Every year, thousands of people in the U.S. end up in the hospital-not because their condition got worse, but because someone didn’t know what medications they were taking. It’s not rare. It’s not unusual. It’s medication list errors. And the fix? Simple. But only if you do it right.
Why Your Medication List Matters More Than You Think
Think about the last time you saw a doctor. Did you tell them about that ibuprofen you take for your knees? What about the magnesium you started last month? Or the ginkgo biloba your sister swore helped her memory? If you didn’t mention it, you’re not alone. Most people leave out over-the-counter drugs, vitamins, or supplements because they don’t think they count. They’re wrong. A 2021 study found that more than half of patient-reported medication lists had at least one critical error. That means doctors were making decisions based on incomplete or wrong info. One wrong dose of blood thinner, one missed allergy, one unreported herb-and you could end up in the ER. The FDA says medication errors cause about 7,000 deaths a year. Many of those are preventable. The solution isn’t fancy tech or expensive apps. It’s a clear, updated list. Not just a note on your phone. Not just a scribble on a napkin. A real, complete, verified list that you carry with you-and update every time something changes.What to Include on Your Medication List
A good medication list isn’t just a drug name. It’s a full picture. Here’s exactly what you need to write down for every medication:- Drug name-both brand and generic (e.g., Lisinopril, also sold as Zestril)
- Strength and dose-like 10 mg, 2 tablets, or 5 mL
- How often-once daily, twice a week, as needed
- How to take it-by mouth, with food, under the tongue, injected
- Why you take it-for high blood pressure, for sleep, for joint pain
- When you last took it-especially important if you take something ‘as needed’
- Who prescribed it-your doctor’s name or clinic
- Allergies and reactions-not just ‘penicillin allergy,’ but ‘rash, swelling, trouble breathing’
Choose Your Format: Paper, App, or EHR
You’ve got options. Each has pros and cons.Paper lists-like the FDA’s free My Medicines template-are simple, reliable, and work even if your phone dies. You can print one, carry it in your wallet, and hand it to any provider. But here’s the catch: 43% of paper lists are outdated within three months. If you don’t update it after every doctor visit or pharmacy refill, it’s useless.
Smartphone apps like Medisafe, MyTherapy, or CareZone help you track doses, set reminders, and even alert you about interactions. One study found they reduce missed doses by 28%. But only 35% of people over 65 use them regularly. If you’re not tech-savvy, they can feel overwhelming. Some apps have clunky interfaces. And if you lose your phone? You lose your list.
EHR-integrated lists-like those in Epic’s MyChart or Apple Health-are powerful. They sync with your doctor’s records and can auto-update when prescriptions are filled. But you can’t access them if you’re not at the hospital or if your provider doesn’t use the same system. And if your doctor doesn’t update it, the list stays wrong.
The best approach? Use both. Keep a printed copy in your wallet. Use an app for reminders. And make sure your doctor has access to the most current version during every visit.
How to Keep It Updated (Without Forgetting)
The biggest reason medication lists fail? People forget to update them.A 2021 University of Michigan study found that 68% of patients didn’t update their list after leaving the hospital. That’s terrifying. You come home with a new blood pressure pill, stop an old one, and never tell anyone. Then you see your primary care doctor a month later-and they prescribe something that clashes with your new med.
Here’s how to make updating easy:
- Set a monthly reminder-every first Sunday, spend 10 minutes checking your meds. Use your phone calendar.
