Every year, thousands of people in the U.S. and UK receive the wrong medication-not because of a mistake in diagnosis, but because two drug names look or sound too similar. Look-alike and sound-alike (LASA) drug names are one of the most common causes of preventable medication errors. You might think it’s rare, but research shows that about 1 in every 1,000 prescriptions contains a name confusion error. And in 34% of those cases, the patient actually gets the wrong drug. Some of these errors lead to serious harm-or worse.
Take hydroCODONE and hydroALAzine. One is a painkiller. The other is for high blood pressure. If you mix them up, you could overdose on opioids or dangerously drop your blood pressure. These aren’t theoretical risks. They happen in hospitals, pharmacies, and even at home when prescriptions are printed poorly or handwritten. The good news? There are clear, proven ways to spot these dangerous pairs before they cause harm.
What Makes Drug Names Look or Sound Alike?
Not all similar drug names are equally risky. The real danger comes when two names share 60-80% of the same letters or syllables. That’s the sweet spot where your brain glides over the differences without noticing. For example:
- vinBLAStine vs. vinCRIStine (both cancer drugs)
- CISplatin vs. CARBOplatin (both chemotherapy agents)
- doXEPamine vs. doBUTamine (one treats depression, the other boosts heart function)
These aren’t typos. They’re brand names and generics that were approved before anyone fully understood how confusing they could be. The FDA has been tracking this since 2001 and now maintains a list of 35 high-risk pairs as of 2025. But even with that list, errors still happen-because visual cues aren’t always consistent.
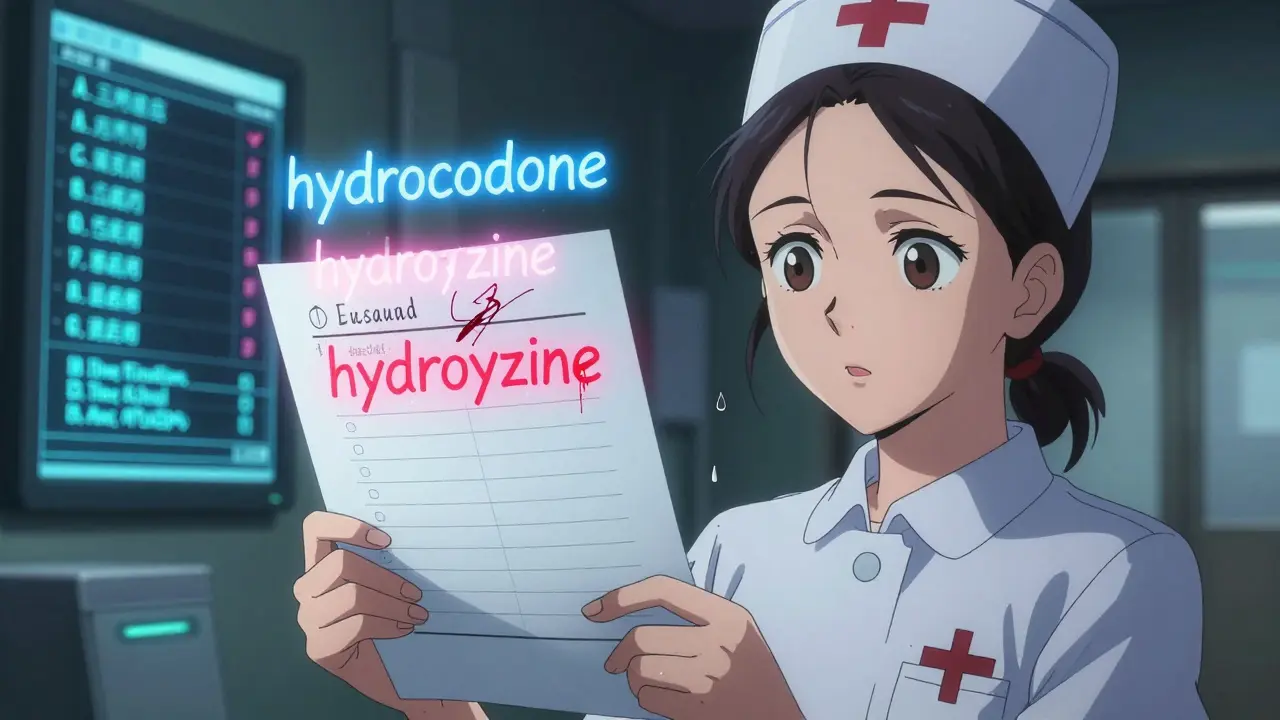
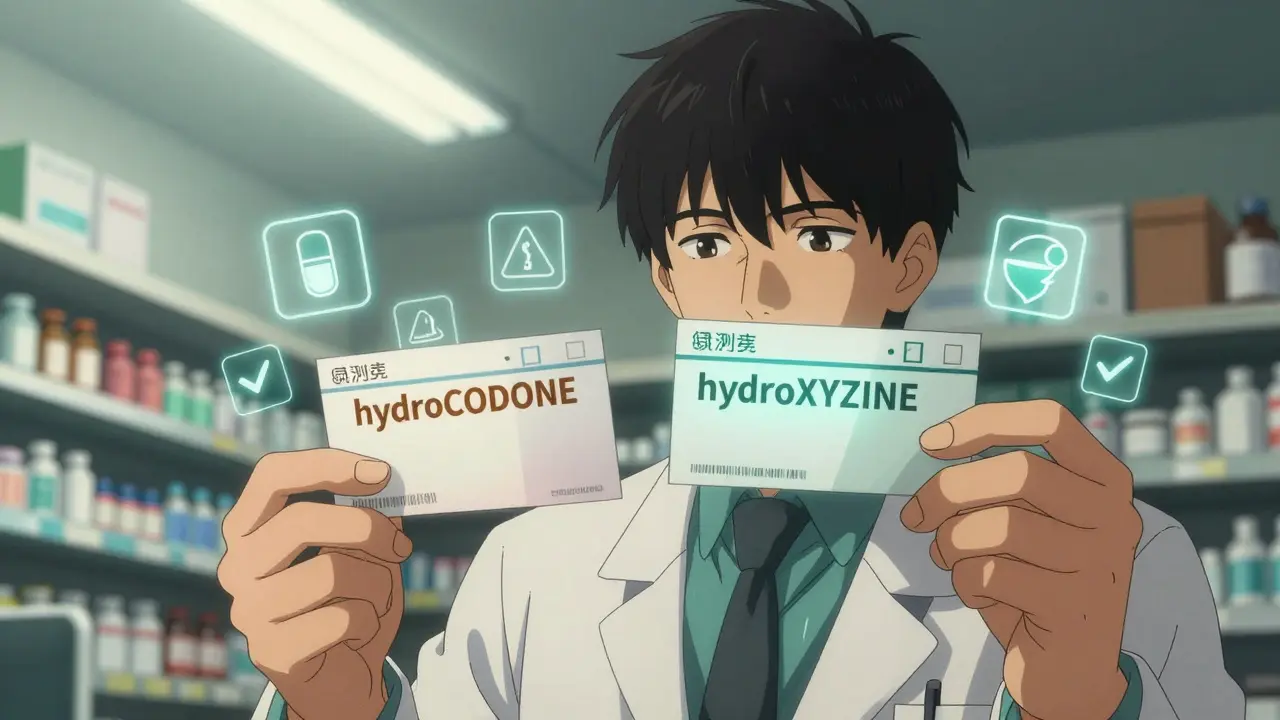
Tall Man Lettering: The Visual Shield Against Confusion
The most widely used tool to fight LASA errors is called tall man lettering. It’s simple: capitalize the parts of the drug name that differ. So instead of writing “hydrocodone” and “hydroxyzine,” you write hydroCODONE and hydroXYZINE. The uppercase letters act like visual signposts, forcing your eyes to slow down and notice the difference.
The FDA recommends capitalizing 2-4 letters that create the clearest visual contrast. This isn’t just a suggestion-it’s now standard in electronic health records, pharmacy labels, and automated dispensing machines. Studies show that when tall man lettering is used correctly, it reduces visual confusion by up to 32%. But here’s the catch: it only works if it’s applied everywhere.
Many healthcare workers report frustration when one system uses tall man lettering and another doesn’t. One nurse in Bristol described switching between her hospital’s EHR (which shows hydrOXYzine) and the printed label from the pharmacy (which says hydroxyzine). “I start doubting myself,” she said. “Did I read it wrong? Or did they forget the caps?” That uncertainty is exactly what leads to mistakes.
