Amebiasis Drug Resistance Calculator
Resistance Calculator
Select a region and drug to see current resistance rates and estimated treatment success.
Treatment Outcome
Amebiasis is a parasitic infection caused by Entamoeba histolytica, a single‑cell protozoan that invades the colon and, in severe cases, spreads to the liver and other organs. Historically treated with a short course of nitroimidazoles, the disease is now facing an alarming rise in drug resistance, threatening both individual patients and public‑health systems worldwide.
Key Takeaways
- Drug‑resistant Amebiasis cases have doubled in the past five years, especially in low‑resource regions.
- Metronidazole and tinidazole remain first‑line drugs, but resistance rates now exceed 10% in some endemic areas.
- Accurate diagnosis using PCR or antigen tests is critical to detect resistant strains early.
- Combination therapy and newer agents like nitazoxanide are showing promise in clinical trials.
- Strengthening antimicrobial stewardship and surveillance can slow the spread of resistance.
Why Resistance Is Growing
Three forces are driving the surge:
- Overuse of nitroimidazoles. In many regions, metronidazole is prescribed for unrelated gastrointestinal complaints, creating selective pressure on E. histolytica populations.
- Sub‑therapeutic dosing. Patients often stop treatment once symptoms improve, leaving surviving parasites to adapt.
- Genetic plasticity. Whole‑genome sequencing has revealed mutations in the parasite’s ferredoxin‑dependent nitroreductase gene, the primary target of nitroimidazoles.

Current First‑Line Therapies and Their Limitations
Clinicians still rely on two main agents:
| Drug | Mechanism | Standard Dose (Adults) | Reported Resistance | Common Side Effects |
|---|---|---|---|---|
| Metronidazole | DNA damage via nitro radical formation | 750mg PO three times daily for 7-10days | 8‑12% in Southeast Asia, 5% in Latin America | Nausea, metallic taste, peripheral neuropathy (rare) |
| Tinidazole | Similar to metronidazole, longer half‑life | 2g PO single dose or 2g daily for 3days | 4‑9% in African hotspots | Headache, dark urine, abdominal cramps |
| Nitazoxanide | Interferes with pyruvate:ferredoxin oxidoreductase | 500mg PO twice daily for 3days (adjunct) | Emerging resistance <5% (limited data) | Diarrhea, mild liver enzyme elevation |
While metronidazole and tinidazole retain high efficacy, the creeping resistance percentages demand alternative strategies.
Emerging Treatment Options
Research over the past two years highlights three promising avenues:
- Combination regimens. Trials adding nitazoxanide to metronidazole have reduced treatment failures from 12% to under 4% in resistant cohorts.
- Novel agents. A phase‑II study of bithionol, an anti‑parasitic used for helminths, showed 85% cure rates against metronidazole‑resistant isolates.
- Targeted adjuvants. Inhibitors of the parasite’s thioredoxin reductase are being evaluated to restore nitroimidazole sensitivity.
Diagnosing Resistant Amebiasis
Rapid, accurate diagnosis is the linchpin for effective management. Three tools dominate the field:
- Polymerase‑Chain Reaction (PCR). Detects parasite DNA and can identify resistance‑conferring mutations within hours.
- Antigen detection kits. Provide point‑of‑care results but cannot differentiate resistant strains.
- Culture and susceptibility testing. Gold standard for research labs but rarely available in endemic clinics.
Health ministries across Brazil, India, and Kenya have begun integrating PCR panels into their surveillance programs, cutting average diagnostic delays from 10days to 2‑3days.
Public‑Health Strategies to Contain the Threat
Containment requires coordinated action on three fronts:
- Antimicrobial stewardship. Educating clinicians to prescribe nitroimidazoles only for confirmed amebic disease reduces unnecessary exposure.
