When the pandemic hit, most people worried about masks, ventilators, and hospital beds. But behind the scenes, something quieter and just as dangerous was unfolding: drug shortages. Essential medications-from antibiotics to insulin to blood pressure pills-suddenly vanished from pharmacy shelves. At the same time, the illegal drug supply turned deadly as fentanyl flooded the streets. This wasn’t just a glitch. It was a systemic collapse that exposed how fragile our medicine supply really is.
Medicines Gone Missing
From February to April 2020, nearly one in three drug supply reports turned into actual shortages. That’s a fivefold jump from pre-pandemic levels. Drugs needed for ICU patients-sedatives, muscle relaxants, even basic antibiotics-were running out. Hospitals scrambled. Nurses rationed doses. Patients delayed treatments because their prescriptions couldn’t be filled. The problem wasn’t one factory shutting down. It was the whole chain. Most active ingredients in pills come from China and India. When lockdowns hit there, production slowed. Shipping containers piled up at ports. Workers got sick. Even a small delay upstream meant a medicine vanished on your local pharmacy shelf weeks later. By May 2020, things started to stabilize. The FDA stepped in-pushing manufacturers to report shortages earlier, fast-tracking inspections, and urging companies to build backup supplies. But the damage was done. By then, 14% of all supply issues had already led to shortages within six months. And 6% of those were severe-meaning the drug was at least one-third harder to find than before.The Illicit Market Turns Deadly
While hospitals fought for morphine, people using street drugs faced a different crisis. With borders closed and traditional suppliers cut off, drug cartels didn’t stop selling-they just made their products more potent and cheaper. Fentanyl, a synthetic opioid 50 to 100 times stronger than morphine, became the go-to filler. It’s easy to smuggle, cheap to make, and a little goes a long way. People who used heroin or painkillers before the pandemic didn’t know what they were getting anymore. Reddit threads from June 2020 tell the same story: “Dose that used to be fine knocked me out cold.” “My friend didn’t wake up.” “I thought I was buying oxy, but it was all fentanyl.” The numbers don’t lie. From May 2019 to April 2020, there were 77,007 drug overdose deaths in the U.S. From May 2020 to April 2021? Nearly 98,000. That’s a 31% jump in just one year. Some states saw increases over 50%. West Virginia, Kentucky, Louisiana-places already hit hard by addiction-got worse.
Telehealth Helped Some, Left Others Behind
As in-person clinics closed, the government moved fast to expand telehealth for addiction treatment. For the first time, doctors could prescribe buprenorphine-medication that helps manage opioid addiction-over video calls. By April 2020, 95% of those prescriptions were done remotely. That saved lives for people who lived far from clinics or couldn’t leave home. But not everyone could benefit. Older adults didn’t know how to use Zoom. People in rural areas had no reliable internet. Some couldn’t afford smartphones. Meanwhile, in-person support groups-NA meetings, peer counseling, needle exchanges-shut down or cut hours. One program in Philadelphia saw its services drop by 40%. Harm reduction workers handed out naloxone kits by drive-through, but they couldn’t replace the human connection that kept people from relapsing. A study found that people with private insurance cut their behavioral health visits by 75% in the spring of 2020. That’s not because they didn’t need help. It’s because the system failed to meet them where they were.Who Got Left Out?
The pandemic didn’t create new inequalities-it amplified them. People without insurance, people of color, those living in poverty, and people with mental health conditions were hit hardest. If you were already struggling to get your meds, lockdowns made it worse. If you were afraid to go to the ER because of stigma, you stayed home until it was too late. A person with diabetes rationing insulin because they couldn’t refill their prescription. A veteran skipping his antidepressant because his VA clinic closed. A mother hiding her fentanyl use because she feared losing custody of her kids. These weren’t rare cases. They were the new normal. The data shows this clearly: overdose deaths rose fastest in communities that already had the fewest resources. And while telehealth helped some, it left others in the dark-literally.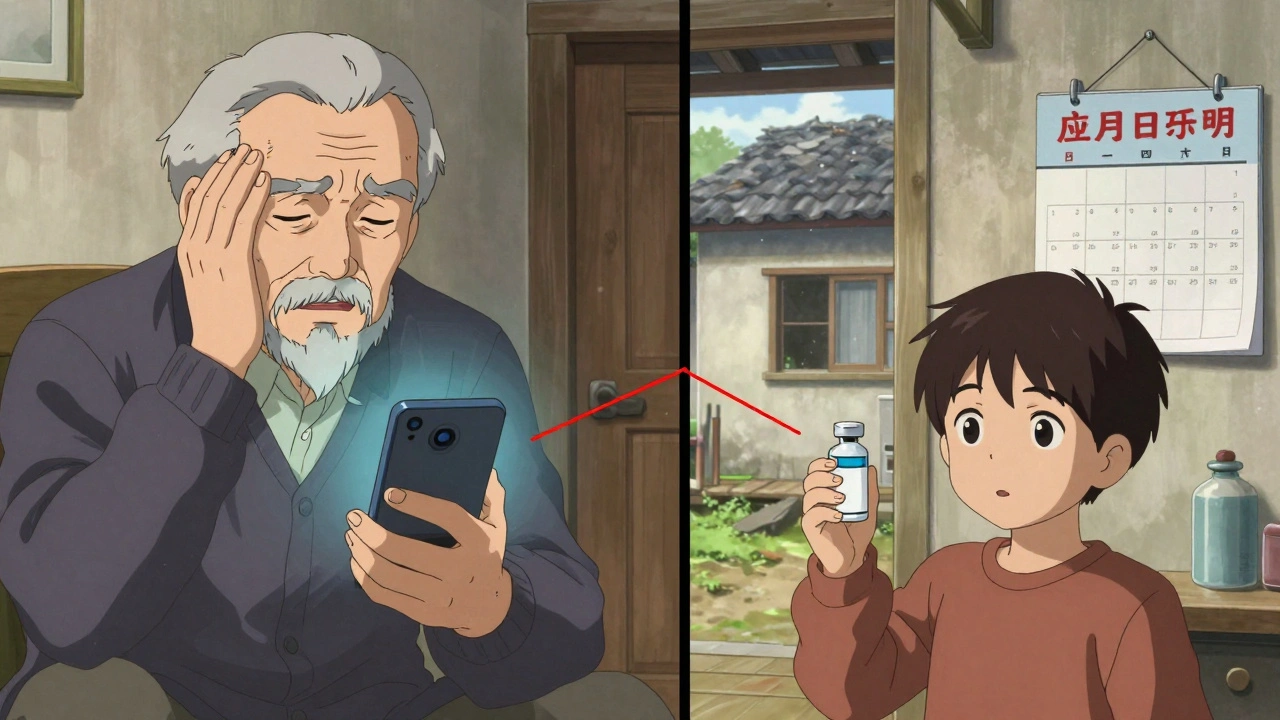