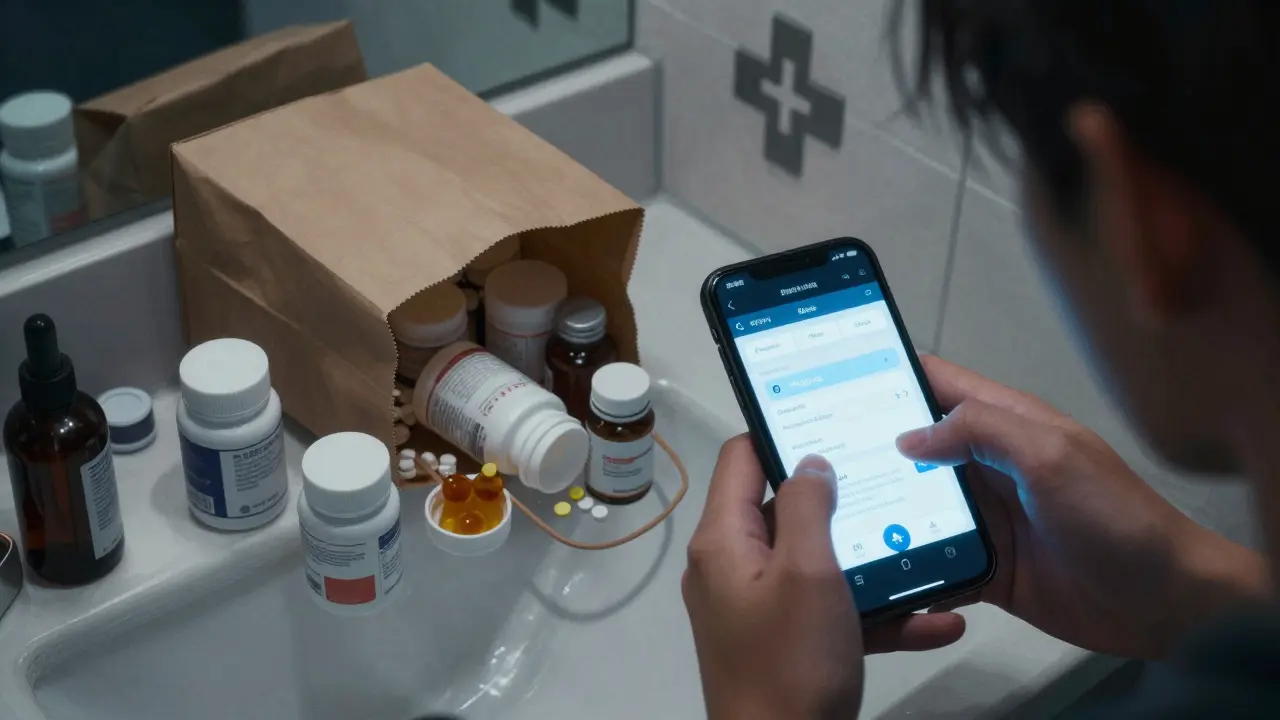
- Use the brown bag method-once a month, dump all your pills, vitamins, and supplements into a bag. Take it to your doctor or pharmacist. They’ll sort it out. No guessing.
- Take a photo of each pill bottle-especially if you have trouble reading small print. Store them in a folder on your phone labeled “My Meds.”
- Update after every change-new prescription? Cross out the old one. Stopped a drug? Write “Discontinued: 12/15/2025.”
- Sync refills-ask your doctor to prescribe 90-day supplies for chronic meds. That means fewer trips to the pharmacy and fewer chances to forget changes.
One patient I know started taking a photo of her pill bottles every Sunday. She didn’t use an app. She didn’t even write anything down. But when she had a fall and ended up in the ER, the nurse pulled up her photos on her phone-and caught a dangerous interaction between her blood thinner and a new painkiller. She was lucky. You can be too.
How to Use Your List in Real Situations
Your list only works if you use it when it matters.- At every doctor’s appointment-hand it to the nurse or doctor before they leave the room. Say: “Here’s my current list. Did anything change?”
- At the pharmacy-when you pick up a new prescription, ask the pharmacist: “Does this interact with anything on my list?” They’re trained to catch this.
- In the ER-keep a copy in your purse, backpack, or car. If you can’t talk, someone else can hand it to staff.
- When you’re admitted to the hospital-don’t wait for them to ask. Bring your list. Say: “This is what I’m taking. Please check it against your records.”
Hospitals are required to reconcile your meds during every transition-admission, transfer, discharge. But they won’t do it well unless you help. Your list is your voice when you’re too sick to speak.

Common Mistakes (And How to Avoid Them)
Even people who try to keep lists make the same errors:- Only listing prescriptions-OTC meds, vitamins, and herbs matter just as much.
- Writing “as needed” without specifics-“Take ibuprofen for pain” isn’t enough. Write “800 mg every 8 hours as needed for joint pain, max 3 per day.”
- Not including discontinued drugs-if you stopped a med, write “Discontinued: [date]” so no one prescribes it again.
- Using abbreviations-“BID” or “QD” can be misread. Write “twice daily” or “once daily.”
- Keeping it in one place-if it’s only on your phone, you’re vulnerable. Print a copy. Keep one in your car. Give one to a family member.
