Generic Drug Savings Calculator
When you pick up a prescription, you might see two different pills on the counter: one with a fancy name like Lipitor, and another labeled simply as atorvastatin. You might wonder-does it really work the same? Is one safer? Is the cheaper one just a knockoff? The answer isn’t as complicated as it seems, but the labels sure make it look that way.
Same Active Ingredient, Different Look
Generic drugs aren’t copies. They’re exact matches in what matters most: the active ingredient. That’s the part that actually treats your condition. If you’re taking a generic version of omeprazole, it’s the same molecule as the one in Prilosec. The FDA requires it. Every single time. The active ingredient must be identical in strength, dosage form, and how it works in your body. That’s not a suggestion-it’s the law.The differences? They’re all on the outside. Color, shape, size, even the imprint on the pill. Those are controlled by trademark laws, not medical need. A brand-name company can’t let a generic look the same-it would confuse customers and risk legal trouble. So generics get different colors, different logos, different shapes. But that doesn’t change how the medicine works. A blue pill and a white pill with the same active ingredient? They’re therapeutically identical.
Labeling: What’s Written vs. What’s Hidden
Look at the label on your brand-name drug. It says Prilosec, Lipitor, Viagra. Those are brand names-marketing tools. The generic label? It says omeprazole, atorvastatin, sildenafil. Those are the chemical names. That’s it. No fancy packaging, no celebrity ads, no catchy slogans. Just the facts.But here’s the important part: everything else on the label has to match. The FDA mandates that generic drug labels include the same indications, dosing instructions, warnings, side effects, and contraindications as the brand. If the brand says “may cause dizziness,” so does the generic. If it warns against use with grapefruit juice, the generic says the same thing. The FDA’s 2021 guidance makes this crystal clear: labeling must be identical in content, even if the formatting looks slightly different.
That means the information you rely on to know when to take it, what to avoid, and what side effects to watch for? It’s the same. No hidden warnings. No missing risks. Just a simpler label.
Therapeutic Equivalence: What the FDA Actually Requires
The FDA doesn’t just say generics are “close enough.” They prove it. Every generic drug must pass a test called bioequivalence. That means it has to get into your bloodstream at the same rate and to the same level as the brand-name version. The standard? The amount of drug absorbed (measured as AUC) and the peak concentration (Cmax) must fall within 80% to 125% of the brand’s numbers. That’s a tight range.Think of it like this: if your brand-name drug delivers 100 units of medicine into your blood, the generic can deliver between 80 and 125 units. That’s not a wide gap-it’s actually tighter than the natural variation you’d see between two different batches of the same brand-name drug. As Dr. Ameet Nagpal from Northwestern Medicine pointed out in 2023, the body’s own response to the same drug can vary more than the difference between brand and generic.
These tests are done in healthy volunteers-usually 24 to 36 people-before the drug ever hits shelves. And it’s not a one-time check. The FDA inspects manufacturing facilities just as rigorously for generics as they do for brand-name companies. No shortcuts. No exceptions.
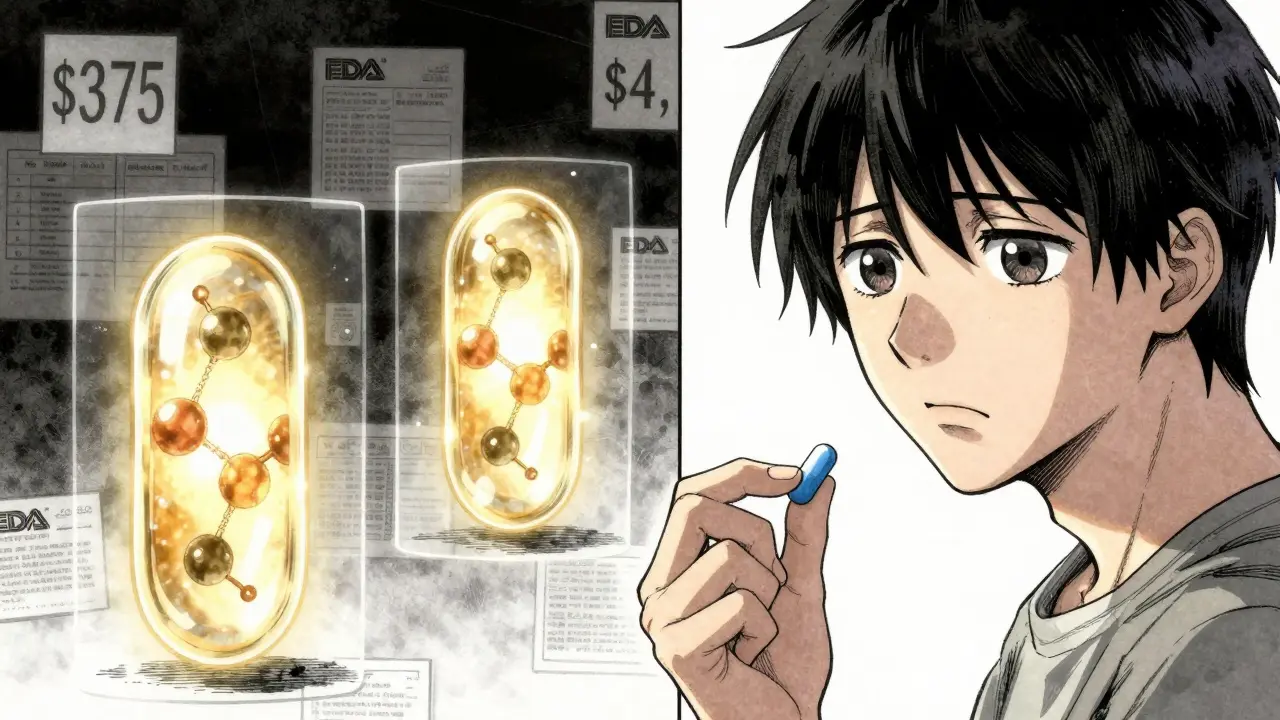
Cost: The Real Difference
