Vascular Pregnancy Risk Assessment
How This Works
This tool helps you understand pregnancy risks associated with your vascular condition. Results are based on standard medical guidelines and should not replace professional medical advice.
Important Note
Always consult your healthcare team before making any medical decisions. This assessment is for informational purposes only.
Pregnancy Risks
Management Strategies
Red Flag Symptoms
Finding out you have a vascular condition just before or during pregnancy can feel like a punch to the gut. You start worrying about the baby, the delivery, and whether your own health will survive the strain. The good news? With the right knowledge, solid monitoring, and sensible lifestyle tweaks, most women navigate pregnancy safely even with vascular disease.
- Vascular disease can change how blood flows, raising the chance of complications during pregnancy.
- Common issues include hypertension, varicose veins, deep‑vein thrombosis, peripheral artery disease, and aortic aneurysms.
- Early screening, medication adjustments, and regular check‑ups keep risks low.
- Stay active, hydrate, and wear compression stockings when advised.
- Know the red‑flag symptoms that need immediate medical attention.
Understanding Vascular Disease in Pregnancy
Vascular disease is a broad term for any disorder that affects the blood vessels-arteries, veins, and capillaries. It can narrow, weaken, or block vessels, making blood flow less efficient. When a woman becomes pregnant, her heart pumps about 30‑50 % more blood, so any underlying vessel problem can become magnified.
Pregnancy itself isn’t a disease, but the hormonal surge (especially estrogen and progesterone) relaxes vessel walls and increases blood volume. For most women this adaptation is harmless, but if you already have a vascular condition, the extra workload may trigger symptoms or complications.
Common Vascular Conditions That Affect Pregnancy
While every vascular disease is unique, a handful of conditions show up most often in prenatal clinics. Below is a quick snapshot of each, how it shows up, and why it matters for you and your baby.
| Condition | Typical Pregnancy Risk | Key Management Tips |
|---|---|---|
| Hypertension | Pre‑eclampsia, placental insufficiency, early delivery | Low‑salt diet, regular BP checks, safe antihypertensives (e.g., labetalol) |
| Varicose veins | Pain, swelling, rare thrombosis | Compression stockings, leg elevation, gentle exercise |
| Deep vein thrombosis (DVT) | Pulmonary embolism, leg pain, swelling | Low‑molecular‑weight heparin (if prescribed), movement breaks |
| Peripheral artery disease | Reduced limb perfusion, ulceration | Smoking cessation, supervised walking program, vascular imaging |
| Aortic aneurysm | Rupture risk during labor, need for early delivery | Serial imaging, possible elective C‑section, cardiology consult |
How Pregnancy Changes Your Vascular System
During pregnancy, the maternal cardiovascular system undergoes three major shifts:
- Blood volume rises by roughly 40‑50 %, stretching veins and arteries.
- Hormones soften the smooth muscle in vessel walls, lowering systemic resistance.
- The heart rate climbs 10‑20 beats per minute, boosting cardiac output.
These changes help deliver oxygen and nutrients to the growing fetus, but if a vessel is already narrowed or fragile, the extra pressure can cause it to leak, clot, or even burst.

Risks for Mother and Baby
Every vascular problem carries its own mix of maternal and fetal concerns. The most common red‑flag outcomes include:
- Pre‑eclampsia - high blood pressure with protein in the urine; can lead to organ damage.
- Placental insufficiency - the placenta doesn’t get enough blood, causing low birth weight or growth restriction.
- Thrombo‑embolic events - clots that travel to the lungs (pulmonary embolism) are life‑threatening.
- Pre‑term birth - many doctors recommend delivering early to protect the mother’s heart.
- Maternal heart failure - rare, but possible if an aneurysm ruptures or severe hypertension goes untreated.
Precautions and Management Strategies
Knowing the risks is only half the battle. Proactive steps can dramatically lower the chance of trouble.
