Nocturnal Acid Breakthrough Symptom Checker
This tool helps determine if you might have nocturnal acid breakthrough, which is the only situation where combination therapy with H2 blockers and PPIs might be appropriate. Based on your symptoms, it will provide personalized recommendations.
Many people take acid-suppressing meds without realizing they might be doubling up-sometimes unnecessarily. If you’re on both an H2 blocker and a proton pump inhibitor (PPI), you’re not alone. About 15-20% of hospitalized patients get both. But here’s the catch: for most people, this combo doesn’t work better. It just adds risk.
How H2 Blockers and PPIs Work (and Why They’re Not the Same)
H2 blockers like famotidine (Pepcid) and cimetidine (Tagamet) cut stomach acid by blocking histamine from telling acid-producing cells to turn on. They kick in fast-within an hour-and last about 6 to 12 hours. That’s why some people take them at night if they get heartburn after dinner.
PPIs like omeprazole (Prilosec) or esomeprazole (Nexium) work differently. They shut down the actual acid pumps in the stomach lining. But they don’t work right away. It takes 2 to 5 days to reach full power. Once they do, they suppress acid by 90-98%, nearly all day long.
So why do doctors sometimes prescribe both? The idea was simple: if one blocks histamine and the other shuts down pumps, maybe together they’d be stronger. But reality doesn’t match the theory.
The Problem: PPIs Make H2 Blockers Less Effective
H2 blockers need some acid activity to work. They rely on histamine signals to be present. But PPIs turn those signals off so completely that there’s almost nothing left for H2 blockers to block. Think of it like turning off the water main-then asking someone to shut off individual faucets. The faucets don’t matter anymore.
A 2022 study in the Journal of Clinical Gastroenterology looked at patients on omeprazole who added ranitidine (an H2 blocker). The result? Only a 5% extra drop in acid over 24 hours. That’s barely noticeable. And it didn’t help daytime symptoms at all. There was a tiny dip in nighttime acid, but even that wasn’t enough to improve how people felt.
The American College of Gastroenterology reviewed 12 studies with nearly 3,000 patients. Their 2022 guideline says it clearly: “Long-term combination therapy offers no additional benefit for GERD.”
The Hidden Risks: Why This Combo Can Hurt More Than Help
Using two acid-suppressing drugs isn’t just redundant-it’s risky.
A 2014 study of nearly 80,000 ICU patients found that those on PPIs had a 30% higher chance of getting hospital-acquired pneumonia than those on H2 blockers. They also had a 32% higher risk of Clostridium difficile infection-a nasty, hard-to-treat gut bug that causes severe diarrhea.
Even more surprising? PPIs were linked to a 22% higher risk of gastrointestinal bleeding than H2 blockers. That’s the opposite of what you’d expect. PPIs are often used to prevent bleeding in sick patients, but the data shows they might not be safer-and could even be riskier.
For people with kidney problems, the danger grows. A 2021 study of over 3,600 patients with chronic kidney disease found that those on PPIs were 28% more likely to progress to kidney failure than those on H2 blockers. That’s not a small difference. It’s a real, measurable threat.
And it’s not just infections or kidneys. Long-term PPI use is tied to lower levels of vitamin B12, magnesium, and calcium. That’s because stomach acid helps break down nutrients. Less acid means less absorption. Many patients don’t realize their fatigue, muscle cramps, or tingling fingers might be from a medication they’ve been taking for years.
Who Actually Benefits from This Combo?
