Diabetic retinopathy doesn’t come with warning signs. You might feel fine, see clearly, and think your diabetes is under control-until one day, your vision gets blurry, or you start seeing floaters like dark cobwebs drifting across your sight. By then, the damage is already done. This isn’t rare. About 1 in 3 people with diabetes in the U.S. develop some form of diabetic retinopathy. And it’s the leading cause of vision loss in adults between 21 and 64.
How High Blood Sugar Attacks the Retina
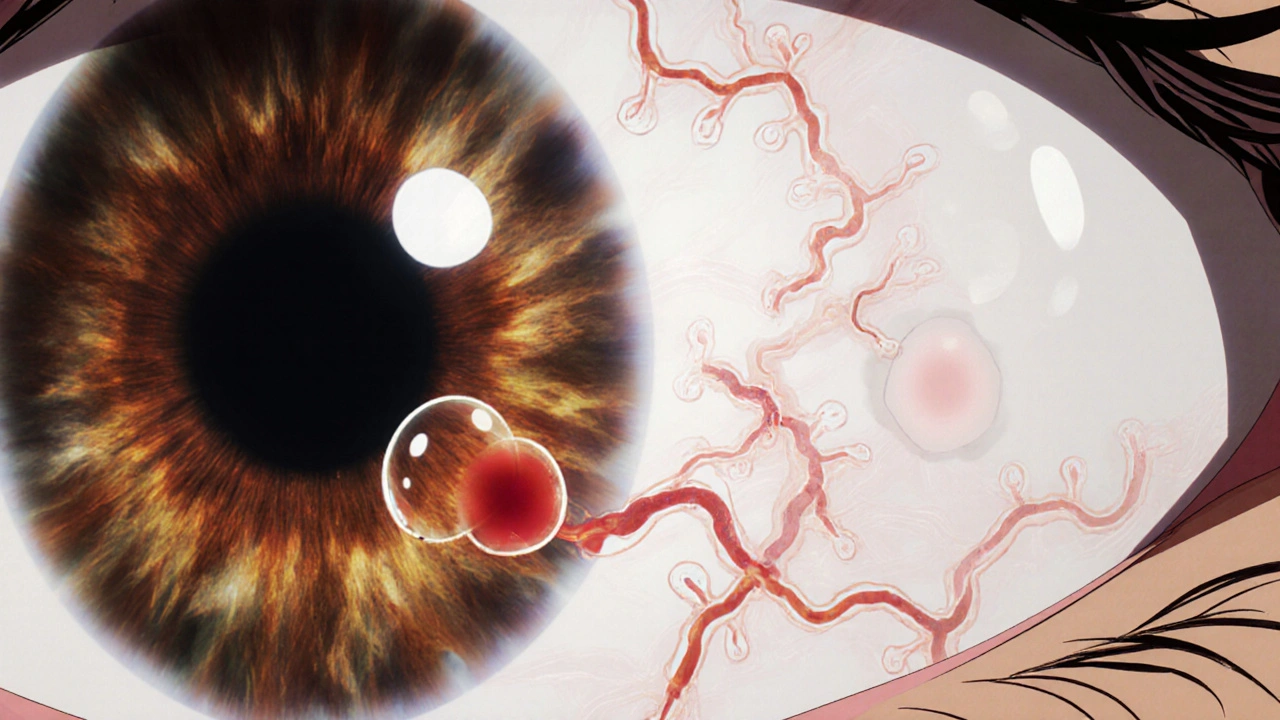
Your retina is the light-sensitive layer at the back of your eye. It turns light into signals your brain turns into images. But it’s also packed with tiny blood vessels-so delicate, so vital. When blood sugar stays high for years, those vessels get damaged. It’s not just a slow leak; it’s a slow breakdown. High glucose thickens the walls of blood vessels and weakens them. Over time, they bulge out into tiny balloons called microaneurysms. These can leak fluid and blood into the retina. When fluid collects in the macula-the center of your vision responsible for sharp, detailed sight-it causes diabetic macular edema. That’s when things get blurry, especially when reading or recognizing faces. But the damage doesn’t stop there. As vessels get blocked, parts of the retina are starved of oxygen. The eye tries to fix this by growing new blood vessels. But these aren’t normal. They’re fragile, messy, and prone to bleeding. They can tear the retina, cause scar tissue to form, or even trigger glaucoma by blocking fluid drainage. This is proliferative diabetic retinopathy-the most dangerous stage. And here’s the cruel part: you won’t feel it until it’s advanced. Most people don’t notice anything until their vision is already fading. That’s why screening isn’t optional. It’s your first and best defense.The Three Stages of Retinal Damage
Diabetic retinopathy doesn’t jump from normal to blind. It creeps forward in stages:- Mild nonproliferative: Small microaneurysms appear. No symptoms yet. Just tiny weak spots in the vessel walls.