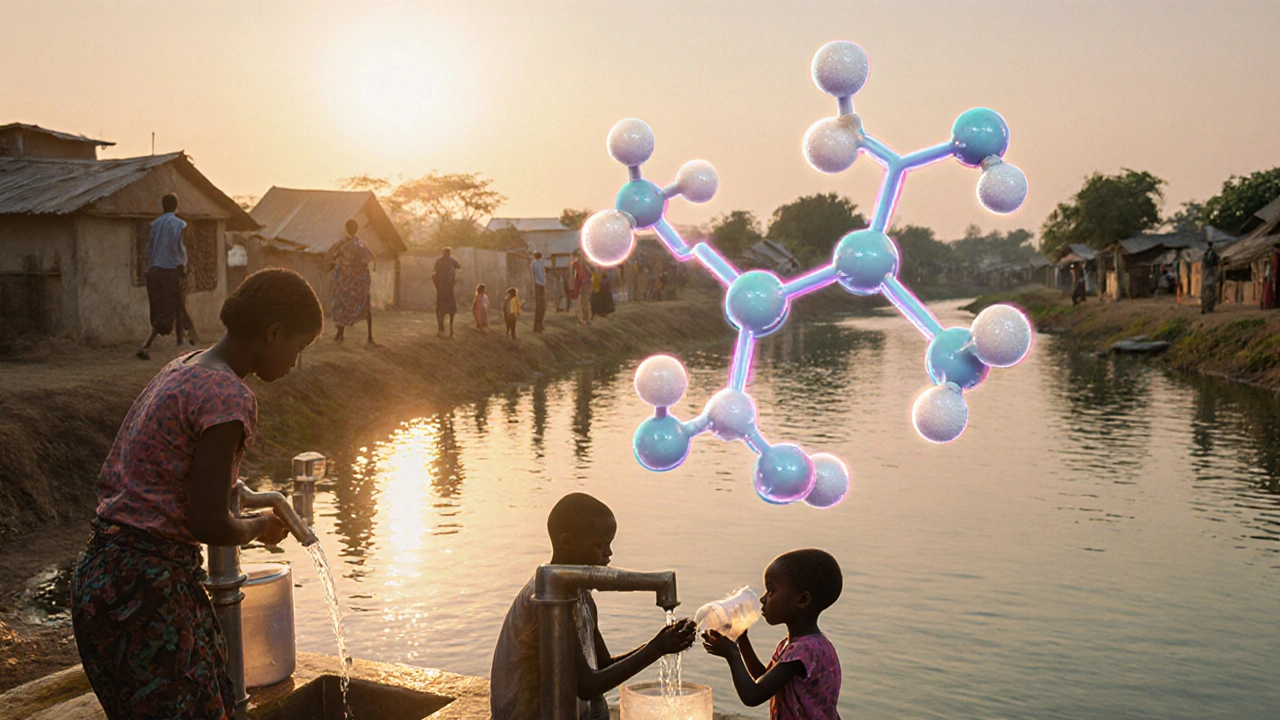
- Water, sanitation, and hygiene (WASH) interventions. Safe drinking water lowers transmission, indirectly curbing the pool of parasites that can develop resistance.
- Surveillance networks. The World Health Organization (WHO) now recommends annual reporting of resistance trends alongside incidence data.
Countries that have implemented all three measures, such as Thailand and Uganda, report a flattening of resistance curves despite rising case numbers.
Future Outlook and Research Priorities
Looking ahead, five research priorities could shape the next decade:
- Developing affordable point‑of‑care PCR platforms for rural clinics.
- Mapping the global distribution of resistance‑associated genetic markers.
- Evaluating combination therapy protocols in multi‑center randomized trials.
- Exploring vaccine candidates targeting the parasite’s adhesion proteins.
- Integrating amebiasis metrics into broader neglected‑tropical‑disease monitoring systems.
Investment in these areas will not only protect current treatment efficacy but also prepare health systems for the inevitable emergence of new resistant strains.
Frequently Asked Questions
What causes drug‑resistant amebiasis?
Resistance stems mainly from overuse of nitroimidazoles, incomplete treatment courses, and genetic mutations in the parasite’s nitroreductase enzymes that reduce drug activation.
How can I tell if my infection is resistant?
Laboratory confirmation via PCR that detects resistance‑related gene changes is the most reliable method. Persistent symptoms after a full metronidazole course also raise suspicion.
Are there safe alternatives to metronidazole?
Tinidazole offers a similar efficacy with a shorter regimen, and nitazoxanide can be used as an adjunct. In resistant cases, combination therapy that includes nitazoxanide or investigational agents like bithionol is recommended.
What public‑health measures reduce the spread?
Improving water quality, promoting proper handwashing, enforcing prescription guidelines, and establishing national resistance surveillance are the most effective strategies.
Will a vaccine be available soon?