And never assume your doctor knows what you’re taking. A 2022 study showed that 56% of patient-reported lists had critical errors-meaning doctors were trusting inaccurate info. Your list is your safety net. Don’t rely on someone else to remember it for you.
Resources to Get Started
You don’t need to build this from scratch. Free tools exist:- FDA’s My Medicines template-downloadable, printable, includes allergies and emergency contacts.
- American Heart Association medication tracking sheets-simple, clear, designed for seniors.
- Medisafe, MyTherapy, CareZone-free apps with refill alerts and interaction warnings.
- Your pharmacist-many offer free Medication Therapy Management (MTM) under Medicare Part D. They’ll review your list, check for interactions, and update your records.
Don’t wait for a crisis. Start today. Spend 20 minutes. Write it down. Take a photo. Print it. Give a copy to someone you trust.
Medication safety isn’t about technology. It’s about responsibility. And the person most responsible? You.
What if I take a lot of medications? How do I keep track?
If you take five or more medications, you’re considered polypharmacy. That’s when mistakes are most dangerous. Use a combination: a printed list you carry, a photo album of all your pill bottles on your phone, and a trusted app like Medisafe for reminders. Ask your pharmacist for a Medication Therapy Management session-they’ll organize everything for you and flag risks. Many Medicare Part D plans cover this for free.
Should I include supplements and vitamins?
Yes, absolutely. Supplements aren’t harmless. St. John’s Wort can make birth control and antidepressants ineffective. Vitamin K can interfere with blood thinners like warfarin. Even common ones like calcium or magnesium can affect how your body absorbs other drugs. List every pill, capsule, powder, or tea you take daily-even if you think it’s “just a natural remedy.”
How often should I update my medication list?
Update it every time you start, stop, or change a medication. That includes prescriptions, OTC drugs, supplements, or even doses. At minimum, review your list every three months. And always bring it to every doctor’s visit, ER trip, or hospital admission. Don’t wait for an annual checkup-changes happen between visits.
Can my doctor update my list for me?
They should-but they often don’t. Most doctors rely on what you tell them. If you don’t bring an updated list, they won’t know what’s changed. Don’t assume they’re tracking it. Take charge. Bring your list. Say, “I’ve updated this. Can you confirm it matches your records?” If they don’t update their system, ask them to write the changes on your copy.
What if I forget my list at an appointment?
If you forget it, call your pharmacy. They have your full prescription history. Ask them to email or fax a copy to your doctor. Or use your phone to show photos of your pill bottles. Even that’s better than nothing. In an emergency, if you can’t speak, a family member or friend can still hand over your list or photos. Keep a copy with someone you trust.
Is a digital list safer than paper?
It depends. Digital lists are great for reminders and interaction alerts, but they fail if your phone dies, you lose it, or you’re not tech-savvy. Paper is always accessible, but it gets outdated. The safest approach is both: use an app for daily reminders, and keep a printed version in your wallet, purse, or car. That way, you’re covered no matter what.
Next Steps: Start Today
You don’t need to wait for a health scare. Right now, do this:- Find all your medications-prescriptions, OTCs, vitamins, herbs.
- Write down the six key details for each (name, dose, frequency, route, reason, prescriber).
- Print a copy using the FDA’s free template.
- Take a photo of each pill bottle and save it in a folder labeled “My Meds.”
- Give a copy to a family member or close friend.
- Bring it to your next appointment-even if you think nothing’s changed.
Medication errors don’t happen because people are careless. They happen because no one thought to write it down. Don’t be the one who forgot. Your life depends on it-not on a doctor’s memory, not on an app’s reminder, but on your action today.






jesse chen
December 27, 2025 AT 18:44I’ve been keeping a paper list in my wallet since my dad had that near-miss with the blood thinner and St. John’s Wort last year. I update it every Sunday after I dump all my pills into a bag and take them to the pharmacist. It’s not glamorous, but it’s saved me twice already.
Don’t wait for an ER visit to start. Just do it.
It’s the one thing no one can take from you.
Alex Ragen
December 29, 2025 AT 09:55How quaint. A paper list? In the age of blockchain-enabled, AI-audited pharmacovigilance ecosystems? You’re clinging to the analog equivalent of a rotary phone while the world moves toward decentralized, interoperable health ledgers synced with your biometrics and micro-dosing AI.