Here’s where things get real. A brand-name drug like Lipitor (atorvastatin) cost around $375 a month in 2023. The generic? $4 at Walmart. That’s not a typo. The same medicine. Same effectiveness. Same safety. But 99% cheaper.That’s not luck. It’s the result of the Hatch-Waxman Act of 1984, which created the legal pathway for generic drugs to enter the market without repeating expensive clinical trials. Generic manufacturers don’t have to pay for the original research, marketing, or advertising. They just have to prove they’re the same. That’s why generics make up 90% of all prescriptions filled in the U.S.-but only 25% of total drug spending.
Since 2007, generic drugs have saved the U.S. healthcare system over $1.67 trillion. In 2023 alone, that number was $313 billion. That’s money staying in patients’ pockets, reducing insurance premiums, and keeping hospitals from cutting services. And the FDA says 90% of generics cost less than $10 per month.
When Generics Might Need Extra Care
Most of the time, switching from brand to generic is seamless. But there are exceptions. For drugs with a narrow therapeutic index (NTI), even tiny changes in blood levels can cause problems. That’s why the FDA specifically flags a few: warfarin (blood thinner), levothyroxine (thyroid hormone), and phenytoin (seizure control).In these cases, doctors often monitor patients more closely when switching-especially if you’re going from one generic manufacturer to another. Why? Because while each generic meets FDA standards, different manufacturers might use slightly different inactive ingredients. For most people, that’s no issue. But for someone on warfarin, a small change in absorption could affect INR levels. That’s why pharmacists and doctors keep an eye on lab results during the switch.
It’s not that generics are less safe. It’s that for these specific drugs, the body is less forgiving. That’s why the FDA’s Orange Book lists therapeutic equivalence ratings. Look for an “A” rating. That means the generic is approved as interchangeable. “B” ratings? Those aren’t interchangeable. Stick with the brand unless your doctor says otherwise.

What Patients Actually Experience
Real-world data backs this up. A 2021 study in JAMA Internal Medicine tracked 2 million patients on cardiovascular drugs. No difference in heart attacks, strokes, or hospitalizations between brand and generic users. A 2023 review in BMJ Open analyzed 47 clinical trials. Same result: no drop in effectiveness.On Drugs.com, generic atorvastatin has a 6.6/10 rating from over 1,800 reviews. Lipitor? 6.3/10. That’s not a win for the brand. That’s a win for the generic.
But people do notice the change in appearance. A University of Michigan study found 12% of patients felt uneasy when their pills looked different. One woman told her pharmacist she stopped taking her blood pressure med because “the blue pill I used to take was gone.” She didn’t realize it was the same drug-just a different manufacturer. That’s why pharmacists now often explain the change before handing over the bottle.
And the cost savings? Huge. A Kaiser Permanente survey in 2022 found 78% of patients said generic prices let them actually fill their prescriptions instead of skipping doses or splitting pills.
How to Make Sure You’re Getting the Right One
You don’t need a degree in pharmacology to navigate this. Here’s what to do:- Ask your pharmacist: “Is this a generic? Is it FDA-approved?” They’re trained to answer this.
- Check the label. If it says the chemical name (like “metformin”), it’s generic. If it says “Glucophage,” it’s brand.
- Use the FDA’s Orange Book online (or ask your pharmacist to check it). Look for “A” ratings for interchangeable generics.
- If you’re on a narrow therapeutic index drug (warfarin, levothyroxine, etc.), ask your doctor if they want you to stick with the same generic manufacturer.
- Don’t panic if your pills change color. Call your pharmacist if you’re unsure-they’ll confirm it’s the same medicine.