- Moderate to severe nonproliferative: More vessels get blocked. The retina may swell. Bleeding starts. Vision might get slightly hazy, but many still don’t notice.
- Proliferative: New, abnormal blood vessels grow on the retina’s surface. These bleed into the vitreous-the gel inside your eye-causing sudden floaters, dark spots, or even vision loss. Scar tissue can pull the retina loose from the back of the eye, leading to detachment.
Diabetic macular edema can happen at any stage, even early on. It’s not a separate disease-it’s a complication that makes vision worse, faster.
Why You Can’t Wait for Symptoms
If you have diabetes, waiting for blurry vision is like waiting for a fire alarm before you call the firefighters. By the time you notice symptoms, up to 68% of patients already have moderate or severe damage. Symptoms that do show up include:- Blurred or wavy vision
- Floaters or dark spots that don’t go away
- Difficulty seeing at night or in low light
- Fading or washed-out colors
- Loss of peripheral vision
- Sudden vision loss from bleeding inside the eye
Many people think their vision fluctuates because of tiredness or screen use. But if you have diabetes and your vision changes-especially if it comes and goes-get checked. That’s often the first sign your retina is struggling.

Laser Treatment: How It Works and What to Expect
Laser treatment, or photocoagulation, has been the go-to option for decades. It’s not glamorous. It doesn’t restore lost vision. But it stops things from getting worse-and it works. There are two main types:- Focal/grid laser: Used for diabetic macular edema. The laser targets specific leaking vessels in the macula to seal them off and reduce swelling.
- Scatter (panretinal) laser: Used for proliferative retinopathy. Dozens to hundreds of tiny laser burns are placed across the peripheral retina. This doesn’t help your side vision, but it reduces the eye’s signal to grow new, harmful blood vessels.
It’s done as an outpatient procedure. Your eye is numbed with drops. You might feel a slight pressure or a quick flash of light with each laser pulse. No stitches. No overnight stay.
Success isn’t about curing-it’s about saving what’s left. Studies show that with timely laser treatment, patients have a 95% chance of avoiding severe vision loss. That’s not a guarantee of perfect sight, but it’s a guarantee you won’t go blind from this.
It’s not painless. After the procedure, your vision might be blurry for a day or two. You might see glare or dark spots. Night vision can be permanently affected, especially after scatter laser. But compared to the risk of total vision loss, that’s a trade-off most people accept.
It’s Not Just About the Laser
Laser treatment doesn’t fix diabetes. It just treats the side effect. The real power comes from controlling your blood sugar. Research shows that keeping your HbA1c below 7% slows retinopathy progression by up to 76%. That’s not a suggestion-it’s a medical fact. Every point you drop in your HbA1c reduces your risk. Consistent control matters more than perfection. High blood pressure and high cholesterol make things worse. Smoking doubles your risk. Pregnancy can speed up damage in women with diabetes. These aren’t side notes-they’re critical factors. Laser treatment works best when paired with:- Regular blood sugar monitoring
- Medications to manage blood pressure and cholesterol
- Quitting smoking
- Annual eye exams-even if you feel fine
Some patients now get anti-VEGF injections instead of-or alongside-laser. These drugs block the signal that triggers abnormal blood vessel growth. They’re often used for macular edema and can improve vision, not just stop it from getting worse. But they require repeated injections, usually every few months. Laser still holds its place, especially for proliferative disease, because it’s long-lasting and doesn’t need ongoing visits.
What Happens If You Don’t Treat It?