And yet-ironically-the only thing that’s ever prevented a fatal interaction is a human hand writing down ‘warfarin, 5mg, daily’ on a napkin. The tragedy isn’t the list-it’s the epistemological collapse of trust in the self as a reliable data source.
Lori Anne Franklin
December 31, 2025 AT 06:16omg yes!! i started using the photo thing after my mom had that mixup with her thyroid med and the calcium pill-turned out the calcium was blocking absorption!!
i just take pics of every bottle every sunday and throw em in a folder called ‘my meds lol’
it’s not perfect but it’s better than nothing and i feel so much less anxious now 😅
Zina Constantin
December 31, 2025 AT 13:54This is one of those rare pieces of advice that’s not just helpful-it’s life-saving. And yet, it’s so simple, it feels almost insulting to need reminding.
But here we are. Millions of people walking around with polypharmacy bombs in their medicine cabinets, and no one’s taught them how to defuse them.
So let’s change that. Print it. Photograph it. Hand it to your doctor like it’s a sacred text. Because it is.
Your life isn’t a suggestion. It’s a responsibility. And this? This is how you honor it.
Sarah Holmes
January 1, 2026 AT 16:21It’s pathetic. We’ve reduced human health to a checklist. We’ve outsourced our cognitive responsibility to paper and apps, while doctors, pharmacists, and hospitals continue to operate in bureaucratic oblivion. The real problem isn’t the lack of a list-it’s the systemic failure to treat patients as partners. You carry your list, and they still misread your handwriting. You update your app, and their EHR is stuck in 2012. This isn’t safety. It’s performative compliance for people too exhausted to demand better.
Jay Ara
January 2, 2026 AT 15:46bro this is gold. i live in india and my grandma takes like 12 things a day and no one writes anything down. i started making her take pics of each bottle and put them in a google folder. now when we go to the clinic, i just show the phone. she’s so proud of herself now. simple but works.
thank you for this
Michael Bond
January 2, 2026 AT 17:24Just did it. Took 17 minutes. Printed it. Gave a copy to my sister. Took photos of every bottle. Done.
Feels good.
Kuldipsinh Rathod
January 3, 2026 AT 01:15i used to think vitamins were harmless. then my cousin had a stroke because he took ginkgo with his aspirin and no one knew. now i list everything-even the turmeric tea i drink at night. it’s not about being paranoid. it’s about being smart.
SHAKTI BHARDWAJ
January 3, 2026 AT 04:39Oh great. Another guilt-trip disguised as public health advice. So now I’m a bad person because I don’t photograph my melatonin bottle? What about the people who can’t afford printers? Who don’t have smartphones? Who work three jobs and sleep 4 hours? This isn’t empowerment-it’s performative privilege wrapped in a FDA template.
Matthew Ingersoll
January 3, 2026 AT 21:00I’ve been using MyChart for years. My doctor updates it. My pharmacy updates it. My insurance updates it. I don’t need a paper list. I don’t need photos. I don’t need to remember anything. The system works-if you’re in it.
But yeah, if you’re not, you’re screwed.
That’s the real problem.
carissa projo
January 5, 2026 AT 13:50There’s something deeply human about holding a piece of paper with your life written on it in your own handwriting. It’s not just a list-it’s a covenant with yourself. A promise: I will not be invisible in this system. I will not be forgotten. I will not be a statistic.
And when you hand it to your doctor, you’re not just giving them information-you’re giving them permission to see you.
That’s power. That’s dignity.
Don’t underestimate it.
josue robert figueroa salazar
January 5, 2026 AT 20:44Yeah sure. Keep your list. But let’s be real-most doctors glance at it for 3 seconds and then ignore it. Pharmacies? They’ll refill your 10-year-old prescription because the computer says so. This is theater. You’re playing along with a broken system because you think it’ll save you.
It won’t.
But hey, at least you tried.
christian ebongue
January 7, 2026 AT 03:16So you’re telling me I need to take photos of my pills… and update a list… and carry it everywhere…
and I still might get prescribed something that clashes with my fish oil?
Wow. I’m so glad I didn’t go to med school.
Thanks for the reminder that healthcare is just a series of inconvenient chores designed to make you feel responsible for a system that doesn’t care.
…I’ll still do it. Because what else can I do?