Why Your Prescription Label Matters More Than You Think
Every time you pick up a new prescription, you’re handed a small piece of paper that could mean the difference between feeling better and ending up in the hospital. Prescription labels aren’t just paperwork-they’re your safety guide. In the U.S., nearly 1.5 million people are hurt each year by medication errors, and many of those mistakes happen because someone didn’t understand what the label actually said. The good news? You don’t need to be a doctor to read it right. You just need to know what to look for.
The 12 Key Parts of a Prescription Label
Every prescription label has the same basic structure, no matter which pharmacy you go to. Here’s what’s on it, and why each part matters:
- Your full name - This isn’t just for show. It stops someone else from accidentally taking your medicine. If your name is even slightly wrong, don’t take it. Call the pharmacy right away.
- Medication name - You’ll see two names: the brand name (like "Lipitor") and the generic name (like "atorvastatin"). In the U.S., the brand name usually comes first. In Canada, the generic name is listed first. Either way, make sure you recognize the drug. If you’ve taken it before, compare the name and how the pill looks to your last bottle.
- Prescription number (Rx#) - This is your prescription’s ID number. It’s how the pharmacy finds your record when you call for a refill. Keep it handy.
- Prescriber’s name - This tells you who ordered the medicine. It could be your doctor, nurse practitioner, dentist, or even a vet if it’s for a pet. If you didn’t see this person recently, double-check with your doctor.
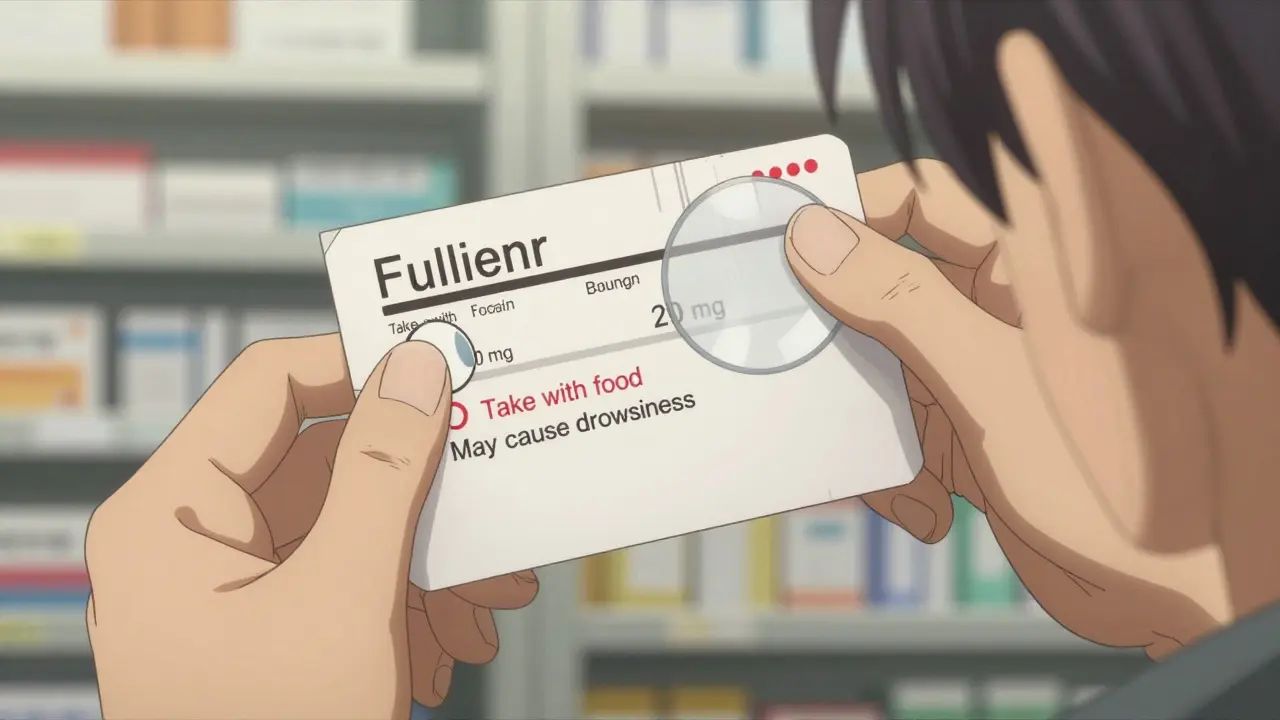
- Medication strength - This tells you how much of the drug is in each pill or dose. "20 mg" means 20 milligrams per tablet. Never assume the strength is the same as your last prescription. A change in strength can be dangerous if you don’t notice it.
- Quantity - This shows how many pills, milliliters, or grams you got. If your bottle has 30 pills but your label says "90," something’s wrong.
- Discard or expiration date - Most prescriptions expire one year after being filled. After that, the medicine may not work as well-or could even become unsafe. Never take medicine past this date.
