Every time you pick up a prescription, you get a little piece of paper with tiny text that feels like a puzzle. You might glance at it, nod, and toss it in your bag-until you forget how many pills to take, or worse, take the wrong one. But that label? It’s not just a receipt. It’s your safety net. And if you know what each part means, you can avoid dangerous mistakes, save time, and feel more in control of your health.
Your Name: The First Line of Defense
Right at the top, you’ll see your full name. It seems obvious, but this isn’t just for show. In the U.S., about 1.5 million medication errors happen every year-and many are because someone got another person’s pills. Your name on the label is the pharmacy’s way of saying, "This is for you, and only you." Always double-check it. If it says "John Smith" and you’re Jane Smith, don’t take it. Call the pharmacy right away. That one check could prevent a life-threatening mix-up.
Medication Name: Brand vs. Generic
You’ll see two names here. The first is the brand name-like "Abstral"-and below it, the generic name-"fentanyl." The brand name is what the drug company calls it. The generic name is the actual medicine inside. Fentanyl is fentanyl, no matter if it’s sold as Abstral, Fentora, or a generic version. Knowing the generic name helps you compare prices and understand what you’re really taking. Some people think generics are weaker, but they’re not. They have the same active ingredient, same dose, same effect. The only difference? Cost. Generics usually cost 80% less.
Dosage Strength: How Much Is in Each Pill?
This tells you the exact amount of medicine in each pill, tablet, or liquid dose. It might say "100 mcg" or "500 mg." That’s critical. Taking two 500 mg pills when you’re supposed to take one 1,000 mg pill is the same. But taking two 500 mg pills when you only need one 250 mg pill? That’s dangerous. Always read the number and unit carefully. "mcg" (micrograms) and "mg" (milligrams) look similar but are 1,000 times different. A mistake here can be fatal. If you’re unsure, ask your pharmacist to show you the difference on a syringe or pill splitter.
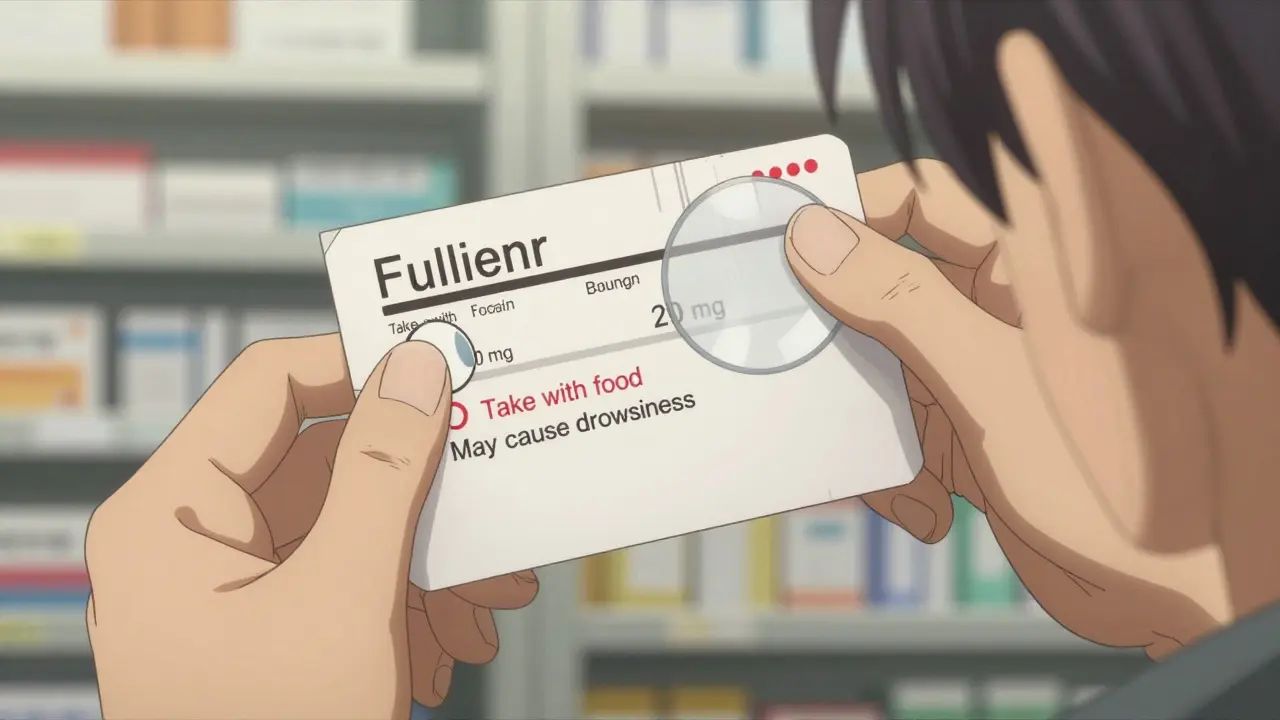
Instructions: When, How, and How Often
This is where most people get confused. It might say: "Take one tablet by mouth every 6 hours as needed for pain." That means: one pill, swallow it whole, every six hours, only if you’re in pain. Not every four hours. Not twice at once. Not with alcohol. Some labels say "take with food" or "on an empty stomach." Why? Because some drugs work better-or are less likely to upset your stomach-when taken with a meal. Others need to be absorbed quickly, so food slows them down. If the label says "take at bedtime," don’t take it at 3 p.m. Timing matters. And if you see "PRN," that’s medical shorthand for "as needed." Don’t assume it means "take daily." Ask if you’re not sure.
