. Some hospitals now do this routinely. Others still use troughs because it’s cheaper and faster. But if your center offers AUC, ask for it. It could save your kidney.
What’s Next? The Future of Transplant Immunosuppression
The triple therapy isn’t going away anytime soon. But it’s changing.
Doctors are now using genetic testing to predict how you’ll metabolize tacrolimus. Some people break it down fast. Others hold onto it too long. That’s why two people on the same dose can have wildly different blood levels. Genetic markers help tailor your dose from day one.
There’s also biomarker research. Scientists are looking for proteins or genes in your blood that signal rejection before it happens. Imagine a simple blood test that says, “Your body is starting to react-let’s tweak your meds.” That’s not science fiction. It’s happening in trials right now.
And the push for steroid-free regimens is growing. With better induction drugs and tighter monitoring, more people are being taken off steroids safely. That means fewer weight gains, fewer broken bones, fewer mood crashes.
By 2030, experts predict up to 20% fewer people will be on the classic triple combo. Not because it doesn’t work-but because we now have smarter, kinder ways to do it.
What You Need to Do Every Day
Surviving a transplant isn’t just about medicine. It’s about routine.
- Take your pills at the same time every day. No skipping. No doubling up.
- Keep a log: what you took, when, and how you felt. Write down diarrhea, dizziness, rashes, or weird dreams.
- Don’t take OTC meds without asking your team. Ibuprofen? Bad. St. John’s Wort? Dangerous. Even antacids can mess with mycophenolate absorption.
- Wash your hands. Avoid sick people. Get your flu shot. Skip the reptile petting zoo.
- Go to every appointment-even if you feel fine. Your kidney can be failing and you won’t know.
It’s exhausting. It’s scary. It’s life-changing. But for tens of thousands of people, this regimen means a second chance. Not perfect. Not easy. But real.
Can I stop taking my immunosuppressants if I feel fine?
No. Stopping these drugs-even for a day-can trigger acute rejection within hours. Many people who stop because they feel fine end up losing their transplant. Immunosuppressants don’t make you feel better-they prevent your immune system from destroying your new kidney. If you’re struggling with side effects, talk to your transplant team. They can adjust your dose or switch medications. Never stop on your own.
Why do I need blood tests so often?
Tacrolimus has a very narrow window between too little and too much. Too little, and your body attacks the kidney. Too much, and it damages your kidneys, nerves, or liver. Blood tests show if your levels are in the safe zone. Mycophenolate levels also matter-low levels increase rejection risk. These aren’t routine checks-they’re life-saving checks.
Is there a chance I’ll still reject the kidney even on this regimen?
Yes. While the triple therapy cuts acute rejection down to about 8%, it doesn’t eliminate it. About 1 in 12 people still experience rejection in the first year. Chronic rejection-slower, silent damage-can happen even years later. That’s why lifelong monitoring is essential. The goal isn’t zero risk. It’s managing risk so your kidney lasts as long as possible.
Can I drink alcohol while on these drugs?
Moderate alcohol is usually okay-like one drink a day-but it’s risky. Alcohol can raise your blood pressure, hurt your liver, and interact with tacrolimus. It can also make you forget to take your pills. Many transplant centers recommend avoiding alcohol entirely, especially in the first year. If you want to drink, talk to your doctor first.
Will I have to take these drugs forever?
For most people, yes. There’s no cure for transplant rejection-only prevention. You’ll likely take at least tacrolimus and mycophenolate for life. Steroids may be stopped, but the other two usually stay. Some patients in rare cases can be weaned off completely under strict supervision, but that’s experimental. Think of these drugs as your new normal-like insulin for diabetes. They’re not a punishment. They’re your lifeline.




Virginia Seitz
December 16, 2025 AT 11:46Just took my meds. Still alive. 😊
Josh Potter
December 16, 2025 AT 15:03Bro. I took my tacrolimus at 7 a.m. and by 11 a.m. I was sweating like I ran a marathon. My doc says it's normal but I still think my body hates me. 🥲
Peter Ronai
December 18, 2025 AT 11:05Oh please. You’re all still using the 1998 protocol? I’ve been on belatacept since 2021. No steroids, no mycophenolate, no daily blood draws. Just one IV every four weeks. Your ‘gold standard’ is a relic. You’re all just scared of change.
Steven Lavoie
December 19, 2025 AT 22:28While Dr. Ronai’s point about belatacept is valid, it’s important to recognize that not all patients are candidates. Belatacept requires HLA-matched donors and carries a higher risk of PTLD in EBV-negative recipients. The triple therapy remains the safest default for the majority, especially in high-risk populations. Precision medicine is the future, but we’re not there yet.
CAROL MUTISO
December 21, 2025 AT 05:04It’s wild how we treat immunosuppression like a lock-and-key system - one drug for one cell, one pill for one problem. But the immune system doesn’t work like a machine. It’s a living, breathing, angry orchestra. Tacrolimus silences the violins. Mycophenolate burns the sheet music. Steroids? They just turn down the whole damn concert hall. And yet, we still act surprised when the bass drum starts playing again. We’re not fixing biology. We’re just drowning it in noise.
Jane Wei
December 21, 2025 AT 20:14I stopped steroids after 6 months. No moon face. No crying over commercials. Best decision ever.
Chris Van Horn
December 23, 2025 AT 14:19It is, of course, axiomatic that the pharmacokinetic variability of tacrolimus renders trough-level monitoring inherently flawed - a crude proxy for true exposure. One must employ AUC monitoring, preferably via LC-MS/MS, to achieve therapeutic precision. The fact that 78% of U.S. centers still rely on troughs is not merely suboptimal - it is a systemic failure of clinical governance.
Anna Giakoumakatou
December 25, 2025 AT 02:13Oh, so now we’re romanticizing the ‘whisper’ of chronic rejection? How poetic. I suppose the next article will be titled: ‘The Silent Sigh of My Kidney as It Fades Into the Mist.’
Sachin Bhorde
December 26, 2025 AT 00:21Bro, my tac level was 12.5 and my creatinine jumped to 2.1. Doc dropped me to 3mg BID. Now I’m at 1.1. But my stomach still hates me. Mycophenolate is the devil in a blue pill. I switched to enteric-coated - barely helped. Now I take it with yogurt. Works better than the science.
Nishant Desae
December 27, 2025 AT 12:44As someone who received a kidney from my brother in India, I want to say thank you for writing this. In our village, people think transplants are for rich people in America. But I want them to know - yes, it’s hard. Yes, you take pills every day. But I can play with my kids now. I can walk to the market. I am alive. And I still take my meds, even on days when I feel fine. Because I know what silence feels like - and I don’t want to go back.
Linda Caldwell
December 28, 2025 AT 10:01You got this. Every pill you take is a middle finger to death. Keep going.
Jigar shah
December 28, 2025 AT 10:21Interesting. In India, we often use lower doses of mycophenolate due to higher rates of leukopenia in our population. Also, many patients use herbal supplements like turmeric - which may interfere with tacrolimus. We need more studies on gene-drug interactions in non-Caucasian populations.
Kent Peterson
December 29, 2025 AT 21:20So… we’re giving people cancer drugs to keep a kidney alive? And you call this medicine? This isn’t treatment - it’s chemical hostage negotiation. I’d rather die than live like this.
Michael Whitaker
December 31, 2025 AT 10:10As a former transplant patient who now works in bioethics, I must say: the emotional burden of lifelong immunosuppression is rarely addressed in medical literature. The guilt of being ‘the one who survived.’ The fear of becoming a burden. The quiet grief over the body you lost - even when you gained a new one. This isn’t just pharmacology. It’s existential labor.