- Instructions - This is the most important part. It tells you how to take the medicine: "Take one tablet by mouth twice daily." But here’s the catch: 79% of people misread these instructions. "Twice daily" doesn’t mean "every two hours." It means morning and night. "Every 12 hours" is more precise. If it says "as needed," ask what that means for your condition.
- Refill info - It might say "Refills: 3" or "No refills." If you run out before your next appointment, you’ll need a new prescription. Don’t wait until you’re out to call.
- Auxiliary labels - These are the small stickers on the bottle with extra warnings: "Take with food," "May cause drowsiness," "Refrigerate," or "Avoid alcohol." These aren’t optional. They’re there for your safety.
- Pharmacy info - The name, phone number, and address of the pharmacy. Keep this. If you have questions, this is who to call. Some labels also have a barcode-this helps the pharmacy track your meds.
What Most People Get Wrong
Even when labels are written clearly, people still misunderstand them. The most common mistakes:
- Thinking "twice daily" means every 12 hours-but not realizing that means you need to take it at 8 a.m. and 8 p.m., not whenever you remember.
- Ignoring "take with food" and taking the pill on an empty stomach, which can cause nausea or make the drug less effective.
- Not checking the strength. Someone might get a 10 mg pill instead of a 20 mg pill and assume it’s the same.
- Missing auxiliary labels. "Avoid sunlight" on a tetracycline label? If you don’t see it, you might get a bad sunburn.
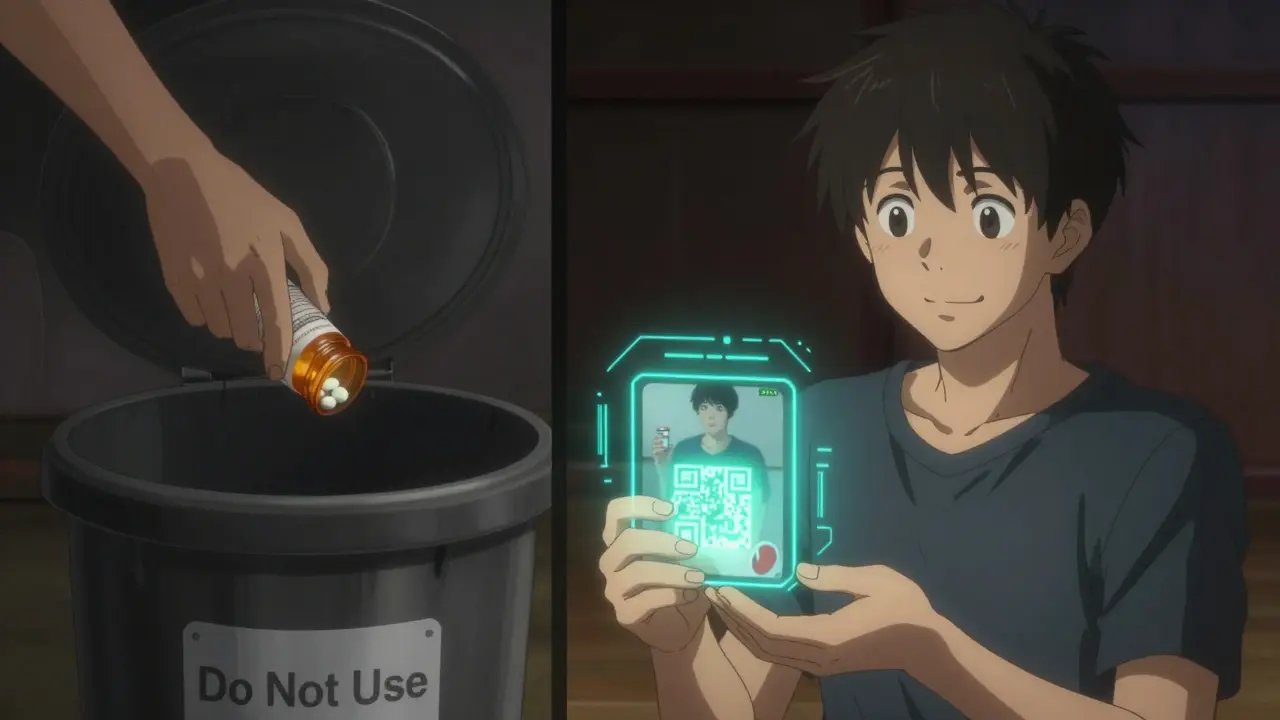
- Using old prescriptions. If your doctor changed your dose, your old bottle might still be sitting in your cabinet. Throw it out.
A study by the NIH found that people with low health literacy were more than twice as likely to make these mistakes-even when the wording was simple. That’s why asking for help isn’t a sign of weakness. It’s smart.
How to Check Your Label Before Taking Anything
Before you swallow any pill, pause and run through this quick checklist:
- Is this medicine for me? - Look at your full name. No nicknames. No "Mr. Smith" if your name is Mary Smith.
- Does the name match what my doctor told me? - If your doctor said "cholesterol pill," and the label says "atorvastatin," that’s fine. But if it says "metformin," that’s for diabetes. Double-check.