Expiration Date: When It Stops Working
That date on the label isn’t just a suggestion. After it, the medicine can lose strength-or even break down into something harmful. Most prescriptions are good for 12 to 18 months after being filled. But some, like insulin or liquid antibiotics, expire much faster. Never use medicine past its expiration date. If you’re unsure, bring it back to the pharmacy. They’ll dispose of it safely. And don’t store pills in the bathroom. Heat and moisture ruin them. Keep them in a cool, dry place-like a bedroom drawer.
Prescription Number (Rx#): Your Unique Code
This number, usually starting with "Rx," is like your medication’s ID tag. Every time you call for a refill, the pharmacist uses this number to pull up your exact prescription. If you switch pharmacies, they’ll need this number to transfer your script. Keep it handy. If you get a new bottle and the Rx number is different from last time, ask why. It could mean a new prescription was written, or there was a mistake. Always match the Rx number on the bottle to the one on your receipt or the one your doctor gave you.
Pharmacy Info: Who Filled It and Who to Call
This section has the pharmacy’s name, address, and phone number. It also lists your doctor’s name. Why? So you know where to call if something’s wrong. If you have side effects, if the pill looks different, if you’re confused about instructions-call the pharmacy. Pharmacists are trained to explain meds. They’re not just cashiers. In fact, studies show that patients who talk to their pharmacist when they get a new prescription are 28% more likely to take it correctly. Don’t hesitate. That number is there for you.
Visual Description: What the Pill Looks Like
Ever opened a bottle and thought, "This doesn’t look right"? That’s because pills change. The same drug can come in different colors, shapes, or imprints depending on the manufacturer. The label might say: "White, round, film-coated tablet, imprinted with 'ABC 50'." That’s your visual fingerprint. If your next refill looks totally different-say, blue instead of white, or oval instead of round-don’t assume it’s the same. Call the pharmacy. It could be a generic switch (common and safe), or it could be a mistake. Always compare the visual description to what’s in the bottle.
National Drug Code (NDC): The Universal Barcode
This 10- or 11-digit number is the drug’s official fingerprint in the U.S. system. It tells you who made it, what the product is, and what size bottle it’s in. You won’t need to use it unless you’re filing insurance, reporting an error, or checking recall notices. But if you ever get a recall notice in the mail, the NDC is how you know if your bottle is affected. Write it down or take a photo of it when you get your prescription. Keep it with your medical records.
Storage Instructions: Keep It Safe
Some meds need to be refrigerated. Others must stay away from light or humidity. The label might say: "Store at 20°C to 25°C (68°F to 77°F)." That’s room temperature. Don’t leave them in your car in summer. Don’t put them in the bathroom cabinet. Some, like epinephrine pens, need to be kept at cool temps. Others, like certain antibiotics, can become toxic if stored wrong. Always follow the storage instructions. If it says "Do not freeze," don’t. If it says "Protect from light," keep it in the original bottle. These aren’t suggestions-they’re science.

Warnings: The Red Flags
This section is the most important. It tells you what could go wrong. It might say: "Avoid alcohol," "May cause drowsiness," "Do not use if pregnant," or "Risk of severe allergic reaction." These aren’t just fine print. They’re lifesavers. For example, mixing certain painkillers with alcohol can cause liver failure. Some blood pressure meds can drop your blood pressure too low if you’re dehydrated. If you see a warning you don’t understand, ask your pharmacist to explain it in plain English. Don’t skip this part. It’s not there to scare you-it’s there to keep you safe.
