When someone overdoses on benzodiazepines, the biggest danger isn’t the drug itself-it’s what happens when breathing slows or stops. Benzodiazepines like alprazolam, diazepam, and lorazepam are commonly prescribed for anxiety, insomnia, and seizures. But when taken in large amounts-or mixed with alcohol, opioids, or other sedatives-they can shut down the central nervous system. The result? Slowed or stopped breathing, coma, and sometimes death. The good news? Most isolated benzodiazepine overdoses aren’t fatal. The bad news? They’re far more deadly when combined with other depressants. In fact, 92% of benzodiazepine-related deaths involve opioids or alcohol, according to CDC data from 2022.
What Happens During a Benzodiazepine Overdose?
Benzodiazepines work by boosting the effect of GABA, a calming neurotransmitter in the brain. Too much of it, and the brain can’t keep the body awake or breathing. Symptoms range from drowsiness and slurred speech to deep coma and respiratory arrest. A person may appear drunk but won’t respond to stimuli. Their breathing may be shallow, less than 10 breaths per minute. Pupils may be pinpoint, but unlike opioid overdoses, their skin usually stays warm and pink.
One key fact: benzodiazepine overdose alone rarely kills. Studies show the fatality rate for pure overdoses is just 0.01% to 0.05%. But when opioids are involved, the risk of death jumps 15 times higher. That’s why every overdose case must be treated as potentially mixed until proven otherwise.
Immediate Emergency Response: ABCDE Protocol
Emergency teams follow the ABCDE approach-Airway, Breathing, Circulation, Disability, Exposure. This isn’t optional. It’s the standard across the UK, Europe, and increasingly in U.S. emergency rooms.
- Airway: Check if the person can protect their airway. If they’re unresponsive or vomiting, position them on their side. Prepare for intubation immediately if they’re not breathing adequately.
- Breathing: Give oxygen via non-rebreather mask at 15 liters per minute. For patients with COPD or known CO2 retention, switch to a Venturi mask to avoid suppressing their drive to breathe.
- Circulation: Monitor heart rate and blood pressure continuously. Hypotension is rare in pure overdoses but common when opioids or alcohol are mixed in.
- Disability: Use the Glasgow Coma Scale. A score of 8 or below means urgent anesthesiology help is needed.
- Exposure: Remove clothing to check for injection marks, pill bottles, or medical alert tags. Look for signs of other drug use.
Don’t waste time guessing. Assume the worst: this could be a mixed overdose. Always check for opioids-even if the person only took a benzodiazepine, they might have unknowingly ingested fentanyl-laced pills.
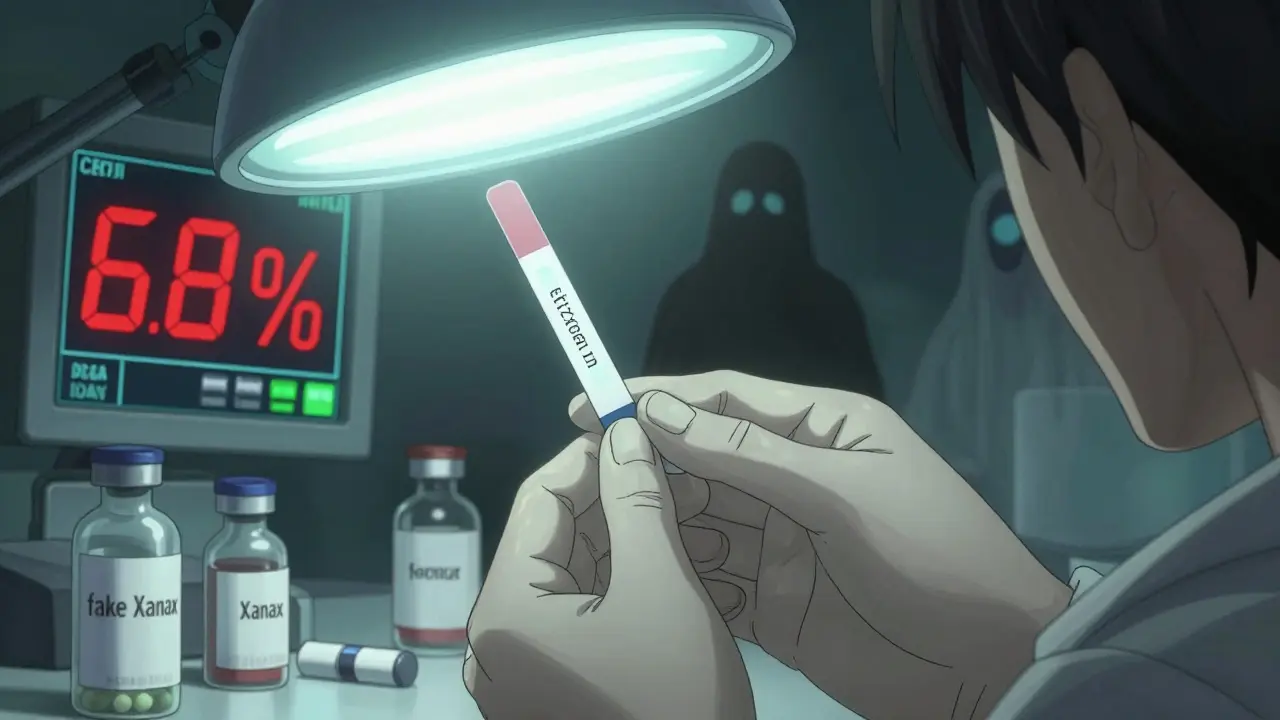
Testing and Diagnosis: What Doctors Look For
There’s no single test to confirm a benzodiazepine overdose. Diagnosis is clinical, based on symptoms and history. But labs help rule out other causes and uncover hidden dangers.
