Why Patients Think Generic Medicines Don’t Work - Even When They Do
Imagine switching from your brand-name antidepressant to a generic version, only to wake up the next day feeling more anxious, dizzy, and tired than ever. You didn’t change your dose. You didn’t miss a pill. But something feels off. You start blaming the new pill - the one with the plain white label and unfamiliar name. It’s not just in your head. Research shows this happens more often than you think.
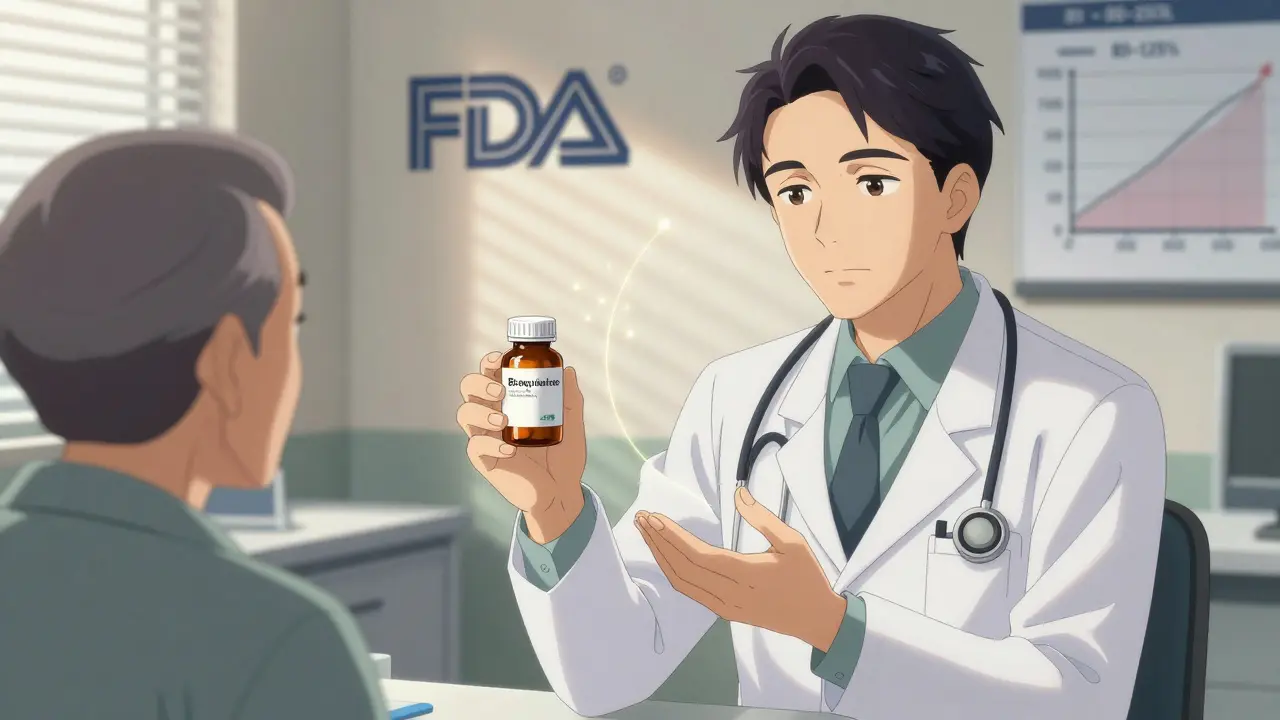
Here’s the truth: generic drugs are chemically identical to their brand-name counterparts. They contain the same active ingredient, in the same strength, and are absorbed into your body at the same rate. The generic medications you get at the pharmacy are required by the FDA to meet the same strict standards as the brand-name version. So why do so many people report worse side effects - or even feel like the medicine isn’t working anymore?
The Nocebo Effect: When Expectations Hurt More Than the Drug
The answer lies in something called the nocebo effect. Unlike the placebo effect - where positive expectations make a treatment feel more effective - the nocebo effect is when negative beliefs cause real, physical symptoms. It’s not a trick of the mind. It’s biology. Your brain expects harm, and your body responds as if it’s under threat.
A 2025 study tested this with fake nasal spray. Half the participants were told they were getting a brand-name product. The other half were told it was generic - same chemical formula, same delivery method, but different packaging and price cues. Those who believed they were taking the generic version reported significantly more side effects - even though the spray had no active ingredient at all. The difference? Their expectations. The same thing happens with real medications.