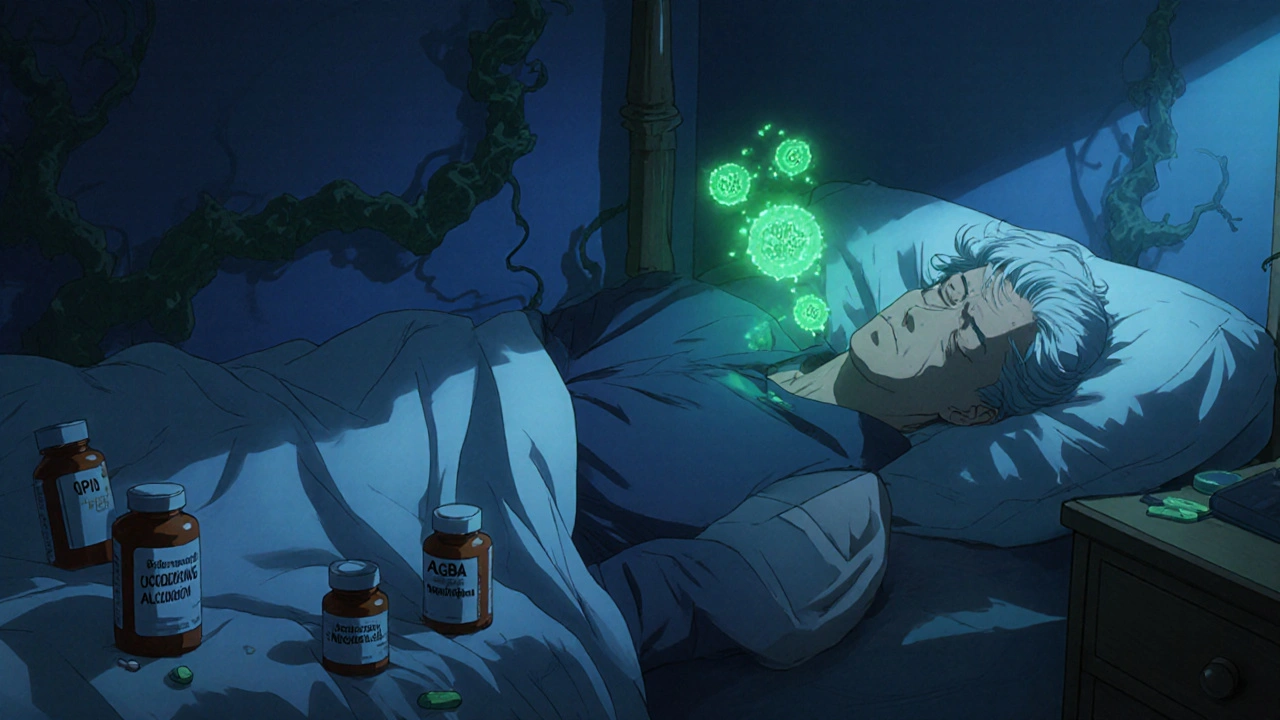
There’s one group where this combo might still make sense: people with nocturnal acid breakthrough.
This means their stomach acid rises too high between midnight and 6 a.m., even while on a full dose of PPI. Symptoms include waking up with heartburn, a sour taste, or coughing. It’s rare. And it’s hard to diagnose without a 24-hour pH test that measures acid levels overnight.
If that test shows acid levels below pH 4 for more than an hour during the night, adding an H2 blocker at bedtime might help. But even then, it’s temporary. The guidelines say to try it for 4 to 8 weeks. If symptoms don’t improve, stop the H2 blocker. Don’t keep it going.
Most people don’t need this test. Most people don’t have nocturnal breakthrough. And most people are taking both drugs because their doctor always did it-or they saw it online.
Why Is This Combo So Common If It’s Not Recommended?
It’s a mix of habit, fear, and misinformation.
Doctors used to think PPIs were the gold standard. H2 blockers were seen as old-school. So when a patient didn’t feel better right away, adding another drug felt like doing more. But more isn’t better here.
Pharmaceutical marketing played a role too. PPIs became billion-dollar drugs. H2 blockers like famotidine are cheap and generic. There’s little incentive to promote them.
Patients don’t always know why they’re on both. A 2022 survey by the American College of Gastroenterology found that 31% of people on combo therapy couldn’t explain why they were taking both. Sixty-four percent didn’t know the possible side effects.
And then there’s the internet. Reddit threads in r/GERD show that 42% of long-term PPI users say they can’t stop because they get rebound heartburn. That’s not addiction-it’s physiology. When you shut down acid for months, your stomach overcompensates. Stop the PPI too fast, and acid surges back. That’s why people think they need it forever.

What Should You Do If You’re on Both?
Don’t stop suddenly. But do ask questions.
- Ask your doctor: “Why am I on both? Is there proof I need this?”
- Ask: “Could I try stopping the H2 blocker first?”
- Ask: “Has my need for acid suppression been rechecked in the last 3 months?”
The Department of Veterans Affairs recommends a “PPI time-out” every 90 days. That means pausing the drug to see if you still need it. If you’re not having symptoms, you might not.
If you’ve been on a PPI for over a year, talk to your doctor about tapering. Don’t quit cold turkey. Reduce the dose slowly. Switch to taking it every other day. Try an H2 blocker at night instead. Many people find relief this way.
And if you’re taking famotidine (not cimetidine), you’re probably safe from major drug interactions. Cimetidine can interfere with how other meds are broken down by the liver. But famotidine? Almost no effect. So if you’re on other pills-like blood thinners or antidepressants-stick with famotidine if you need an H2 blocker.
The Bigger Picture: Less Is Often More
The U.S. spends $12.3 billion a year on acid-suppressing drugs. PPIs make up 78% of those prescriptions. Yet studies show that up to 70% of PPI prescriptions are unnecessary.
Adding an H2 blocker to an unnecessary PPI doesn’t fix the problem. It makes it worse.
The American Gastroenterological Association now lists “Don’t prescribe combination therapy for routine GERD” as one of its top Choosing Wisely recommendations. Medicare is starting to penalize hospitals that overuse this combo. That’s a big shift.