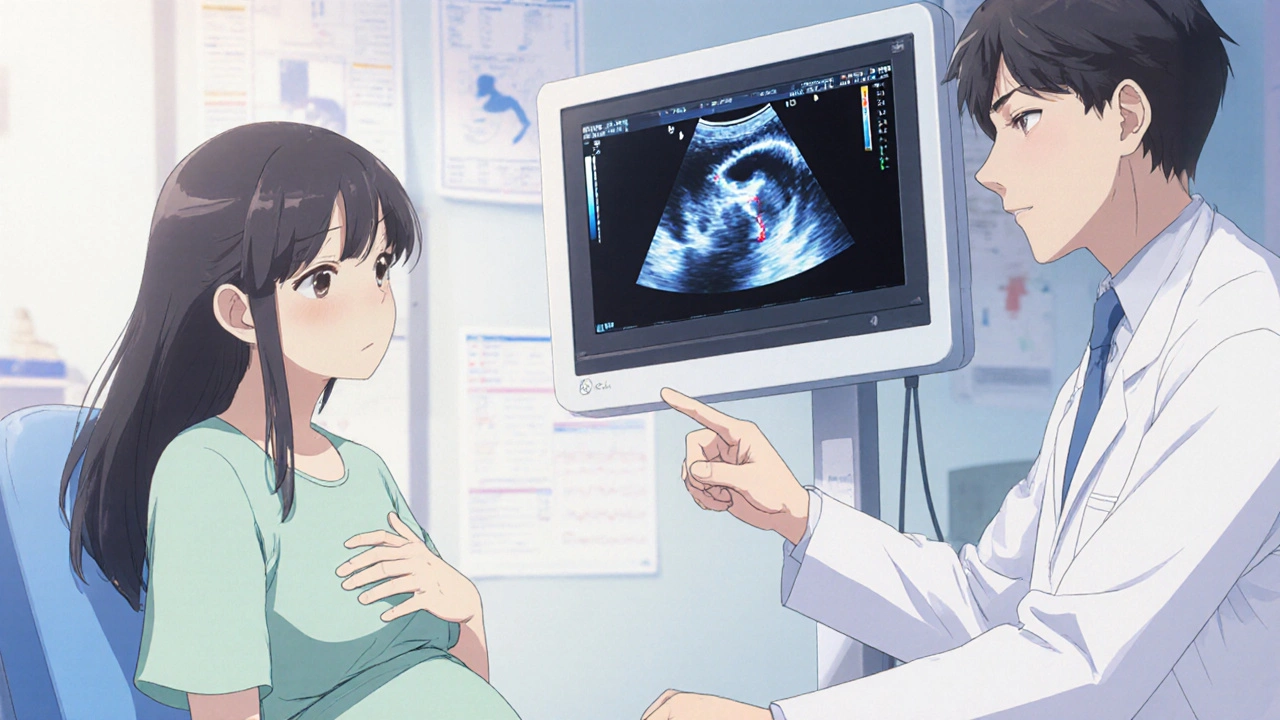
1. Early and Ongoing Screening
Ask your obstetrician for a baseline ultrasound screening at 12‑14 weeks, then a detailed Doppler study around 20 weeks to check blood flow to the placenta. If you have a known aneurysm, serial MR or CT angiograms (low‑dose) may be scheduled.
2. Medication Review
Some blood‑pressure drugs are unsafe in pregnancy (e.g., ACE inhibitors). Your physician will likely switch you to labetalol, nifedipine, or methyldopa. For clot‑prone conditions, low‑molecular‑weight heparin is the preferred anticoagulant because it doesn’t cross the placenta.
3. Lifestyle Tweaks
- Stay moving: short walks every hour keep blood from pooling in the legs.
- Hydrate: aim for at least 2‑3 liters of water daily.
- Wear compression stockings if varicose veins or DVT risk is high.
- Eat a balanced diet rich in leafy greens, lean protein, and omega‑3 fatty acids.
4. Specialist Collaboration
Bring a vascular surgeon or cardiologist into your prenatal team. Joint clinics where obstetrics, cardiology, and anesthesia discuss the birth plan can prevent surprises on delivery day.
5. Birth Planning
For most vascular conditions, a vaginal birth is safe if blood pressure remains controlled. However, an aortic aneurysm or severe hypertension may call for an elective C‑section before labor starts. Discuss timing, anesthesia type, and postpartum monitoring well ahead of time.
When to Seek Immediate Care
Even with careful planning, emergencies can happen. Call your doctor or go to the nearest emergency department if you notice any of these signs:
- Sudden, severe leg swelling or pain-possible DVT.
- Sharp chest or back pain with a feeling of “pressure”-could signal aneurysm stress.
- Headache, visual changes, or swelling of hands/face-warning of pre‑eclampsia.