Studies show that about 1 in 5 people in placebo groups of clinical trials report side effects - nausea, headaches, fatigue - even when they’re not taking any medicine. And nearly 1 in 10 drop out of trials because they think the treatment is making them worse. That’s not a fluke. That’s the nocebo effect in action.
Price, Packaging, and Perception: How Your Brain Judges a Pill
Your brain doesn’t just look at the active ingredient. It looks at the label. The color. The shape. The price tag. A 2024 study tested this with a fake anti-itch cream. One group got a cream in a sleek blue box labeled "Solestan® Creme" - it looked expensive. The other group got the exact same cream in a plain orange box labeled "Imotadil-LeniPharma Creme" - it looked generic. The people who thought they were using the expensive version reported less pain sensitivity. The ones who thought they were using the generic version? They felt more pain. Even though the cream had no active ingredient.
This isn’t just about price. It’s about trust. When a pill looks cheap, feels unfamiliar, or comes from a company you’ve never heard of, your brain starts scanning for problems. You notice every little ache. Every mood swing. Every sleepless night. And you blame the new pill.
And it gets worse when the brand changes. In New Zealand, when doctors switched patients from one brand of venlafaxine to another, reports of side effects didn’t spike right away. But after local news ran stories about the switch - warning people that "the new version might not work the same" - reports of side effects jumped by over 200%. The medicine didn’t change. The fear did.
How Common Is This? The Numbers Don’t Lie
Eighty-nine percent of all prescriptions filled in the U.S. in 2022 were for generic drugs. That’s nearly 9 out of 10 pills. But a 2023 survey found that 38% of patients still believe generic medications are less effective than brand-name ones. That’s a huge gap between science and perception.
And it’s not just in the U.S. A meta-analysis of 37 studies found that 15 to 22% of the side effects reported after switching to a generic drug are likely caused by the nocebo effect - not the drug itself. That means thousands of people are suffering unnecessarily because they believe the generic won’t work.
Even more telling: authorized generics - the exact same pills made by the same company that makes the brand-name version, just sold under a different label - still trigger more side effect reports than the branded version. Same factory. Same ingredients. Same packaging design. Only the name changed. And still, patients reported worse outcomes.
What Doctors and Pharmacists Can Do - Real Strategies That Work
Changing how patients think about generics isn’t about lying. It’s about reframing. Here’s what actually helps:
- Don’t lead with the word "generic." Instead, say: "This is the same medication you were taking, just a different brand name. It’s been tested to work exactly the same way."
- Use positive framing. Instead of saying, "Some people get headaches," say: "Most people tolerate this well. If you notice anything unusual, let us know - we’ll help you adjust."
- Explain the savings. A 2022 study found that when patients were told switching to a generic could save them $3,172 a year - and that it was just as effective - nocebo effects dropped by 37%. Money talks, but so does trust.
- Use trusted visuals. Some pharmacies now use "branded generics" - packaging that looks closer to the original brand. It’s not misleading. It’s just reducing the psychological shock of change.
- Don’t overwhelm with side effect lists. Listing every possible side effect during a 5-minute visit triggers anxiety. Focus on what’s common, what’s serious, and what’s unlikely.
What Patients Can Do - Taking Back Control
If you’ve switched to a generic and started feeling worse, don’t assume it’s the drug. Ask yourself:
- Did anything else change? Stress levels? Sleep? Diet?
- Did I hear someone say the generic doesn’t work?
- Is the new pill a different color or shape? That might feel strange, but it doesn’t mean it’s less effective.
Keep a simple journal for a week. Write down how you feel each day - not just physical symptoms, but mood, energy, sleep. Then compare it to how you felt on the brand-name version. You might be surprised. Often, the difference isn’t in the pill - it’s in your attention to it.
And if you’re still unsure? Talk to your pharmacist. Ask: "Is this the same as the brand?" They can show you the bioequivalence data. They’ve seen this before. They know what to look for.
Why This Matters Beyond the Prescription Bottle
This isn’t just about saving money. It’s about access. If people stop taking their meds because they think the generic doesn’t work, their conditions get worse. Blood pressure rises. Depression deepens. Diabetes gets out of control. The nocebo effect doesn’t just hurt feelings - it hurts health.