The Hidden Gem: The Medication’s Purpose
Here’s something many labels still don’t include-but they should: why you’re taking this medicine. Is it for high blood pressure? Diabetes? Anxiety? Depression? If it’s not written on the label, ask. A 2020 FDA study found that 78% of patients took their meds wrong because they didn’t know the reason. One woman in a Cleveland Clinic study took insulin because she thought it was for her joint pain. She almost died. Including the purpose on the label reduces wrong-medication errors by 55%, according to the Institute for Safe Medication Practices. If your label doesn’t have it, request it. More pharmacies are starting to add it-especially since 2023, when the FDA pushed for clearer labeling. You have the right to know why you’re taking something.
What’s Missing? What You Should Ask
Even with all this info, labels aren’t perfect. Many still use confusing abbreviations like "q.d." (once daily) or "tsp" (teaspoon). The FDA recommends spelling everything out: "once daily," "teaspoon." If you see abbreviations, ask for clarification. Also, ask: "What side effects should I watch for?" and "What happens if I miss a dose?" Don’t wait until you feel bad. Get answers before you leave the pharmacy.
Use the "5 Questions" method the FDA recommends:
- What’s the name of this medicine, and what is it for?
- How and when do I take it?
- What if I miss a dose?
- What side effects should I expect?
- Will this interact with my other meds or supplements?
And remember the "Ask Me 3" rule: Know your main problem. Know what you need to do. Know why it’s important.
What to Do If Something Doesn’t Add Up
If the pill looks wrong, the instructions are unclear, or your name is misspelled-don’t guess. Call the pharmacy. Bring the bottle back. Ask to speak to the pharmacist. Most pharmacies have a medication therapy management program where they review all your drugs and catch interactions you didn’t know about. And if you’re over 65, on five or more meds, or have memory issues, ask about a MedsCheck. It’s free, takes 20 minutes, and can prevent hospital visits.
Medication errors cause about 7,000 deaths in the U.S. every year. Most are preventable. You don’t need to be a doctor to read your label. You just need to be curious. And a little careful.
Why does my prescription label have both a brand and generic name?
The brand name is what the drug company calls the medicine-for marketing. The generic name is the actual active ingredient. For example, "Lipitor" is the brand; "atorvastatin" is the generic. Both contain the same medicine. Generics are cheaper and just as effective. Seeing both helps you compare prices and avoid accidentally taking two versions of the same drug.
What does "PRN" mean on my prescription label?
"PRN" stands for "pro re nata," a Latin term meaning "as needed." It doesn’t mean take it every day. For example, if your label says "Take one tablet PRN for pain," you only take it when you feel pain-not every 4 hours unless you’re in pain. Always check with your pharmacist if you’re unsure how often you’re allowed to take it.
Is it safe to take medicine after the expiration date?
Generally, no. After the expiration date, the medicine may lose strength, or break down into harmful substances. Some, like insulin or liquid antibiotics, become unsafe quickly. Others might still work but won’t be as effective. The FDA advises against using expired meds. If you’re unsure, bring the bottle to your pharmacy-they’ll dispose of it safely.
Why doesn’t my label say why I’m taking this drug?
Many labels still don’t include the reason, even though it’s strongly recommended. The FDA says 78% of patients take meds incorrectly because they don’t know why they were prescribed. If your label doesn’t say it, ask your pharmacist or doctor. You have the right to know. Many pharmacies now add it voluntarily, especially since 2023, when new guidelines pushed for clearer labeling.
What should I do if my pill looks different this refill?
Don’t take it. Compare the visual description on the label (color, shape, imprint) to what’s in the bottle. If they don’t match, call the pharmacy. It could be a switch to a generic version (which is safe), or it could be a mistake. Always verify before swallowing. Never assume it’s the same pill just because the name is the same.
Next Steps: Make Your Labels Work for You
Start today. When you get a new prescription, pause before leaving the pharmacy. Read the label. Ask the five questions. Write down the purpose of the medicine if it’s not there. Take a photo of the label on your phone. Keep it in your notes app. If you’re on multiple meds, use a pill organizer with labels. And if you ever feel confused-call your pharmacist. They’re paid to help you understand this stuff. You’re not bothering them. You’re using their expertise.
Medication safety isn’t just the doctor’s job. It’s yours too. And the little label on your bottle? It’s your most powerful tool.






