When you take a pill once a day instead of three times, it’s not magic-it’s science. Modified-release (MR) formulations are engineered to release medicine slowly over hours, keeping drug levels steady in your blood. That means fewer side effects, better control of chronic conditions, and more convenience. But here’s the catch: just because two pills look the same doesn’t mean they work the same. For generic versions of these drugs to be approved, they must prove bioequivalence-and the rules for MR drugs are far more complex than for regular pills.
Why Modified-Release Drugs Need Special Rules
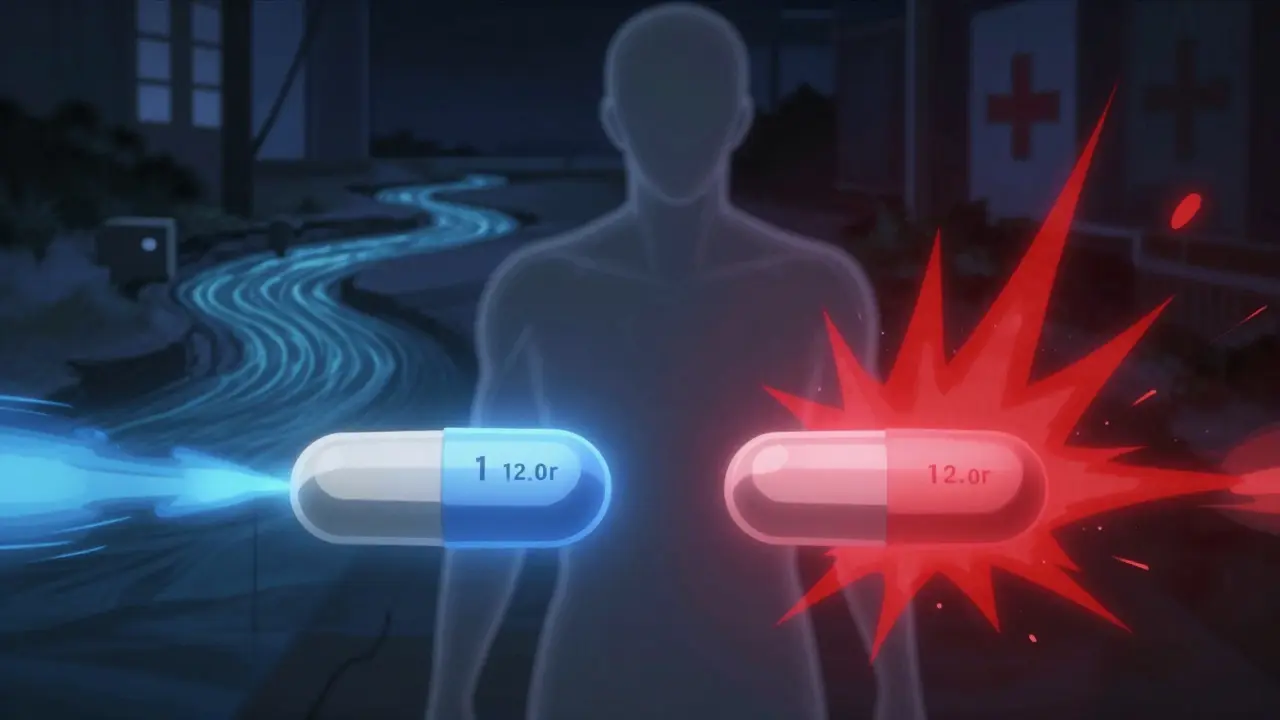
Immediate-release (IR) drugs hit your bloodstream fast and clear. Their bioequivalence is simple: measure how much drug gets into your blood (AUC) and how high the peak level goes (Cmax). If the generic matches the brand within 80-125%, it’s approved. But modified-release drugs? They’re designed to behave differently. An extended-release (ER) tablet might release 30% of its dose in the first hour, then slowly trickle out over the next 12 hours. If a generic releases that 30% too fast, you get a spike-maybe even side effects. Too slow, and you don’t get enough medicine when you need it. That’s why regulators don’t just look at total exposure. They break the curve into pieces. For example, with zolpidem CR (Ambien CR), the FDA requires two separate measurements: one for the first 1.5 hours (the quick-release part), and another for the rest of the time (the slow-release part). Both must fall within the 80-125% range. Miss one, and the whole application gets rejected.The FDA vs. EMA: Two Different Approaches
Not all regulatory agencies see eye to eye. The U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) have different standards, and that creates real headaches for drugmakers trying to launch generics globally. The FDA prefers single-dose studies in fasted patients. They argue that’s the most sensitive way to catch differences in how the drug releases from the tablet. In fact, 92% of ER generics approved since 2015 used this method. They also demand detailed dissolution testing at three pH levels-stomach acid (pH 1.2), small intestine (pH 4.5), and upper gut (pH 6.8). If your tablet dissolves too fast in acid or too slow in neutral pH, it’s a red flag. The EMA, on the other hand, sometimes requires steady-state studies-where patients take the drug daily for weeks until levels stabilize. They argue this better reflects real-world use, especially for drugs that build up in the body. But critics say this adds months to development and isn’t always necessary. In 2023, the EMA proposed aligning more closely with the FDA, possibly dropping the steady-state requirement for most products. And then there’s the WHO, which claims MR bioequivalence rules should be “essentially the same” as for regular drugs. That’s not true in practice. No major regulator treats them that way.Special Cases: Multiphasic, NTI, and Alcohol Risks