There’s new research looking at genetic markers that might predict who truly benefits from dual therapy. But for now, the answer is simple: if you don’t have documented nighttime acid breakthrough, you probably don’t need both.
Stomach acid isn’t your enemy. It’s your digestive partner. Too little can cause more problems than too much.
What to Do Next
Write down your symptoms. When do they happen? After meals? At night? Do you wake up with a sour taste? Are you taking your meds exactly as prescribed?
Bring this list to your next appointment. Ask if you can try going off the H2 blocker for a few weeks. Monitor how you feel. If your symptoms stay gone, you might not need it at all.
If you’ve been on a PPI for years, ask about a taper plan. Don’t assume you need it forever. Most people don’t.
And if your doctor says, “It’s fine to keep both”-ask why. Demand evidence. Not tradition. Not habit. Not fear.






Solomon Ahonsi
February 2, 2026 AT 23:29So let me get this straight-we’re spending billions on drugs that don’t work better together and might actually kill you slowly? And doctors still prescribe this like it’s a fucking buffet? I’ve been on both for three years and just realized I’m basically a lab rat for Big Pharma. Thanks, medicine.
George Firican
February 4, 2026 AT 09:50The irony here is almost poetic-our entire medical infrastructure is built on the assumption that more intervention equals better outcomes, when in reality, biology thrives on balance, not suppression. Stomach acid isn’t an enemy to be eradicated; it’s a gatekeeper, a catalyst, a silent guardian of digestion and immunity. To silence it indiscriminately is to dismantle a system we barely understand, then wonder why we’re fatigued, deficient, and prone to infection. We’ve turned physiology into a problem to be solved with pills, not a process to be respected.
Matt W
February 5, 2026 AT 19:23I had no idea this combo was so risky. I’ve been on omeprazole for years and added famotidine when my heartburn got worse at night. I thought I was being proactive. Turns out I was just stacking risks. Going to talk to my doc about dropping the H2 blocker first. Thanks for the wake-up call.
Anthony Massirman
February 6, 2026 AT 21:41Just stop the H2 blocker. You’ll be fine.
Brittany Marioni
February 8, 2026 AT 03:31Wow. This is so important. Seriously. I can’t believe how many people are on this combo without even knowing why. I’ve seen patients on both drugs for over a decade-and they’re all tired, all low on magnesium, all confused. We need to stop treating symptoms and start treating the root cause. And yes, please, everyone: ask your doctor for a PPI time-out. Every 90 days. Please.
phara don
February 8, 2026 AT 10:58So if PPIs cause more bleeding than H2 blockers… why are they still the go-to for ICU patients? 🤔
Bob Hynes
February 9, 2026 AT 05:23bro i just found out my doc gave me both because he "always does it"... i thought it was some advanced science thing. turns out its just medical muscle memory. like wearing socks with sandals. it works? maybe. but why??
Eli Kiseop
February 10, 2026 AT 17:48So the study says adding H2 to PPI only gives 5% more acid reduction and no symptom improvement but we still do it because doctors are lazy and pharma pushes PPIs? Makes sense. Guess I’m quitting my meds and eating celery instead
Chinmoy Kumar
February 12, 2026 AT 02:17This is eye-opening. I’m from India and here too, doctors prescribe PPIs like candy. I’ve seen people take them for years without review. I’ll share this with my family. Also, famotidine is cheap here, so maybe switching to just that if needed? Thanks for the clarity.
Bridget Molokomme
February 13, 2026 AT 07:16Oh so the reason my stomach feels like it’s staging a rebellion after I tried to quit PPIs is because my body went full drama queen and overproduced acid? Not addiction. Just biology being dramatic. Cool. So now I’m supposed to taper? Like a recovering addict? Guess I’m joining the club.
Ansley Mayson
February 14, 2026 AT 07:00Typical. Americans pay $12 billion for drugs they don’t need while other countries use generics and live longer. Of course the system’s broken. We’re too busy buying pills to fix our diets. Stop eating pizza at midnight and maybe you won’t need this crap.
Murarikar Satishwar
February 14, 2026 AT 15:22This is one of the clearest summaries I’ve read on acid suppression. The science is solid, the risks are real, and the cultural inertia is terrifying. I’ve seen patients on dual therapy for over 10 years, and not one had a documented indication. The real tragedy? They all believe they need it. Knowledge is power-but only if it’s shared. Thank you for this.
Dan Pearson
February 15, 2026 AT 06:19Ohhhhh so THAT’S why I can’t stop my PPI?! I thought I was addicted to Prilosec like it was a drug-which, honestly, I kinda was. But now I get it-it’s not addiction, it’s my stomach throwing a tantrum because I shut down its acid factory for too long. I’m gonna taper slow, try famotidine at night, and blame Big Pharma for my 3am heartburn. Thanks, doc… I guess.