- Point-of-care glucose: Hypoglycemia can mimic overdose symptoms. Test immediately.
- Serum acetaminophen and aspirin: Many overdose patients take multiple drugs. These are common co-ingestants.
- Serum ethanol: Alcohol is involved in nearly half of all benzodiazepine overdose cases.
- Urine toxicology screen: Detects other sedatives, opioids, or new synthetic benzos like etizolam and clonazolam-now responsible for 68% of severe cases in the Western U.S.
Don’t rely on blood levels to guide treatment. Benzodiazepine concentrations don’t reliably predict severity. A person with a high level might be alert; someone with a low level might be comatose. Symptoms matter more than numbers.
Flumazenil: Why It’s Rarely Used
Flumazenil is the only drug that reverses benzodiazepines. It sounds perfect-until you know the risks.
Flumazenil works fast. But its effects last only 41 minutes. That means sedation often returns, requiring repeat doses every 20 minutes. Worse, it can trigger seizures in people who are dependent on benzodiazepines-up to 38% of cases, according to StatPearls. That’s why the American College of Medical Toxicology says flumazenil is appropriate in only 0.7% of overdose cases.
It’s especially dangerous in mixed overdoses. If someone takes alprazolam with trazodone or an antidepressant, flumazenil can cause violent seizures within seconds. Emergency nurses on Reddit report multiple cases where flumazenil caused harm-none where it saved a life without complications.
In 2023, 78% of U.S. emergency departments stopped stocking flumazenil. The European Resuscitation Council and American Heart Association no longer recommend it. The only time it’s considered: a known pure benzodiazepine overdose in a non-dependent patient with life-threatening respiratory depression that doesn’t improve with oxygen and ventilation.
Bottom line: Supportive care saves lives. Flumazenil rarely does.
When to Use Activated Charcoal
Activated charcoal can bind drugs in the stomach and prevent absorption. But it only works if given within 60 minutes of ingestion. After that, benzodiazepines are already absorbed-fast. Emergency Care BC found it reduces absorption by only 45% if given early. Beyond that, it’s useless.
And it’s not without risk. It can cause vomiting and aspiration, especially in unconscious patients. For that reason, most guidelines now say: don’t give it unless the patient is awake, alert, and swallowed the drug less than an hour ago.
Hemodialysis, whole bowel irrigation, and multiple doses of charcoal? None of these help. They’re outdated practices. The 2023 StatPearls review explicitly states they have no role in benzodiazepine toxicity.
Monitoring: How Long to Watch
Observation time depends on symptoms. Asymptomatic patients-those who took a pill but show no drowsiness-need at least 6 hours of monitoring. Most will be fine by then.
Symptomatic patients? Watch until every sign of sedation is gone. That usually takes 12 hours. But in older adults, people with liver disease, or those who took long-acting benzos like diazepam, it can take 24 to 48 hours. Alprazolam is especially tricky-it’s 3.2 times more likely to cause deep sedation requiring intubation than other benzos.
Use standardized tools to track progress: the Pasero Sedation Scale or Glasgow Coma Scale. Reassess every 15 minutes after any intervention. Document respiratory rate, oxygen saturation, and level of consciousness. Don’t discharge someone just because they’re awake. Ataxia (loss of coordination) lingers longer than drowsiness. A patient who can sit up might still be too unsteady to walk without falling.
The Changing Landscape: Illicit Benzos and New Risks
Benzodiazepine prescriptions have dropped 14.3% since 2019, thanks to tighter prescribing rules. But overdose cases have risen 27%-because people are now taking fake pills sold online. These aren’t prescription drugs. They’re illicitly made versions like etizolam, clonazolam, and bromazolam. They’re 3 to 10 times stronger than traditional benzos and often mixed with fentanyl.
California’s poison control system found that 68% of severe benzodiazepine overdoses now involve these synthetic versions. They’re harder to detect on standard urine tests. Hospitals are scrambling to adapt.
Meanwhile, harm reduction programs are expanding. As of January 2023, 37 U.S. states include benzodiazepine recognition in naloxone distribution programs. First responders now carry naloxone and are trained to watch for sedation even after reversing an opioid overdose. Why? Because naloxone won’t fix benzodiazepine-induced coma. That patient still needs airway support and hours of monitoring.

