Can You Get Pregnant While Taking Immunosuppressants?
Many people assume that if you’re on immunosuppressants - whether for lupus, rheumatoid arthritis, or a transplanted organ - pregnancy is off the table. That’s not true anymore. Thanks to better science and smarter drug choices, people on these medications are having healthy babies. But it’s not as simple as just stopping the pills and trying. The wrong drug at the wrong time can harm fertility, increase miscarriage risk, or lead to birth defects. This isn’t about fear. It’s about planning.
Which Immunosuppressants Are Safe During Pregnancy?
Not all immunosuppressants are created equal when it comes to fertility and pregnancy. Some are relatively safe. Others are dangerous. The key is knowing which is which.
Azathioprine is one of the safest options. Over 1,200 pregnancies in women taking this drug showed no increase in birth defects or miscarriage rates. It’s often the go-to choice for people who need to stay on immunosuppressants during pregnancy. Transplant centers and rheumatologists routinely recommend it for those planning to conceive.
Corticosteroids like prednisone can be continued during pregnancy, but they’re not harmless. They can disrupt ovulation and sperm production. They also raise the risk of premature rupture of membranes by 15-20%. Still, stopping them suddenly can trigger a flare-up of autoimmune disease - which is far riskier than the medication itself. The trick is using the lowest effective dose.
Belatacept is newer. Only a handful of pregnancies have been reported so far - three, to be exact - and all resulted in healthy babies. It’s promising, but not yet a standard recommendation. More data is needed.
Which Immunosuppressants Should You Avoid Before and During Pregnancy?
Some drugs are outright dangerous. These aren’t just ‘use with caution’ - they’re stop-now-or-delay-pregnancy drugs.
Methotrexate is a known embryotoxin. It causes severe birth defects. You must stop it at least three months before trying to conceive. Even a single dose after conception can be harmful. Many clinics require a negative pregnancy test before restarting it.
Cyclophosphamide is brutal on fertility. In women, it can cause permanent ovarian damage, especially with cumulative doses over 7g/m². About 60-70% of women who take it long-term lose their ability to conceive naturally. In men, it can cause irreversible azoospermia (no sperm) in up to 40% of cases. If you’re on this drug and want kids, talk to your doctor about egg or sperm freezing before starting treatment.
Chlorambucil is a high-risk drug. It’s linked to serious birth defects: missing kidneys (8% of cases), malformed ureters (12%), and heart problems (15%). It also blocks breastfeeding. If you’re on this, pregnancy should be avoided unless there’s no other option.
Sirolimus has a scary track record. Early reports showed a 43% miscarriage rate - more than double the normal rate. There were also cases of structural birth defects. It’s still listed as contraindicated in pregnancy. Even animal studies don’t fully reassure experts.
Sulfasalazine affects men more than women. It cuts sperm count by 50-60%. The good news? It’s reversible. Sperm counts bounce back within three months after stopping. But if you’re trying to conceive, you’ll need to time it right.
Men, Your Fertility Matters Too
Most people think fertility is a woman’s issue. But men on immunosuppressants need counseling too. The FDA and EMA didn’t require male fertility testing for decades. That means many older drugs were approved without knowing how they affected sperm.
Sulfasalazine, cyclophosphamide, and methotrexate all impact male fertility. Sulfasalazine causes temporary low sperm count. Cyclophosphamide can wipe it out permanently. Methotrexate can reduce sperm quality and increase miscarriage risk if conception happens while the man is taking it.
The FDA recommends semen analysis at three key points: before starting the drug, after one full spermatogenic cycle (about 74 days), and 13 weeks after stopping. If you’re planning a family, ask your doctor for this testing. Don’t assume you’re fine just because you feel healthy.
When Should You Start Planning?
Don’t wait until you miss a period. Start talking to your doctor at least six months before you want to conceive. That’s not too early - it’s essential.