Left unchecked, diabetic retinopathy doesn’t just blur your vision. It steals it. Vitreous hemorrhage can cause sudden, painless vision loss. Retinal detachment can lead to permanent blindness if not fixed within days. Neovascular glaucoma-where new vessels block fluid drainage-can raise eye pressure so high it damages the optic nerve. All of this can happen silently, without pain. Once photoreceptor cells die from lack of oxygen, they’re gone forever. No treatment can bring them back. That’s why timing is everything. Early detection + early treatment = preserved vision. Delay = irreversible loss.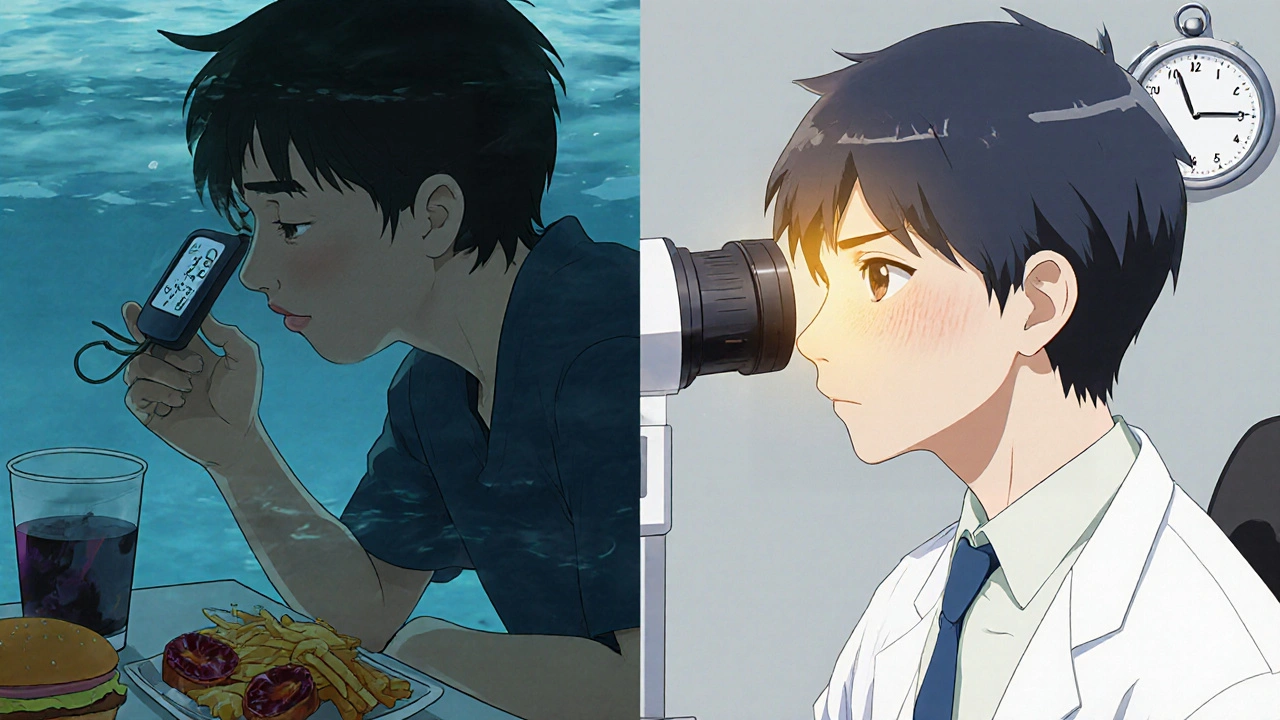
Screening: Your Lifeline
The NHS and other major health bodies recommend a dilated eye exam at least once a year for everyone with diabetes. If you already have retinopathy, you might need them every 3 to 6 months. These aren’t just quick checks. A dilated exam lets the doctor see the back of your eye clearly. They’ll look for microaneurysms, bleeding, swelling, or new blood vessels. Some clinics now use AI-powered retinal imaging-you sit in front of a camera, it takes a picture, and an algorithm flags any signs of damage. It’s fast, accurate, and becoming more common. Don’t skip these. Even if your diabetes feels “mild,” even if you’re young, even if you think you’re doing everything right-get screened. Your eyes don’t lie.Final Reality Check
Diabetic retinopathy isn’t a punishment. It’s a consequence. And like most consequences of uncontrolled diabetes, it’s preventable. You can’t undo years of high blood sugar. But you can stop it from getting worse. Laser treatment isn’t a cure, but it’s a shield. Regular screenings aren’t a chore-they’re your lifeline. Managing your diabetes isn’t optional-it’s your best tool for keeping your sight. The numbers don’t lie: 1 in 3 people with diabetes will face this. But 95% of those who get timely care will keep their vision. That’s not luck. That’s action.Frequently Asked Questions
Can diabetic retinopathy be reversed?