- Is the strength right? - If you used to take 10 mg and now it’s 20 mg, ask why. Don’t assume it’s an upgrade.
- Do I understand the instructions? - Say them out loud: "I take one tablet in the morning and one at night." If you’re unsure, don’t guess.
- Are there any special warnings? - "Don’t drink alcohol," "May cause dizziness," "Keep refrigerated"-these matter. Skip them at your risk.
- Is it still good? - Check the expiration date. If it’s more than a year old, don’t use it.
- Do I know who to call if I have questions? - Write down the pharmacy number. Keep it on your fridge or in your phone.
What to Do If Something Doesn’t Look Right
Pharmacists are trained to catch mistakes. They’re not just there to hand out pills. If anything seems off-wrong name, wrong pill color, confusing instructions-ask them. Don’t wait. Don’t be shy. Say: "I’m not sure I understand this. Can you walk me through it?"
Many pharmacies now offer free 5-minute consultations when you pick up a new prescription. Use them. Ask them to point out each part of the label. If you’re not fluent in English, ask for a translator. Many pharmacies have phone or app-based translation services.
And if you’re helping an older parent or someone with memory issues, go with them. Read the label together. Write down the instructions in big letters on a sticky note. Put it on the bathroom mirror.
What’s Changing on Prescription Labels
Pharmacies are slowly making labels easier to read. The FDA pushed for clearer language in 2014, banning phrases like "q.d." and "b.i.d." (medical abbreviations) in favor of plain English: "once daily," "twice daily."
Now, some pharmacies are testing QR codes on labels. Scan one with your phone, and you’ll get a short video showing how to take the medicine-in your language. In pilot programs, this cut misinterpretation by 40% among non-native speakers.
By 2025, most U.S. pharmacies will offer digital label options through their apps. You’ll get reminders, explanations, and even alerts if you’re taking something that interacts badly with another drug.
But until then, the paper label is still your main tool. And you’re the only one who can make sure you read it right.
Why This Saves Money-and Lives
Medication errors cost the U.S. healthcare system over $3.5 billion a year. Many of those costs come from emergency visits and hospital stays that could have been avoided.
People who understand their labels are 28% more likely to take their medicine correctly. That means fewer flare-ups, fewer trips to the doctor, and better health overall.
It’s simple: if you know what you’re taking and why, you’re less likely to get sick. And that’s the best kind of medicine.
What if my prescription label has a different name than what my doctor told me?
It’s common to see both a brand name and a generic name on the label. For example, "Lipitor" is the brand, and "atorvastatin" is the generic. Both are the same medicine. But if the name is completely different-like your doctor prescribed blood pressure medicine but the label says insulin-call the pharmacy immediately. This could be a serious error.
Can I take medicine past the expiration date?
Most medications are safe for a year after being filled, but they start to lose effectiveness after that. Some, like insulin or liquid antibiotics, can become dangerous. Never take expired medicine unless a pharmacist or doctor says it’s okay. When in doubt, throw it out.
What does "take with food" really mean?
"Take with food" means eat something-like a snack or a meal-when you take the pill. It helps your stomach handle the medicine better and can improve how well your body absorbs it. Don’t just sip water. Eat something solid. A cracker or a piece of toast is enough.
Why does my label say "refills: 0" when I still have pills left?
Some prescriptions are meant to be short-term, like antibiotics or painkillers after surgery. Even if you have pills left, you can’t refill it without a new prescription. This is by design-it keeps you from using the medicine longer than your doctor intended. Call your doctor if you still need it after finishing the course.
Can I split my pills if the label doesn’t say to?
Only if the pill has a score line (a groove down the middle) and your doctor or pharmacist says it’s okay. Some pills are designed to release medicine slowly. Splitting them can make them unsafe. Never split pills without checking first.
What should I do if I accidentally take the wrong dose?
Don’t panic. Call your pharmacist or doctor right away. If it’s after hours, call Poison Control at 1-800-222-1222 (in the U.S.) or your local emergency number. Don’t wait to see if you feel sick. Even small mistakes can be dangerous with certain drugs like blood thinners or diabetes meds.






Kacey Yates
January 30, 2026 AT 05:43ryan Sifontes
January 31, 2026 AT 15:50Laura Arnal
February 1, 2026 AT 07:22Pawan Kumar
February 1, 2026 AT 20:10Jasneet Minhas
February 2, 2026 AT 09:52Eli In
February 4, 2026 AT 01:45Megan Brooks
February 5, 2026 AT 12:26Sheryl Dhlamini
February 7, 2026 AT 01:33Doug Gray
February 7, 2026 AT 09:04LOUIS YOUANES
February 7, 2026 AT 11:51Laia Freeman
February 8, 2026 AT 06:42rajaneesh s rajan
February 8, 2026 AT 17:04paul walker
February 10, 2026 AT 01:55Alex Flores Gomez
February 11, 2026 AT 07:34Frank Declemij
February 13, 2026 AT 00:39