In 49 states, pharmacists can switch your brand to generic automatically unless your doctor writes “Dispense as Written.” That’s not a loophole-it’s a system designed to save money and keep people on their meds.
The Future of Generics
The FDA approved its first generic version of Ozempic (semaglutide) in September 2023. That’s a big deal-this is a high-demand, high-cost drug. More complex generics are coming: inhalers, injectables, patches. The agency is speeding up reviews for these through GDUFA III, aiming for 10-month approval timelines for priority applications.And it’s not just about saving money. It’s about access. A 2023 report showed that 268 billion dollars in brand-name drug sales will face generic competition by 2028. That means more people will get the medicines they need, without the financial burden.
Generics aren’t second-rate. They’re the backbone of modern pharmacy. They’re rigorously tested, legally required to be identical in effect, and proven safe in millions of real-world patients. The only real difference? The price tag-and the label.







gary ysturiz
January 13, 2026 AT 04:40Generics are the real MVPs of pharmacy. I used to think brand-name was better until I switched my blood pressure med and saved $300 a month. Same pill. Same results. My doctor didn't even notice.
Stop overthinking the color change. Your body doesn't care if it's blue or white.
Jessica Bnouzalim
January 14, 2026 AT 20:40OMG YES!! I used to panic every time my pills looked different-like my medicine was being swapped out for some sketchy knockoff!!
Then my pharmacist sat me down and showed me the FDA label match-same active ingredient, same warnings, same everything!!
Now I ask for generics every time-and I’ve saved over $2,000 in two years!!
Also, my anxiety about pills? Gone. Thank you, science!!
laura manning
January 15, 2026 AT 19:17While the FDA's bioequivalence standards are statistically rigorous, the 80-125% AUC/Cmax range is not biologically inert. Variability in excipients can still influence dissolution kinetics, particularly in patients with gastrointestinal pathologies or polypharmacy regimens.
Moreover, the absence of post-marketing surveillance mandates for generics creates a de facto regulatory blind spot. The JAMA study cited, while large, lacks stratification by manufacturer or bioavailability outliers.
Therefore, while the generalization holds for most, it is not universally applicable without clinical context.
TiM Vince
January 16, 2026 AT 11:12My grandma switched from Lipitor to atorvastatin after her Medicare Part D deductible. She was scared. Took her two weeks to trust it. Then she told me, ‘I feel the same, and I’ve got $300 extra in my pocket.’
That’s the real story. Not the science. Not the labels. The money.
People don’t need to understand bioequivalence. They just need to know it won’t kill them.
Sumit Sharma
January 16, 2026 AT 12:06As a pharmacist in Mumbai, I’ve seen generics save lives in low-income communities where brand-name drugs are unaffordable. The FDA standards are global benchmarks-India’s DCI and WHO prequalification follow similar protocols.
But here’s the catch: not all generics are created equal. Some Indian manufacturers cut corners on excipients. Always check the manufacturer’s reputation and regulatory status.
Don’t just assume ‘generic = safe.’ Verify. Always.
Jay Powers
January 16, 2026 AT 22:29Just want to say thank you to the pharmacist who explained to me why my new pill looked nothing like the old one
It felt weird at first but now I just look at the name on the bottle
If it says atorvastatin I know I’m good
And I’m saving so much money I can finally afford my gym membership
Thanks for making this simple
Lawrence Jung
January 18, 2026 AT 21:17People think the system is fair because the FDA says so
But who really benefits? The pharmaceutical corporations
They made billions on brand names then let generics in when the patent expired
It’s not altruism. It’s capitalism
And we’re just happy to get the crumbs
Still… I take the generic. I’m not stupid.
Alice Elanora Shepherd
January 19, 2026 AT 06:09For those concerned about NTI drugs: I’ve worked in endocrinology for 18 years, and levothyroxine variability is the most common cause of under- or over-treatment in hypothyroid patients.
Once a patient switches manufacturers-even within generics-the TSH can drift by 1-2 points. Not catastrophic, but enough to cause fatigue or palpitations.
Always request the same manufacturer. Write ‘brand only’ on the script if necessary. Your thyroid will thank you.
Katherine Carlock
January 21, 2026 AT 05:32I used to hate generic pills because they made me feel like I was settling for less
Then I started reading the labels and realized I was the one being manipulated by marketing
Now I feel like a smart shopper, not a cheapskate
And I tell all my friends to do the same
Also, the white oval pill with ‘50’ on it? Still the same as the blue one. I swear.
Sona Chandra
January 21, 2026 AT 16:48Why do people still trust the FDA? They let Big Pharma write the rules!
Generics are fine until you get one from a factory in China that uses talc from a mine that’s also used for construction dust!
My cousin took a generic blood thinner and nearly bled out-no one told her the filler changed!
Stop glorifying generics. They’re a gamble. And someone’s making money off your fear.