Sue Stone
January 23, 2026 AT 03:20Just read this while waiting for my refill. Honestly? I’ve been ignoring my labels for years. Now I’m going back to check every single one. That visual description thing? I once took a blue pill thinking it was my usual white one. Turned out it was my mom’s blood pressure med. Scary stuff.
Thanks for the reminder to actually read the damn thing.
Stacy Thomes
January 23, 2026 AT 21:38THIS. THIS IS SO IMPORTANT. I almost died because I didn’t know ‘PRN’ meant ‘as needed’ and not ‘every 4 hours.’ My pharmacist had to call me at 2 a.m. because I was passed out from too much painkiller. Don’t be like me. Read the label. Ask questions. Your life depends on it.
Susannah Green
January 24, 2026 AT 17:08Always write down the purpose-even if it’s not on the label. I keep a little notebook: ‘Metformin = for diabetes (not weight loss).’ ‘Lisinopril = for BP (not for headaches).’ I even color-code them now. Green = safe, red = dangerous interactions. It’s saved me so many times.
Also: never trust the pharmacy’s handwriting. Always double-check the Rx number. I once got someone else’s thyroid med. I noticed because the pill was a different shape. Thank God I checked.
Andrew Smirnykh
January 25, 2026 AT 18:37It’s wild how much we just hand over our health to strangers. Pharmacies are busy, doctors are rushed, but the label is the one thing that doesn’t change. I always take a photo of the label right after I get it. Then I compare it to the next refill. If anything’s off-color, shape, size-I call before swallowing. Simple. No drama. Just safety.
Also, the NDC code? I saved mine in my phone notes. When the recall came for that batch of metformin last year, I knew instantly mine was affected. Saved me a trip to the ER.
charley lopez
January 27, 2026 AT 06:50The pharmacokinetic variability of generic formulations is often overstated. Bioequivalence thresholds are strictly regulated by the FDA under 21 CFR 314.94. The active pharmaceutical ingredient is identical. The excipients may differ, but these do not alter therapeutic efficacy in the vast majority of cases. Clinical outcomes are statistically indistinguishable in peer-reviewed meta-analyses.
That said, patient adherence improves significantly with clear labeling. The omission of indication remains a systemic failure in U.S. pharmacy practice, despite the 2023 FDA guidance. Documentation of purpose should be mandatory, not optional.
Dawson Taylor
January 27, 2026 AT 17:18Labels aren’t perfect. But they’re the best tool we’ve got.
Read them. Question them. Don’t assume.
That’s it.
Anna Pryde-Smith
January 28, 2026 AT 01:56Ugh. I just got my new prescription and the pill is a different color. I called the pharmacy and they said, ‘Oh, we switched generics.’ I said, ‘But the label didn’t say that!’ They said, ‘It’s fine.’ Fine? Fine?! I could’ve had a stroke because some corporate cost-cutting decision didn’t get printed on the damn label!
Someone needs to sue these places. This isn’t customer service-it’s a gamble with people’s lives.
Laura Rice
January 29, 2026 AT 05:34my grandma used to say: ‘if it doesn’t say why you’re takin’ it, ask.’ she was right. i took my dad’s blood pressure med once because i thought it was for ‘feeling tired.’ turned out he was on it for kidney issues. i almost passed out. now i always write the reason on the bottle with a sharpie. ‘for heart’ ‘for nerves’ ‘for sugar’ - simple. clear. no confusion.
also: don’t store meds in the bathroom. i learned that the hard way. my insulin went bad and i didn’t know until i was shaking at 3 a.m. 🤦♀️
Kerry Evans
January 30, 2026 AT 08:04People don’t read labels because they’re lazy. I’ve seen it a hundred times. ‘Oh, the pharmacist explained it.’ No, they didn’t. They handed you the bottle and said ‘take one.’ That’s not counseling. That’s negligence. If you don’t know the difference between mcg and mg, you shouldn’t be taking prescription meds. Period.
And yes, generics are fine. But if you’re still using expired insulin because ‘it looks okay,’ you’re not just irresponsible-you’re a danger to yourself and others.
Janet King
January 31, 2026 AT 04:04Always ask for the purpose. If it's not on the label, request it. The FDA recommends it. Pharmacies are required to provide it upon request. You have rights. Write it down. Keep a list. Share it with your doctor during visits. Medication errors are preventable. Knowledge is the first step. Do not rely on memory. Do not assume. Confirm. Always.