- Shortness of breath, rapid heartbeat, or coughing up blood-possible pulmonary embolism.
Prompt treatment can protect you and your baby, so keep your contact numbers handy and don’t dismiss unusual symptoms.
Frequently Asked Questions
Frequently Asked Questions
Can I have a normal vaginal delivery with varicose veins?
Yes. Varicose veins rarely affect labor. Wearing compression stockings during pregnancy and on the day of delivery helps keep blood flowing and reduces swelling.
Is it safe to take aspirin for hypertension in pregnancy?
Low‑dose aspirin (81 mg) is often prescribed to lower pre‑eclampsia risk, but it must be cleared by your obstetrician. Higher doses can interfere with platelet function and are not recommended.
How often should I have blood‑pressure checks?
If you have a known vascular condition, weekly checks are common. Some clinics ask you to record home readings twice daily and bring a log to each appointment.
Can I travel abroad while on blood‑thinners?
Yes, but plan ahead. Carry a letter from your doctor, keep medication in your hand luggage, and stay hydrated. Avoid long, immobile flights - stand up and walk every hour.
What lifestyle changes matter most?
Gentle daily exercise (walking, prenatal yoga), a low‑salt diet, staying well‑hydrated, and quitting smoking are the three biggest factors that lower both maternal and fetal risk.





nitish sharma
October 18, 2025 AT 18:13Congratulations on taking the initiative to understand how vascular disease intersects with pregnancy; early awareness is the cornerstone of a safe gestation. It is essential to schedule a comprehensive cardiovascular evaluation before conception, including Doppler ultrasound and baseline blood pressure monitoring. Discuss with your obstetrician the possibility of adjusting any teratogenic medications, such as ACE inhibitors, well in advance. Incorporate low‑salt meals and a balanced intake of omega‑3 fatty acids to support vascular health. Regular, moderate exercise-such as prenatal yoga or daily walking-helps maintain circulation without overburdening the heart. Hydration should not be overlooked; aim for at least two to three liters of water each day. If you have a history of varicose veins or deep‑vein thrombosis, wear graduated compression stockings during the second trimester and on labor day. Establish a routine of weekly blood‑pressure checks, noting any sudden spikes that warrant immediate medical attention. Collaborate with a multidisciplinary team, including a cardiologist or vascular surgeon, to tailor a birth plan that aligns with your specific condition. Finally, keep a written log of symptoms, medication changes, and appointment outcomes to share with each specialist you see. By adhering to these precautions, you empower both yourself and your baby to navigate pregnancy with confidence and reduced risk.
Rohit Sridhar
October 22, 2025 AT 05:33Great points above! I’d add that keeping a positive mindset truly helps your body respond better to the extra cardiac load. When I was expecting my second child, I set daily reminders to stand up, stretch, and take a short walk-those micro‑breaks made a huge difference in leg comfort. Also, don’t underestimate the power of a good prenatal vitamin fortified with folic acid and iron; they aid both vascular function and fetal development. If you ever feel a fluttering or mild chest discomfort, jot it down and discuss it promptly-early intervention is always better than waiting. Remember, the goal is not just to survive pregnancy but to thrive throughout the journey.
Nhasala Joshi
October 25, 2025 AT 16:53🌪️💉 Did you know the pharma giants are *pushing* a one‑size‑fits‑all pill for pregnant women with vascular disease? They don’t want you to read the fine print about long‑term clot risks! 😱 The hidden agenda is to keep you dependent on brand‑name anticoagulants while they cash in on the hype. Stay vigilant, question every “standard protocol,” and demand personalized care that isn’t filtered through a corporate lens. 🕵️♀️✨
Joe Moore
October 29, 2025 AT 03:13lol, Nhasala, u sound like one of those tinfoil‑hat vloggers. sure, pharma makes big $$, but doctors actually test these meds for safety in pregnancy. i mean, the guidelines exist for a reason – they’re not just some cash‑grab. still, keep ur eyes open, but dont let scare tactics ruin ur pregnancy vibes.
Ayla Stewart
November 1, 2025 AT 14:33I appreciate the detailed overview. For readers who wonder about the frequency of prenatal visits, most specialists recommend a check‑up every four weeks until 28 weeks, then every two weeks, and weekly after 36 weeks, especially when vascular issues are present. This schedule allows timely adjustments to medication and monitoring of blood‑pressure trends.