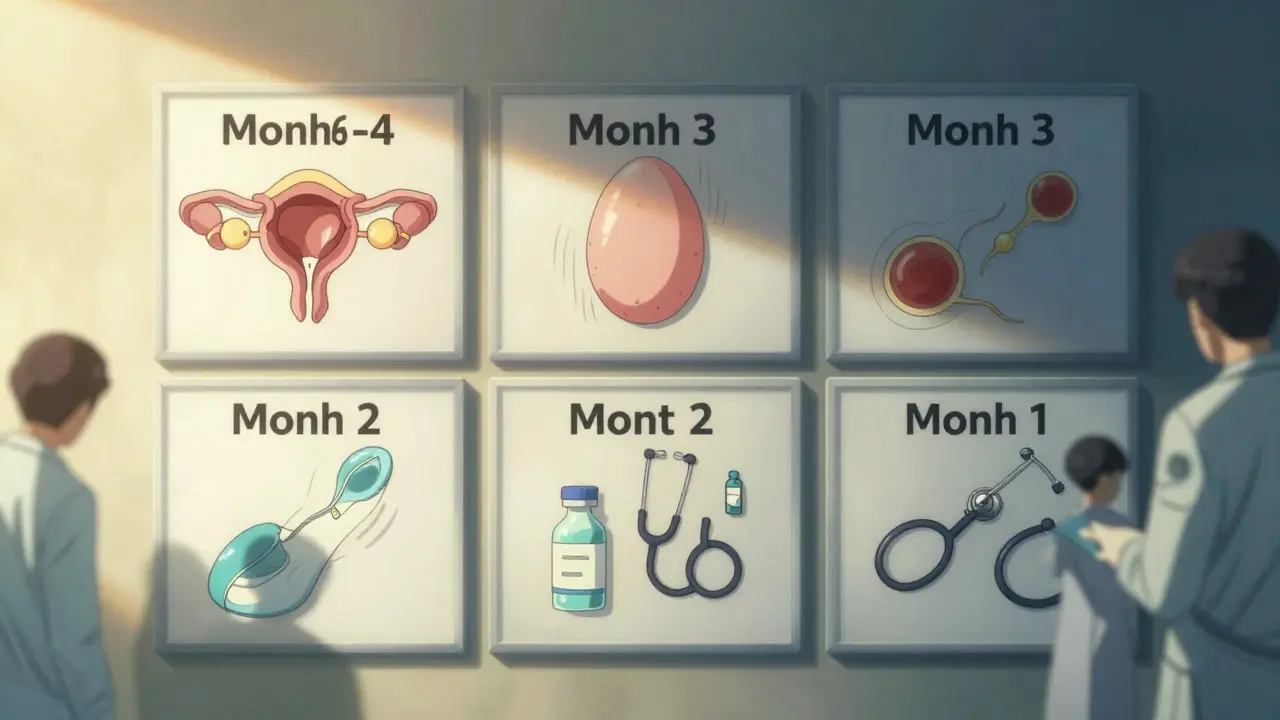
Here’s what that timeline looks like:
- Months 6-4: Review all current medications. Switch from risky drugs like methotrexate or cyclophosphamide to safer ones like azathioprine. This takes time - your body needs to clear the old drug and adjust to the new one.
- Month 3: If you’re a woman on cyclophosphamide, consider fertility preservation (egg freezing). If you’re a man on sulfasalazine, get a semen analysis. Stop methotrexate now.
- Month 2: Get baseline blood work. Check kidney function (creatinine levels). High creatinine before pregnancy raises your risk of preeclampsia. If your level is above 13 mg/L, your doctor may delay pregnancy until it’s under control.
- Month 1: Confirm you’re off all unsafe drugs. Start prenatal vitamins with folic acid. Schedule a preconception visit with your rheumatologist, transplant team, and OB-GYN.
This isn’t just about getting pregnant. It’s about staying healthy during pregnancy. Flares of lupus or rejection of a transplanted kidney are far more dangerous to mother and baby than the right dose of azathioprine.
What Happens After the Baby Is Born?
Medication doesn’t end at delivery. Many people worry about breastfeeding while on immunosuppressants.
Azathioprine is considered safe for breastfeeding. Only tiny amounts pass into milk, and studies show no harm to infants.
Chlorambucil and cyclophosphamide are not safe. They can damage the baby’s immune system through breast milk.
Prednisone is okay in low doses. Take it right after feeding to minimize exposure.
Also, babies exposed to immunosuppressants in the womb may have lower B-cell and T-cell counts. That means they’re more vulnerable to infections in the first year. Your pediatrician should monitor them closely. Vaccinations may need to be delayed or adjusted.
Why Is Preconception Counseling So Important?
Back in 2000, doctors had almost no data on children born to parents on immunosuppressants. Today, we know more - but gaps remain. Newer drugs like belatacept have only been used in a few pregnancies. Long-term effects on children’s immune systems, growth, and brain development are still unknown.
That’s why counseling isn’t optional. It’s a team effort. Your rheumatologist, transplant specialist, fertility expert, and OB-GYN need to be on the same page. One missed detail - like not switching from methotrexate in time - can change everything.
And here’s the truth: the risk of your disease flaring up if you stop your meds is 2-5%. That’s higher than the risk of birth defects from azathioprine. The goal isn’t to stop treatment. It’s to switch to the safest option at the right time.
What’s Changing in the Field?
The rules are getting stricter - and that’s good. New drugs now require FDA and EMA approval based on studies involving at least 200 men, testing sperm count and quality before and after exposure. That didn’t happen 20 years ago.
Transplant centers are also standardizing care. Eighty-five percent now have written protocols for pregnancy management. That’s a huge leap from the days when every case was a guessing game.