Some MR drugs are designed to release in multiple phases. Zolpidem CR is one. Others include methylphenidate ER (Concerta) and certain opioid painkillers. These require partial AUC (pAUC) analysis-measuring drug levels at specific time windows tied to clinical effect. Then there are narrow therapeutic index (NTI) drugs. These are the dangerous ones: small changes in blood levels can mean the difference between no effect and toxicity. Warfarin, levothyroxine, and some antiepileptics fall into this category. For these, the FDA demands tighter limits: 90-111.11% instead of 80-125%. And they require proof that both the brand and generic have similar variability in how patients absorb them. And don’t forget alcohol. Many ER opioids and pain meds contain over 250 mg of active ingredient. If you take them with alcohol, the tablet can dump all its drug at once-called “dose dumping.” That’s led to hospitalizations and even deaths. Since 2015, the FDA has required alcohol testing for these products. Between 2005 and 2015, seven ER products were pulled off the market because of this risk.
Why Developing Generic MR Drugs Costs So Much More
A generic immediate-release pill might cost $500,000 to develop. A generic extended-release version? $5-7 million more. Why? Because the studies are longer, more complex, and require specialized equipment. Single-dose MR bioequivalence studies cost $1.2-1.8 million-up from $0.8-1.2 million for IR. You need advanced dissolution testing (USP Apparatus 3 or 4, not the standard 2), pharmacokinetic modeling software like WinNonlin or NONMEM, and statisticians who understand Reference-Scaled Average Bioequivalence (RSABE). RSABE is used for highly variable drugs-where patient absorption differs wildly from person to person. For these, the acceptable range isn’t fixed at 80-125%. It expands based on how variable the brand drug is. But calculating that? It adds 6-8 months to development time. And failure rates are high. A formulation scientist at Teva reported that 35-40% of early ER oxycodone prototypes failed dissolution testing across all three pH levels. The FDA rejected 22% of MR generic applications between 2018 and 2021 because of inadequate pAUC data.What Happens When Bioequivalence Isn’t Done Right
There’s a myth that if a generic passes regulatory tests, it’s as safe and effective as the brand. But real-world data tells a different story. A 2016 study in Neurology found that 18% of generic extended-release antiepileptic drugs had higher seizure breakthrough rates than the brand-even though they passed all bioequivalence criteria. Why? Because the drug release pattern, while statistically equivalent, wasn’t clinically identical. Patients got slightly lower levels during critical overnight hours. The 2012 rejection of a generic Concerta is another warning. The applicant didn’t properly test the early release phase (0-2 hours). The FDA said: “You didn’t prove the drug comes out when it’s supposed to.” That’s not a minor oversight-it’s a failure of design.How to Get Started With MR Bioequivalence
If you’re a pharmacist, clinician, or even a patient curious about generics, here’s what you should know:- Not all generics are equal. For MR drugs, the release profile matters as much as the dose.