More Than Just Letters: Color, Context, and Confirmation
Tall man lettering alone isn’t enough. The best protection comes from combining multiple layers:
- Color coding: Some hospitals use background colors to distinguish high-risk pairs. For example, insulin vials might be labeled with a yellow background to set them apart from other injectables. Research shows combining color with tall man lettering boosts error reduction to 47%.
- Purpose-of-treatment: Adding a short note like “for anxiety” or “for arrhythmia” right next to the drug name helps staff double-check intent. At Johns Hopkins Hospital, this simple addition cut LASA errors by 59% when paired with tall man lettering.
- Brand + generic names: Seeing both names together helps. For instance, “Valtrex (valACIClovir)” vs. “Valcyte (valGANCIClovir)” makes the difference obvious-even if you’re rushing.
These aren’t fancy tech tricks. They’re basic human-centered design. Your brain works better when it has multiple cues to rely on. Don’t trust just one.
How to Spot a Look-Alike Name-A 3-Step Check
If you’re a pharmacist, nurse, or even a caregiver picking up a prescription, use this simple routine every time you handle a high-risk drug:
- Read the full label-not just the first few letters. Look for capitalized differences. If you see “hydroCODONE,” pause. Is this the one for pain? Or is it hydroXYZINE for allergies?
- Confirm with a second person-even if you’re sure. Studies show that a second pair of eyes catches 78% of errors missed by the first person. Say out loud: “This is hydroCODONE for pain, not hydroXYZINE for itching.”
- Read it again before giving it to the patient. That final check reduces errors by 52%. It’s not about distrust-it’s about building a safety net.
This isn’t extra work. It’s a habit that saves lives. And it takes less than 15 seconds per prescription.
Why Handwritten Prescriptions Are Still a Big Risk
Even with all the digital tools, handwritten prescriptions are still common-especially in urgent care clinics, nursing homes, and rural areas. And they’re the #1 source of LASA errors outside hospitals.
A 2023 survey found that 41% of LASA errors occurred because a doctor scribbled “hydroxyzine” without tall man lettering, and the pharmacist misread it as “hydrocodone.” Poor ink, shaky handwriting, and rushed notes make it easy to confuse “D” and “O,” “B” and “H,” or “C” and “O.”
Electronic prescribing systems have cut these errors by 68%, but they’re not everywhere. If you’re the one writing or receiving a paper script, slow down. Ask the prescriber to spell the name out loud. Write it down yourself before filling it. Don’t assume.
The Tech That’s Making a Difference
Technology is helping-but only if used right.
- Barcode scanning at every step-stocking, dispensing, administering-cuts errors by up to 89%. It’s the gold standard, but it costs hospitals over $150,000 to implement.
- Computer alerts in EHR systems pop up when you select a high-risk pair. But here’s the problem: clinicians override 49% of them because they’re too frequent. Smart systems now only trigger alerts for the 35 FDA-listed high-risk pairs, cutting alert fatigue by more than half.
- AI tools like Google Health’s Med-PaLM 2 can now predict which new drug names might cause confusion before they’re even approved. Since 2018, 17 potentially dangerous names have been blocked from entering the market thanks to this system.
But tech doesn’t replace human vigilance. It just supports it.
What You Can Do Right Now
You don’t need to wait for your hospital to upgrade its systems. Here’s what you can do today:
- Learn the top 10 LASA pairs-like hydroCODONE/hydroXYZINE, doXEPamine/doBUTamine, and CISplatin/CARBOplatin. Keep a printed list in your pocket or on your phone.
- Always check the full name-even if you’ve seen it a hundred times.
- Ask for clarification-if a name looks suspicious, say so. No one will think you’re being slow. They’ll think you’re careful.
- Report near-misses-if you almost gave the wrong drug, report it. These reports help update safety lists and prevent future errors.
Medication safety isn’t about perfection. It’s about layers. One layer might fail. But if you’ve got tall man lettering, double-checking, and clear labeling? The chances of harm drop dramatically.
What’s Coming Next
The FDA plans to expand its list of recommended tall man lettering pairs to 50 by 2026. New standards require all pharmacy labels, EHRs, and automated dispensers to use consistent formatting. AI-powered tools will soon flag confusing names in real time during e-prescribing. And smartphone apps are being tested that can scan a vial and instantly tell you if it’s a look-alike to another drug in the patient’s list.