Poornima Ganesan
November 5, 2025 AT 01:53While the article provides a solid baseline, there are several nuances that deserve explicit mention. First, the traditional emphasis on low‑dose aspirin for pre‑eclampsia prophylaxis often overlooks the fact that aspirin resistance can be genotype‑dependent, rendering the therapy ineffective in a subset of patients. Second, compression stockings, though beneficial for venous stasis, should be pressure‑graded based on ankle circumference; a one‑size‑fits‑all approach may actually exacerbate arterial inflow obstruction in cases of peripheral artery disease. Third, the recommendation to increase fluid intake must be balanced against the risk of iatrogenic hyponatremia, especially in women already on diuretics for hypertension control. Fourth, regarding anticoagulation, low‑molecular‑weight heparin (LMWH) dosing should be weight‑adjusted and monitored via anti‑Xa levels; fixed dosing can lead to sub‑therapeutic exposure, increasing the chance of DVT recurrence. Fifth, the article’s suggestion of elective cesarean delivery for aortic aneurysms omits the critical role of endovascular repair in select cases, which can convert a high‑risk surgical scenario into a relatively low‑risk elective procedure. Sixth, the psychological impact of chronic vascular disease during pregnancy is often underestimated; a structured counseling program can mitigate anxiety‑related hypertension spikes. Seventh, many patients are unaware that certain dietary supplements, such as high‑dose vitamin E, have been linked to increased clotting risk and should be avoided. Eighth, for patients with peripheral artery disease, supervised interval walking programs have been shown to improve ankle‑brachial indices by up to 0.15, which is clinically meaningful. Ninth, the role of telemedicine in longitudinal monitoring of blood‑pressure trends can reduce missed appointments and allow rapid medication adjustments. Tenth, the interplay between gestational diabetes and vascular disease can amplify endothelial dysfunction, necessitating stricter glycemic targets. Eleventh, the postpartum period carries a lingering risk of thrombo‑embolic events for up to six weeks, so continuation of LMWH should be individualized rather than automatically discontinued. Twelfth, the importance of postpartum pelvic floor rehabilitation should be highlighted, as it can improve venous return and reduce varicose vein progression. Thirteenth, there is emerging evidence that low‑dose nitric‑oxide donors may ameliorate endothelial dysfunction in pregnant patients with hypertension, though they remain off‑label. Fourteenth, in cases of severe hypertension unresponsive to first‑line agents, magnesium sulfate can serve both as a seizure prophylaxis and a vasodilator. Finally, the article fails to address the need for a clear hand‑off protocol between obstetrics and cardiology teams during labor-without this, critical information may be lost, jeopardizing both maternal and fetal outcomes.
Janet Morales
November 8, 2025 AT 13:13Forget all the guidelines – listen to your gut.
Tracy O'Keeffe
November 12, 2025 AT 00:33Oh, dear, yet another ivory‑tower write‑up that pretends to distill complex hemodynamics into a checklist of bland bullet points. One must appreciate the audacity of reducing a symphony of vascular remodeling, neuro‑humoral feedback loops, and placental‑maternal cross‑talk to “stay hydrated” and “wear stockings.” If we truly wish to elevate discourse, let us invoke the principle of *vascular plasticity* – the dynamic adaptation of endothelial shear stress in response to gestational hormonal flux. Moreover, the discourse neglects the emerging field of *materno‑fetal angiogenic profiling*, wherein circulating sFlt‑1/PlGF ratios guide therapeutic stratification. Such nuances deserve a paragraph, not a footnote. And, for the love of all that is scholarly, let us abandon the pedestrian phrase “good diet” and instead discuss the macro‑micronutrient interplay that modulates nitric oxide bioavailability. In short, the article is a commendable primer but falls short of the intellectual rigor demanded by clinicians who navigate the labyrinthine corridors of obstetric vascular care.
Rajesh Singh
November 15, 2025 AT 11:53It is morally incumbent upon us to place the well‑being of the unborn child above any personal inconvenience, and that starts with strict adherence to evidence‑based protocols, not whimsical speculation. When a pregnant woman with a compromised vascular system ignores professional advice, she risks transforming a manageable condition into a preventable tragedy. The ethical duty of healthcare providers is to enforce these standards, offering clear guidance while holding patients accountable for their choices. Only through collective responsibility can we safeguard both mother and child.