- Stick with FDA-approved generics. Check the Orange Book for approved products and their specific bioequivalence data.
- If you’re switching brands, watch for changes in side effects or effectiveness. Don’t assume “same drug = same result.”
- Ask your pharmacist: “Is this a modified-release generic? Has it been tested for partial AUC or dissolution similarity?”
The Future of Modified-Release Bioequivalence
The field is moving fast. More companies are using physiologically based pharmacokinetic (PBPK) modeling-computer simulations that predict how a drug behaves in the body based on anatomy, pH, and enzyme activity. In 2022, 68% of big pharma firms were using this for MR development. The FDA is also working on a new 2024 guidance for complex MR systems like gastroretentive tablets (that float in the stomach) and multiparticulate beads. These are harder to test because they break apart in different ways. And biowaivers-skip-the-study approvals based on dissolution similarity-are becoming more common. Sandoz got one for an ER tacrolimus product by proving its dissolution profile matched the brand at pH 6.8 with an f2 score of 68. That saved $1.5 million and 10 months. But the bottom line hasn’t changed: modified-release drugs aren’t just about dosage. They’re about timing. And timing, in medicine, can mean the difference between control and crisis.Why can’t we use the same bioequivalence rules for modified-release and immediate-release drugs?
Because immediate-release drugs release all their dose quickly, so total exposure (AUC) and peak level (Cmax) are enough to prove they work the same. Modified-release drugs are designed to release slowly over time. If a generic releases too fast at first or too slow later, patients might get side effects or not enough medicine. That’s why regulators look at partial AUCs, dissolution profiles, and timing-not just total exposure.
What is pAUC and why does it matter for MR drugs?
pAUC stands for partial area under the curve. It measures how much drug is in the blood during a specific time window, like the first 1.5 hours after taking a pill. For multiphasic MR drugs like Ambien CR, the first part releases quickly to help you fall asleep, and the second part keeps you asleep. If the generic doesn’t match the brand in both phases, you might not sleep well-or you might wake up groggy. pAUC ensures each part works as intended.
Are generic modified-release drugs safe?
Most are. FDA-approved generics must meet strict bioequivalence standards. But real-world evidence shows some patients experience changes in effectiveness or side effects after switching-especially with narrow therapeutic index drugs like antiepileptics or blood thinners. If you notice new symptoms after switching to a generic MR drug, talk to your doctor. It’s not always the drug-it could be how it releases in your body.
Why do some MR generics get rejected by the FDA?
Common reasons include: failing dissolution tests across all three pH levels, not measuring pAUC at the right timepoints, not testing for alcohol-induced dose dumping (for high-dose ER products), or not proving similarity in release timing. The FDA rejected 22% of MR generic applications between 2018 and 2021 for these issues.
Can I trust a generic MR drug that’s cheaper than the brand?
Price doesn’t tell you if it’s equivalent. A cheaper generic might have cut corners on testing. Look for FDA approval status in the Orange Book. If it’s listed as “AB-rated,” it’s been proven bioequivalent. If it’s not listed, or if you’re unsure, ask your pharmacist for the manufacturer’s bioequivalence data. Don’t assume cost equals quality.






Alexandra Enns
January 25, 2026 AT 23:37Okay but let’s be real-this whole bioequivalence mess is just Big Pharma’s way of keeping generics expensive. They design these ridiculous multi-phase release profiles so only they can make them, then cry when someone else tries to copy it. The FDA? More like FDA = Fast Drug Approval for the rich. I’ve seen people on $500/month brand meds switch to generics and get seizures. And they wonder why people don’t trust the system?
Marie-Pier D.