What’s Next? Research and Technology
New tools are emerging. In January 2023, the FDA approved the first continuous benzodiazepine blood monitor-BenzAlert™-for clinical trials. Early results show 94.7% accuracy in predicting when sedation will wear off. That could one day replace guesswork with real-time data.
The NIH is funding $4.2 million to develop longer-acting reversal agents. Flumazenil’s short half-life is a major limitation. A drug that lasts 8 hours instead of 40 minutes would be a game-changer.
Point-of-care ultrasound (POCUS) is also gaining ground. Emergency teams are using it to quickly assess lung movement and breathing effort. Studies show it cuts intubation delays by 22 minutes on average.
By 2025, the American College of Medical Toxicology predicts a 40% increase in emergency visits for benzodiazepine overdoses. The rise of synthetic benzos won’t slow down. The medical community must adapt-not by chasing reversal drugs, but by mastering supportive care.
Key Takeaways for Emergency Response
- Most benzodiazepine overdoses aren’t fatal-but they become deadly when mixed with opioids or alcohol.
- Always assume a mixed overdose until proven otherwise. Test for opioids, alcohol, and other drugs.
- Supportive care-airway, oxygen, ventilation-is the gold standard. Never delay intubation for a patient who can’t breathe.
- Flumazenil is rarely needed and often dangerous. Avoid it in patients with known dependence or possible co-ingestants.
- Activated charcoal only helps if given within an hour. After that, it’s pointless and risky.
- Monitor for at least 12 hours in symptomatic patients. Discharge only when full alertness and coordination return.
- Illicit synthetic benzodiazepines are the new threat. They’re stronger, harder to detect, and often laced with fentanyl.
Can you die from a benzodiazepine overdose alone?
Yes, but it’s extremely rare. Isolated benzodiazepine overdoses have a fatality rate of only 0.01% to 0.05%. Death usually occurs only if breathing stops completely and isn’t supported. Most deaths happen when benzodiazepines are mixed with opioids, alcohol, or other sedatives.
Is flumazenil safe to use in all benzodiazepine overdoses?
No. Flumazenil is dangerous in patients with chronic benzodiazepine use or those who may have taken other drugs like antidepressants or opioids. It can trigger seizures, arrhythmias, or sudden withdrawal. It’s only considered in rare cases: pure overdose, no dependence, and severe respiratory failure that doesn’t respond to oxygen or ventilation.
How long should someone be monitored after a benzodiazepine overdose?
Asymptomatic patients need at least 6 hours. Symptomatic patients require monitoring until all signs of sedation and ataxia are gone-usually 12 hours, but up to 24-48 hours in elderly patients or those taking long-acting benzos like diazepam. Never discharge someone just because they’re awake; coordination takes longer to recover.
Do activated charcoal or dialysis help treat benzodiazepine overdose?
No. Activated charcoal only works if given within 60 minutes of ingestion, and even then, its benefit is limited. Hemodialysis and whole bowel irrigation have no proven role. Benzodiazepines are rapidly absorbed and not removed by dialysis. Current guidelines strongly advise against these treatments.
Why are synthetic benzodiazepines like etizolam more dangerous?
Synthetic benzos like etizolam and clonazolam are 3 to 10 times more potent than traditional ones like diazepam. They’re often sold as fake prescription pills and mixed with fentanyl. They’re harder to detect on standard drug screens, delay diagnosis, and cause deeper, longer-lasting sedation. They now account for nearly 70% of severe overdose cases in the Western U.S.
What to Do Next
If you suspect someone has overdosed on benzodiazepines, call 911 immediately. Don’t wait for symptoms to worsen. Don’t try to wake them with cold showers or coffee. Don’t give them flumazenil or charcoal unless you’re a trained provider. Your job is to keep them breathing and safe until help arrives.
For medical professionals: review your facility’s overdose protocol. Make sure everyone knows the ABCDE approach. Remove flumazenil from emergency carts unless you have a specific, approved use case. Train staff to recognize synthetic benzos. And never assume an overdose is isolated-always test for opioids.
The future of overdose care isn’t in new drugs. It’s in better monitoring, faster recognition, and smarter protocols. Supportive care saves lives. And in the case of benzodiazepine overdose, it always has-and always will.






Poppy Newman
January 7, 2026 AT 07:52Anastasia Novak
January 8, 2026 AT 05:07Jonathan Larson
January 9, 2026 AT 10:40Alex Danner
January 9, 2026 AT 22:04Elen Pihlap
January 11, 2026 AT 03:58LALITA KUDIYA
January 12, 2026 AT 13:07Mina Murray
January 14, 2026 AT 03:23Rachel Steward
January 15, 2026 AT 23:05Katrina Morris
January 15, 2026 AT 23:40Anthony Capunong
January 17, 2026 AT 03:21Aparna karwande
January 19, 2026 AT 01:10Jessie Ann Lambrecht
January 20, 2026 AT 16:05Ayodeji Williams
January 21, 2026 AT 10:57