Gareth Storer
December 5, 2025 AT 00:04Oh wow, so the system collapsed because... people needed pills? Shocking. Next you’ll tell me breathing is important too. 🤡
Pavan Kankala
December 6, 2025 AT 00:23This is all a psyop. The FDA and Big Pharma teamed up with China to create artificial shortages so they could push you into telehealth and biometric tracking. Fentanyl? That’s not a drug-it’s a tracker. They’re using overdoses to justify the surveillance state. You think insulin is hard to get? Wait till they start charging you per milligram via your smart fridge.
Martyn Stuart
December 6, 2025 AT 23:46Let’s be clear: the supply chain fragility exposed here isn’t new-it’s been warned about since the 2000s. We outsourced manufacturing for cost savings, ignored redundancy, and treated medicine like a commodity, not a human right. The pandemic didn’t break the system; it just held up a mirror. We need domestic production of critical APIs, strategic stockpiles, and mandatory transparency from manufacturers. And yes-this requires investment. But what’s the cost of another 100,000 deaths? Nothing, apparently.
Jessica Baydowicz
December 7, 2025 AT 03:14Y’all. I just want to say-this hit me in the soul. My cousin went without her blood pressure meds for 3 weeks in 2020. She ended up in the ER, scared, confused, and crying because she thought she was dying. She’s fine now, but the fear? That stuck. We need to treat meds like oxygen. Not a luxury. Not a privilege. Just… basic. 💙
Yasmine Hajar
December 8, 2025 AT 23:02As a Black woman in rural Georgia, I saw this up close. My dad’s diabetes meds? Gone for months. The VA clinic? Closed. The nearest pharmacy? 45 minutes away, and they wouldn’t refill without an in-person visit. Meanwhile, the corner store had fentanyl-laced pills for $5. No one talked about it. Everyone just… stopped asking. We didn’t need data. We needed help. And no one came.
Karl Barrett
December 10, 2025 AT 14:14The ontological rupture of pharmaceutical access during the pandemic reveals a deeper epistemological failure: the conflation of logistical efficiency with systemic resilience. We optimized for lean supply chains, but neglected the latent variables of human vulnerability. The result? A bifurcated healthcare reality: those with capital and connectivity survived via telehealth; those without were rendered statistically invisible. The tragedy isn’t the shortage-it’s the normalization of it.
Libby Rees
December 12, 2025 AT 03:29People died because we didn’t plan for this. That’s it.
Gillian Watson
December 13, 2025 AT 10:40My mom’s insulin was out for six weeks. She cut her dose in half. She didn’t tell anyone. She just kept going. We’re lucky she’s still here. But so many weren’t. This isn’t politics. It’s just… wrong.
Jordan Wall
December 14, 2025 AT 02:53Bro… the fact that we’re even talking about this like it’s news? 😒 Like, we all knew the supply chain was a house of cards. And now we’re surprised? Also, fentanyl? That’s just capitalism’s way of saying ‘you’re not worth the full dose.’ 🤷♂️💊
George Graham
December 14, 2025 AT 10:50I’ve worked in harm reduction for 15 years. The telehealth push saved lives, but it also exposed how disconnected we are from real people. You can’t replace a handshake with a Zoom call. You can’t replace a warm blanket and a cup of tea with a prescription app. The people who fell through the cracks? They weren’t invisible. We just stopped looking.
John Filby
December 15, 2025 AT 00:42My cousin OD’d last year. He thought he was buying oxy. He wasn’t. I didn’t even know how to use naloxone until it was too late. Now I carry two. I teach my friends. If you’re reading this and you don’t know how to use it-go to your pharmacy. It’s free. Just… do it. Please.