But we still need more research. Registries tracking outcomes for babies exposed to newer drugs like belatacept or sirolimus are urgently needed. We need long-term studies on whether these children develop normally - physically, mentally, and immunologically.
For now, the message is clear: You can have a baby while on immunosuppressants - but only if you plan ahead, switch drugs wisely, and work with a team that knows the science.
What If You’re Not Ready for Pregnancy Yet?
If you’re not planning a family now but might want kids later, don’t wait until it’s too late. Talk to your doctor about fertility preservation - egg freezing, sperm banking, or even ovarian suppression with hormone therapy if you’re on cyclophosphamide.
It’s not just about saving cells. It’s about saving options. Many people assume they’ll have time. But some drugs cause damage fast. Once the eggs or sperm are gone, they’re gone for good.
And if you’re already on a high-risk drug? Don’t panic. But do act. Ask your doctor: ‘What’s my risk of infertility? What can we do now to protect my future fertility?’
Can I get pregnant while taking azathioprine?
Yes. Azathioprine is one of the safest immunosuppressants for pregnancy. Over 1,200 pregnancies have been studied, and no increase in birth defects or miscarriage rates has been found. It’s often the preferred choice for women who need to stay on immunosuppressants while trying to conceive or during pregnancy.
How long before pregnancy should I stop methotrexate?
You must stop methotrexate at least three months before trying to conceive. It’s a powerful drug that can cause severe birth defects even in early pregnancy. Waiting three months gives your body time to clear it completely. Some doctors recommend a blood test to confirm levels are undetectable before stopping contraception.
Does cyclophosphamide cause permanent infertility?
It can. In women, cumulative doses over 7g/m² cause permanent ovarian damage in 60-70% of cases. In men, it leads to irreversible azoospermia in about 40%. If you’re on this drug and want children, consider egg or sperm freezing before starting treatment. Once the damage is done, it can’t be reversed.
Is it safe to breastfeed while on immunosuppressants?
It depends on the drug. Azathioprine is considered safe in low to moderate doses. Prednisone is okay if taken right after feeding. But chlorambucil, cyclophosphamide, and methotrexate are not safe - they can pass harmful amounts into breast milk. Always check with your doctor before breastfeeding.
Should men on immunosuppressants get a semen analysis?
Yes. Many immunosuppressants affect sperm count and quality, but this isn’t always obvious. The FDA recommends semen analysis before starting the drug, after one spermatogenic cycle (74 days), and 13 weeks after stopping. This helps determine if fertility is affected and when it might return.
What’s the biggest mistake people make when planning pregnancy on immunosuppressants?
Waiting too long to talk to a doctor. Many people assume they can just stop the meds and try right away. But switching drugs takes months. Stopping dangerous ones like methotrexate requires a three-month buffer. Delaying counseling can cost you your chance to conceive safely - or worse, lead to a high-risk pregnancy.








Brittany Fiddes
January 27, 2026 AT 18:58And don’t get me started on the ‘preconception counseling’ nonsense. If you need a six-month plan to have a baby, maybe you shouldn’t be having one at all. Nature didn’t invent spreadsheets.
Amber Daugs
January 28, 2026 AT 21:18Ambrose Curtis
January 28, 2026 AT 22:51And guys? Get your sperm tested. Seriously. You think you’re fine because you ‘feel good’? Nope. Sperm takes 74 days to regenerate. If you’re on sulfasalazine and didn’t test, you’re just winging it. And that’s not love. That’s luck.
Phil Davis
January 30, 2026 AT 14:18Also, ‘three months’ before stopping methotrexate? That’s not science. That’s guesswork with a lab coat. And yet we’re supposed to treat this like gospel? I’ll stick with my gut and my Google.
Irebami Soyinka
January 31, 2026 AT 02:25God didn’t design women to be pharmaceutical test subjects. 🙏
Linda O'neil
February 1, 2026 AT 02:46If you’re scared, talk to someone who’s been there. Not some random Reddit commenter. Real people. Real results. You got this.
Robert Cardoso
February 2, 2026 AT 06:47And let’s not pretend cyclophosphamide’s 60% infertility rate is ‘manageable.’ That’s not a side effect-that’s a war crime against future generations. We’re treating fertility like an optional feature on a car. It’s not. It’s biological infrastructure.
James Dwyer
February 3, 2026 AT 23:06jonathan soba
February 4, 2026 AT 06:27Also, ‘lowest effective dose’ of prednisone? How is that defined? By whom? And why is no one asking if the mother’s mental health matters? Stress kills more babies than drugs.
Chris Urdilas
February 5, 2026 AT 05:30Men, this isn’t just your partner’s problem. It’s yours. Get tested. Don’t wait. Don’t assume. Don’t be the guy who blames his wife for ‘failing’ to conceive when he’s been on a drug that turns sperm into confetti.
Jeffrey Carroll
February 6, 2026 AT 16:07