But none of this matters if we don’t stay alert. The safest system in the world won’t help if someone skips the last check.
Every time you pause before handing over a prescription, you’re not just following protocol. You’re protecting someone’s life.
What are look-alike and sound-alike (LASA) drug names?
Look-alike and sound-alike (LASA) drug names are medications with similar spelling or pronunciation that can easily be confused, leading to dangerous medication errors. Examples include hydroCODONE and hydroXYZINE, or vinBLAStine and vinCRIStine. These aren’t typos-they’re approved drug names that pose a high risk because their similarities trick the brain into mistaking one for the other.
How does tall man lettering help prevent medication errors?
Tall man lettering uses uppercase letters to highlight the parts of drug names that differ, making it easier to spot similarities. For example, writing hydroCODONE instead of hydrocodone draws attention to the “CODONE” part, helping staff quickly distinguish it from hydroXYZINE. Studies show this method reduces visual confusion errors by up to 32% when used consistently across all systems.
Why are handwritten prescriptions still a problem for LASA errors?
Handwritten prescriptions often lack tall man lettering, have poor legibility, or are written quickly under pressure. A doctor’s scribble of “hydroxyzine” can easily be misread as “hydrocodone,” especially if the pharmacist is rushed. Nearly 41% of LASA errors occur because of handwritten orders, making them the leading cause outside of digital systems.
Can technology completely eliminate LASA errors?
No. While barcode scanning prevents up to 89% of errors and AI tools can predict confusing names with 89% accuracy, technology can’t replace human attention. Clinicians still override alerts, systems can have inconsistent formatting, and handwritten orders slip through. The most effective approach combines technology with verified human checks at every step.
What should I do if I suspect a prescription has a look-alike name?
Stop. Don’t fill or administer it. Double-check the full name using tall man lettering. Confirm the purpose of the medication-ask the prescriber or check the patient’s chart. If you’re still unsure, consult a pharmacist or supervisor. Never assume. Reporting near-misses helps improve safety systems for everyone.






Alisa Silvia Bila
December 20, 2025 AT 06:08Just read this at my mom’s pharmacy shift last night. We had a near-miss with hydROXYzine and hydROCODONE. I paused, read it twice, and called the doctor. She said I was being paranoid. Turns out, the script was handwritten and totally wrong. I’m not sorry I checked.
Marsha Jentzsch
December 20, 2025 AT 11:02THIS IS WHY WE NEED TO BAN HANDWRITTEN PRESCRIPTIONS!!!
It’s 2025!!! Why are we still letting doctors scribble like they’re in a 1950s Western?! I’ve seen people get the wrong drug because someone couldn’t tell a ‘D’ from an ‘O’!!!
And don’t even get me started on how pharmacies don’t even USE tall man lettering consistently!!!
It’s not just negligence-it’s a systemic failure!!!
Someone’s going to die because of this, and it’s going to be someone’s MOM!!!
Henry Marcus
December 20, 2025 AT 13:29Ever wonder why the FDA only lists 35 pairs? Because they’re being controlled by Big Pharma.
They don’t want you to know that 90% of similar drug names are intentionally designed to confuse you-so you keep buying the expensive brand versions.
HydroCODONE vs hydroXYZINE? Nah, they’re both made by the same parent company.
They profit from your confusion.
And now they’re pushing AI to ‘solve’ it? That’s just a distraction.
They’re not trying to fix the system-they’re trying to monetize the fear.
Check the patent filings. Everything’s connected.
Wake up.
They’re not protecting you. They’re protecting their margins.
Adrienne Dagg
December 21, 2025 AT 05:22Okay but like… I’m just a caregiver and I don’t have time to memorize 35 drug pairs 😭
Can we just make all the labels look like warning signs? 🚨
Also, why is this not on every pharmacy app? I need a ‘DANGER: LOOK-ALIKE’ button when I scan a script!
Also also-can we get a sound alert when someone says ‘hydro’? Like, ‘WARNING: HYDRO-WORD DETECTED’? 🤖🔊
Kinnaird Lynsey
December 21, 2025 AT 18:34I work in a rural clinic where we still use paper scripts. We started using color-coded sticky notes next to high-risk names-yellow for opioids, blue for BP meds. It’s dumb, but it works.