No, once retinal cells die or scar tissue forms, the damage is permanent. But early treatment can stop it from getting worse and preserve remaining vision. That’s why catching it early is so critical.
Does laser treatment hurt?
Most people feel only mild discomfort-like a quick pinch or bright flash. Numbing drops are used, and the procedure takes less than 30 minutes. Some temporary blurriness or light sensitivity afterward is normal, but serious pain is rare.
How often should I get my eyes checked if I have diabetes?
At least once a year. If you already have signs of retinopathy, your eye doctor may recommend checks every 3 to 6 months. Even if your vision seems fine, skipping these exams puts your sight at risk.
Can I still drive if I have diabetic retinopathy?
It depends on the severity. In early stages, most people can drive safely. As peripheral vision or central vision declines, driving-especially at night-becomes risky. Your eye doctor can assess your vision and advise whether it’s safe. In the UK, you’re legally required to inform the DVLA if your vision changes due to a medical condition.
Are there alternatives to laser treatment?
Yes. Anti-VEGF injections (like ranibizumab or aflibercept) are now commonly used, especially for diabetic macular edema. They can improve vision and reduce swelling. Steroid implants are another option. But laser remains a key tool, especially for proliferative retinopathy, because it’s long-lasting and doesn’t require repeated treatments.
Does controlling my blood sugar really make a difference?
Absolutely. Research shows keeping your HbA1c below 7% reduces the risk of retinopathy progression by up to 76%. Every improvement in blood sugar control helps-even small, consistent changes. It’s the single most effective way to protect your eyes.





Mark Kahn
November 21, 2025 AT 02:21Just had my annual eye scan last week - no signs of retinopathy yet, but I’m so glad I went. My doc said my HbA1c’s at 6.8 and that’s why. Small wins, folks. Keep checking, keep managing. You’re not just protecting your eyes - you’re protecting your future self.
Leo Tamisch
November 22, 2025 AT 23:24How quaint. We’ve known for decades that hyperglycemia induces vascular endothelial dysfunction via AGE accumulation and oxidative stress - yet we still treat this like a moral failing rather than a biochemical inevitability. Laser photocoagulation? A palliative bandage on a systemic collapse. The real tragedy isn’t the retinopathy - it’s the healthcare system’s refusal to treat diabetes as a metabolic disorder and instead reduces it to a behavioral checklist.
Daisy L
November 23, 2025 AT 18:2395% chance of keeping your vision if you DO THE WORK?!?!?!!? That’s not luck - that’s discipline!!! And if you’re skipping eye exams because ‘you feel fine’ - honey, you’re one blurry morning away from never seeing your grandkids’ faces again!!!
Anne Nylander
November 24, 2025 AT 10:56my doctor told me to get my eyes checked every year and i kept putting it off… i thought i was fine. then i saw a dark spot and panicked. turned out it was just early swelling. laser fixed it. no big deal. but if i’d waited? who knows. don’t be like me. just go. seriously. your eyes will thank you 😊
Franck Emma
November 25, 2025 AT 05:02I lost my vision in one eye. No warning. No pain. Just… gone. Don’t wait. Get screened. Now.
Noah Fitzsimmons
November 25, 2025 AT 08:03Wow. So let me get this straight - you’re telling me if I just stop eating carbs and staring at my phone, I won’t go blind? What’s next? Brushing my teeth prevents cancer? This is why people think medicine is a cult. Laser treatment is just a profit machine for ophthalmologists anyway.
Eliza Oakes
November 26, 2025 AT 18:55Actually, I read a study - not this one, a real one - that said laser treatment is outdated. Anti-VEGF injections are way better. And also, aren’t you ignoring the fact that most people with diabetes are low-income and can’t afford annual eye exams? This whole post is just privileged wellness propaganda.
Clifford Temple
November 27, 2025 AT 00:33America’s healthcare system is failing us. You think this is about personal responsibility? No. It’s about insurance companies denying coverage for screenings. It’s about pharmacies hiking insulin prices. Stop blaming the patient. Fix the system. Or are you too busy scrolling memes to care?
Corra Hathaway
November 28, 2025 AT 06:16Okay, real talk - I used to hate checking my sugar. Then I lost my uncle to this. He didn’t believe in eye exams. Now I do them religiously. And yes, laser sucks. But it’s better than darkness. So go. Get it done. You’re stronger than your fear. 💪👁️❤️