January 27, 2026 AT 16:31Thank you for writing this!! 🙏 I’m a pharmacist in Toronto and I see this every day. Patients switch to a generic ER antidepressant and suddenly they’re crying at work or can’t sleep. It’s not ‘all in their head’-it’s the release profile. I always check the Orange Book and ask for the dissolution data. If the manufacturer won’t give it? I don’t dispense it. 💙
Anna Pryde-Smith
January 29, 2026 AT 04:14THIS. I’ve been saying this for YEARS. They test it in healthy young men on an empty stomach. WHAT ABOUT THE 70-YEAR-OLD WOMAN WITH GERD WHO TAKES IT WITH HER COFFEE AND PILL POPPER?!!?? The FDA’s testing is a cartoon. It’s like testing a car’s fuel efficiency only on a flat road at 72°F with no wind. ABSURD. 😤
Stacy Thomes
January 29, 2026 AT 15:52Y’all need to stop panicking. Most generics are fine. I’m a nurse and I’ve given hundreds of ER generics. If your meds feel ‘off,’ talk to your doc-not Reddit. Also, don’t be scared of cheaper options. Sometimes they’re just better made. 😊
dana torgersen
January 29, 2026 AT 17:15so... like... the whole point of MR is timing right? and if the release is even a little off... like... say... 5% too fast in the first hour... then... you know... the body gets a spike... then crashes... and... you get... side effects... or... not enough... and... the body... doesn't... know... what... to... do... and... it's... not... just... about... AUC... it's... about... rhythm... like... a heartbeat... and... if... the... rhythm... is... wrong... the... whole... system... breaks... and... no... one... cares... because... it's... just... a... pill... right?... 🤔
asa MNG
January 30, 2026 AT 11:47bro the FDA is in cahoots with big pharma. they don't want you to know that the 'same' generic you buy at walmart is actually made in a factory in india that uses talcum powder as a filler. and the alcohol thing? they knew about dose dumping for 20 years but waited until people started dying to do anything. also... why do they test at pH 1.2? that's not even real stomach acid. real stomach acid is like 0.8. they're lying to us. 🤡
Shanta Blank
February 1, 2026 AT 09:28Let me get this straight-your ‘generic’ oxycodone ER dissolves like a sugar cube in acid but like a brick in your gut? Congrats, you’ve just turned your painkiller into a time bomb. And the FDA approves this? That’s not science, that’s a horror movie written by a pharma exec who thinks patients are dumb. And don’t even get me started on the fact that the brand name costs $800 and the ‘equivalent’ is $12 but the release profile is a glitchy YouTube video compared to the 4K original. 🎭
Tiffany Wagner
February 1, 2026 AT 12:23I work in a clinic and we had a patient switch from brand to generic Concerta and her focus tanked. We didn’t realize it until she missed three appointments. We switched her back and she cried because she felt like herself again. No one told us the generic didn’t test the first 2 hours properly. We just assumed ‘bioequivalent’ meant ‘same.’ It didn’t. We’re learning. 😔
Vatsal Patel
February 2, 2026 AT 11:21You think this is complicated? Ha. You think regulators care? They care about paperwork. The real question is: why do we let corporations decide how our medicine behaves inside our bodies? The answer: because we let them. The science is just the glitter on the coffin. The real drug is profit. You’re not sick-you’re a revenue stream. 🤡
Sharon Biggins
February 3, 2026 AT 13:25if you're switching generics and feel weird... don't panic. write down your symptoms. talk to your pharmacist. they can often tell you if it's a new manufacturer. and if you're on a tight budget... ask about patient assistance programs. you're not alone. 💪
John McGuirk
February 4, 2026 AT 13:36they’re testing at pH 6.8? that’s the small intestine. but what if your gut is inflamed? what if you have IBS? what if you’re on antibiotics? they’re not testing real people. they’re testing lab rats with perfect digestion. this is all a lie. the whole system is rigged. and the WHO? they’re just the PR arm for Big Pharma. you think they want you to know how many people die from dose dumping? no. they want you to think it’s safe. it’s not.
Michael Camilleri
February 5, 2026 AT 16:55People who trust generics are naive. You think a company that cuts corners on pills is going to care about your health? They care about profit. If you take a generic ER opioid and it dumps in your gut because the coating failed? You’re not just at risk-you’re a statistic they already counted. And if you die? They’ll say you were ‘non-compliant.’
Marlon Mentolaroc
February 7, 2026 AT 08:43Fun fact: the reason MR generics cost 10x more to develop is because they have to reverse-engineer the exact coating, bead size, polymer blend, and dissolution curve of the brand. That’s not ‘science’-that’s espionage. And if you think the FDA is impartial, you’ve never seen the revolving door between regulators and pharma execs. They’re not protecting you-they’re protecting the playbook.