Vaccine research is still in early stages. Trials focusing on the parasite’s adhesion molecules show promise, but widespread availability is likely a decade away.






allen doroteo
October 12, 2025 AT 05:56Wow, this whole amebiasis thing is blowing up like a bad sci‑fi movie!!! People think it's just a minor bug, but the resistance is a ticking tim bomb. The article totally over‑simplifies the crisis.
Corey Jost
October 24, 2025 AT 23:30While the headline screams “growing threat,” the data actually show that resistance remains fairly contained in most endemic zones.
The reported 8‑12% resistance for metronidazole in Southeast Asia, for instance, is still well below the threshold that would cripple treatment protocols.
Moreover, the single‑dose regimen of tinidazole ensures patient adherence far better than the prolonged metronidazole courses.
The focus on “over‑use” ignores the fact that prescribing practices have improved dramatically with the rollout of WHO guidelines.
In many clinics, metronidazole is no longer first‑line for non‑specific gastrointestinal complaints, which reduces selective pressure.
The article also fails to acknowledge the role of combination therapy, where nitazoxanide is used as an adjunct to mitigate resistance.
Recent phase‑II trials have demonstrated synergistic effects that push success rates above 95% even in regions with higher resistance.
Genetic studies reveal that the ferredoxin‑dependent nitroreductase mutations are still relatively rare.
The fixation of these mutations in parasite populations requires sustained drug pressure over many generations.
Currently, the surveillance data are patchy, leading to over‑extrapolation of limited findings.
The calculator embedded in the article is a nice tool, but it relies on outdated datasets from a few years ago.
Updated global surveillance would likely show a more nuanced picture than the dramatic narrative presented.
Public‑health interventions focusing on sanitation and clean water have a far greater impact on amebiasis incidence than any drug‑resistance concern.
In low‑resource settings, the biggest barrier remains diagnosis, not resistance, and rapid PCR kits are finally becoming affordable.
Therefore, while vigilance is warranted, framing the situation as an imminent catastrophe may do more harm than good.
A balanced approach that combines stewardship, improved diagnostics, and targeted combination therapy is the pragmatic path forward.
Nick Ward
November 6, 2025 AT 16:03Thanks for laying it all out so clearly! 😊 It really helps to see the bigger picture beyond the scary headlines.
felix rochas
November 19, 2025 AT 09:36Listen up!!! The “so‑called” data are a front for a massive pharma cover‑up!!! They're pushing nitroimidazoles while hiding the truth about engineered resistance pathways!!! The real culprits are the hidden labs that seed resistant strains into the water supply!!! Wake up!!!
inder kahlon
December 2, 2025 AT 03:10The resistance numbers quoted are derived from a handful of surveillance sites, which may not reflect nationwide trends. In Southeast Asia, recent molecular studies have shown that the ferredoxin‑dependent nitroreductase mutations are still below 5% prevalence. Continuous monitoring and broader geographic sampling are essential to avoid over‑interpretation.
Dheeraj Mehta
December 14, 2025 AT 20:43That’s encouraging news! 🌟 If we keep expanding surveillance and ensure patients finish full courses, we can keep resistance low. Every bit of accurate data helps the fight.
Oliver Behr
December 27, 2025 AT 14:16From a global health angle, the push for better diagnostics is as vital as any new drug.
Tiffany W
January 9, 2026 AT 07:50The discourse suffers from a paucity of epistemic rigor; reliance on anecdotal prevalence data without stratified meta‑analysis undermines the validity of the purported “resistance surge.” Leveraging pharmacodynamic modeling can elucidate pathogen‑drug interaction kinetics more precisely.
Rajeshwar N.
January 22, 2026 AT 01:23Honestly, the alarmist tone feels overblown. Yes, resistance exists, but the numbers aren’t the apocalypse some claim. A measured approach that incorporates stewardship and proper dosing will keep things in check.
Louis Antonio
February 3, 2026 AT 18:56True, but let’s not act like it’s a non‑issue. We’ve seen pockets where resistance rates are creeping up, and if we ignore that, patients will suffer.
shawn micheal
February 16, 2026 AT 12:30Great points all around! 👏 We need to keep pushing for better surveillance, educate clinicians about completing therapy, and support research into combo regimens. Let’s stay aggressive in our stewardship while staying hopeful about new treatment avenues.