And it’s preventable. We know how to fix it. We just need to stop treating patient perception as "irrational" and start treating it as part of the treatment plan.
Generic drugs are safe. They’re effective. They’re the reason millions of people can afford to stay healthy. But they won’t work if people believe they won’t. That’s the real challenge - not chemistry. Psychology.
What’s Next? The Future of Medication Perception
Researchers are now using fMRI scans to see how the brain reacts when people think they’re taking a generic. Early results show increased activity in areas linked to threat detection and pain processing - even when the pill is inert. This isn’t just about belief. It’s about brain wiring.
Some health systems, like Kaiser Permanente, now have official scripts for switching patients: "This medication contains the exact same active ingredient as what you were taking before, and studies show patients do just as well on the generic version." Simple. Clear. Evidence-based.
And in Europe, regulators are pushing for packaging that doesn’t alarm patients - but also doesn’t pretend to be the brand. It’s a tightrope. But progress is being made.
The goal isn’t to convince everyone that generics are perfect. The goal is to make sure the only thing changing when you switch is the price tag - not your health.
Are generic medications really the same as brand-name drugs?
Yes. Generic medications must contain the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They are required by the FDA to be bioequivalent - meaning they deliver the same amount of medicine into your bloodstream at the same rate. Studies show they work just as well for the vast majority of patients. The only differences are in inactive ingredients (like fillers or dyes) and packaging - neither of which affect how the drug works in your body.
Why do I feel worse after switching to a generic?
You may be experiencing the nocebo effect. This happens when negative expectations about a medication - like believing generics are inferior - cause your brain to interpret normal sensations as side effects. You might notice fatigue, headaches, or mood changes you didn’t pay attention to before. These aren’t caused by the drug itself, but by your belief about it. Keeping a symptom journal and talking to your doctor can help you tell the difference.
Can the packaging of a generic drug cause side effects?
Yes, indirectly. Packaging influences perception. A plain, unfamiliar-looking pill can trigger anxiety, which then leads to heightened awareness of normal body sensations. Studies have shown that people report more side effects from identical medications when they believe they’re taking a cheaper or less familiar version. The pill hasn’t changed - your brain’s interpretation has.
Should I ask my doctor to keep me on the brand-name drug?
If you’re doing well on a brand-name drug and switching causes distress, yes - talk to your doctor. But don’t assume the generic is the problem. Ask for a trial: stay on the generic for 4-6 weeks while tracking your symptoms. If you still feel worse, then consider switching back. Many people find their symptoms improve after a few weeks as their expectations adjust. Cost savings from generics can be substantial - over $3,000 a year per patient - so it’s worth exploring before making a permanent switch.
Do authorized generics have fewer side effects than regular generics?
Not necessarily. Authorized generics are made by the same company that makes the brand-name version - same factory, same formula. But if patients believe they’re still "just a generic," they can still experience the nocebo effect. The key isn’t who makes it - it’s how it’s presented. Even authorized generics can trigger side effect reports if patients are told they’re switching to a "cheaper alternative." The message matters as much as the medicine.
Can the nocebo effect be reversed?
Yes. Studies show that when patients are given clear, positive information - especially when paired with financial savings - nocebo effects drop significantly. Reassurance from a trusted provider, consistent messaging, and time usually help. Many patients who initially felt worse on generics report feeling normal again after a few weeks, once their expectations adjust. It’s not a permanent change - it’s a psychological response that can be corrected.




Katie Harrison
December 9, 2025 AT 04:58Just because it doesn’t have a fancy logo doesn’t mean it’s not doing the same job. Your body doesn’t care who made it. It cares if the molecule is there. And it is.
Mona Schmidt
December 11, 2025 AT 00:29Guylaine Lapointe
December 12, 2025 AT 17:59Christian Landry
December 14, 2025 AT 14:51turned out i was. 2 weeks later i forgot i was even on it. saved me $400/mo. also my dog now likes me again. 🤷♂️
Taya Rtichsheva
December 15, 2025 AT 13:31Asset Finance Komrade
December 16, 2025 AT 23:16Ruth Witte
December 17, 2025 AT 19:16It’s not the drug. It’s the ritual. We started putting little notes on the bottles: ‘Same medicine. Just a new face. You’ve got this.’ Guess what? Within 3 weeks, 70% said they felt better. 🤍
Noah Raines
December 19, 2025 AT 06:48