People laugh at first. Then they stop making mistakes.
Simple solutions > fancy tech when you’re understaffed and overworked.
Also, the ‘read it out loud’ rule? Non-negotiable.
Even if you’re alone. Even if you’re tired.
Just say it.
shivam seo
December 21, 2025 AT 23:20US healthcare is a joke. We’re spending millions on AI to fix problems that Australia solved with plain old standardization in 2010.
We don’t need more ‘layers’-we need one national standard.
Stop letting 50 different hospitals do whatever they want.
And stop pretending handwritten scripts are ‘common’-they’re just lazy.
Fix the system, not the symptoms.
benchidelle rivera
December 22, 2025 AT 01:15As a nurse with 22 years in oncology, I’ve seen vinBLAStine misread as vinCRIStine-and I’ve seen patients die because of it.
There is no excuse for not using tall man lettering. None.
If your EHR doesn’t auto-format it, demand it.
If your pharmacy prints it wrong, refuse the med.
And if your hospital says ‘we don’t have the budget’-tell them the cost of one death is $5 million in lawsuits and reputational damage.
This isn’t optional. It’s ethics.
Isabel Rábago
December 23, 2025 AT 09:02People act like this is new, but I’ve been warning about this since 2008.
Back then, I had a friend who got the wrong chemo drug because the nurse didn’t capitalize the ‘C’ in CARBOplatin.
She survived. But she lost a kidney.
And now we’re still talking about it like it’s a ‘new insight’?
It’s not a ‘system failure’-it’s a moral failure.
We knew. We knew. And we did nothing.
Until someone dies. Again.
Mike Rengifo
December 23, 2025 AT 15:54My cousin works at a pharmacy in Ohio. They just started using barcode scanners last year. They went from 3 errors a month to zero.
But the manager cut the scanner budget after 6 months because ‘it wasn’t cost-effective’.
They went back to manual checks.
Two weeks later, someone got the wrong insulin.
He’s fine. But the system didn’t learn.
People are too cheap to save lives.
That’s the real story here.
Ashley Bliss
December 25, 2025 AT 11:34I used to be a pharmacy tech. I thought I was good at my job.
Then I almost gave a patient hydroXYZINE instead of hydroCODONE because I was rushing.
I didn’t even notice the mistake until the patient said, ‘Wait, this isn’t what I usually take.’
That moment broke me.
I quit six months later.
Not because I was bad at the job.
But because the system doesn’t care if you’re good.
It only cares if you’re fast.
And that’s the real tragedy.
Not the drugs.
The culture.
Dev Sawner
December 27, 2025 AT 01:05It is imperative to underscore that the implementation of tall man lettering constitutes a non-negotiable standard of care within the pharmaceutical domain. The absence of standardized orthographic differentiation represents a systemic deficiency in patient safety protocols, which contravenes the fundamental tenets of clinical diligence. The statistical efficacy of this intervention, as cited by the FDA, is empirically validated and ought to be universally mandated without discretionary deviation. Furthermore, the persistence of handwritten prescriptions in the digital age constitutes a flagrant dereliction of professional responsibility, and remedial action must be instituted at the institutional level without further delay.
Elaine Douglass
December 27, 2025 AT 06:06i just read this and thought of my grandma who got the wrong pill last year
she’s fine now but i wish someone had told me about this sooner
thanks for writing this
everyone should read it
Alex Curran
December 28, 2025 AT 20:48Biggest gap I’ve seen? Nobody teaches this in med or pharmacy school.
We learn the drugs, the doses, the interactions-but no one says ‘hey, these two look like twins and one will kill you.’
It’s like teaching car mechanics but never showing people how to check the brakes.
We need a mandatory module on LASA pairs in every curriculum.
It’s not extra. It’s essential.
Kitt Eliz
December 30, 2025 AT 04:54LET’S GOOOOOOOO!!! 🚀
This is EXACTLY the kind of life-saving, human-centered design we need more of!!!
Tall man lettering + color coding + double-checks = UNSTOPPABLE SAFETY STACK!!!
And AI predicting dangerous names before approval? THAT’S THE FUTURE!!!
Stop waiting for the system to change-BE THE CHANGE!!!
Print this list. Stick it on your fridge. Teach your kids. Report every near-miss.
WE CAN DO THIS!!! 💪❤️