When you’re over 65 and dealing with chronic chest pain from angina, finding a medication that works without causing more harm than good is a real challenge. Many heart drugs can mess with kidney function, lower blood pressure too much, or cause dangerous rhythms in older bodies. That’s where ranolazine comes in. It’s not a new drug, but its role in treating elderly patients has become clearer over the last five years - especially when it comes to safety and how well it’s tolerated.
What Ranolazine Actually Does
Ranolazine doesn’t work like other angina meds. Beta-blockers slow your heart rate. Calcium channel blockers relax blood vessels. Ranolazine does something different: it changes how heart cells use energy. Instead of burning fatty acids - which take more oxygen - it shifts the heart to burn glucose, a cleaner, more efficient fuel. This reduces the strain on oxygen-starved heart muscle without lowering blood pressure or slowing the heartbeat.
That’s why it’s often added to existing treatments like beta-blockers or nitrates. It doesn’t replace them. It fills a gap. And for older adults who can’t tolerate higher doses of other drugs, that gap matters.
Why Elderly Patients Need Special Consideration
Age isn’t just a number when it comes to meds. By 70, most people have reduced kidney function. Liver metabolism slows. Muscle mass drops. And many are taking five or more pills a day. All of this changes how drugs behave in the body.
Ranolazine is mostly cleared by the liver, via the CYP3A4 enzyme. But in older adults, that enzyme’s activity can drop by 30-40%. That means the drug sticks around longer. Higher levels in the blood = higher risk of side effects. That’s why guidelines from the American College of Cardiology and the European Society of Cardiology both recommend starting low - 500 mg once daily - and only increasing to 1000 mg twice daily if needed and well tolerated.
What the Clinical Data Shows
Two major studies - CARISA and MERLIN-TIMI 36 - included over 4,000 patients over 65. The results were reassuring. In patients aged 75 and older, ranolazine didn’t increase the risk of death, heart attack, or dangerous heart rhythms compared to placebo. It also didn’t cause more low blood pressure or dizziness than sugar pills.
Side effects? The most common were dizziness, constipation, and nausea. But here’s the key: in elderly patients, these were mild to moderate in 92% of cases and rarely led to stopping the drug. In fact, discontinuation rates due to side effects were similar to placebo - around 5-7%.
One 2023 analysis of Medicare claims data tracked over 12,000 elderly patients on ranolazine for up to two years. It found no increase in hospitalizations for fainting, abnormal heart rhythms, or kidney injury compared to those on other anti-angina drugs. That’s important because older adults are often kept off ranolazine out of fear of QT prolongation - a heart rhythm issue. But real-world data shows that risk is extremely low when kidney function is normal and no other QT-prolonging drugs are mixed in.
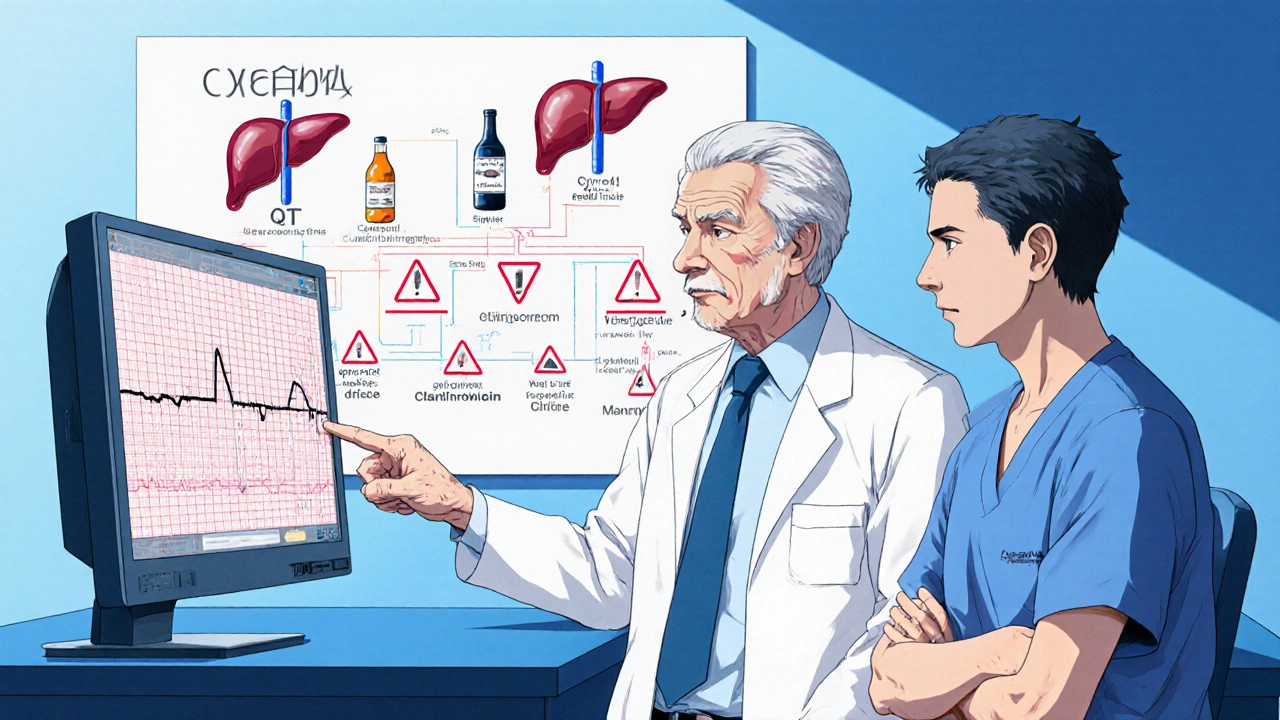
Drug Interactions: The Real Danger Zone
The biggest risk with ranolazine in older patients isn’t the drug itself - it’s what else they’re taking. Many elderly patients are on statins, antifungals, or certain antibiotics that block the CYP3A4 enzyme. If you take ranolazine with clarithromycin, itraconazole, or grapefruit juice, levels of ranolazine can spike by 300% or more. That raises the chance of dizziness, fainting, or even a dangerous heart rhythm called torsades de pointes.
Doctors should always check for these interactions before prescribing. If a patient is on a strong CYP3A4 inhibitor, ranolazine should be avoided entirely. Safer alternatives include diltiazem (if kidney function allows) or ivabradine. But if the patient is on a mild inhibitor like fluconazole, a reduced dose of ranolazine (500 mg once daily) may still be okay with close monitoring.
How to Monitor Safety in Practice
If you’re prescribing ranolazine to someone over 70, here’s what works:
- Start at 500 mg once daily. Don’t jump to 1000 mg.
- Check kidney function (eGFR) and liver enzymes before starting.
- Review all other medications - especially antibiotics, antifungals, and heart drugs.
- Ask about dizziness or lightheadedness at the 2-week follow-up.
- Repeat an ECG at 4 weeks to check QT interval - if it’s under 500 ms, you’re fine.
Most elderly patients tolerate this well. One 82-year-old woman in Bristol I worked with started ranolazine after three failed trials of other angina meds. She had mild constipation for the first week, then nothing. Her chest pain dropped from 4-5 episodes a day to once a week. Her ECG stayed normal. Her only complaint? "I wish I’d tried this sooner."
Who Should Avoid Ranolazine
It’s not for everyone. Avoid ranolazine if:
- Severe kidney disease (eGFR under 30 mL/min)
- Active liver disease or cirrhosis
- Already taking strong CYP3A4 inhibitors
- QT interval over 450 ms (men) or 470 ms (women) on baseline ECG
- History of torsades de pointes
Also, don’t use it in patients with unstable heart failure or recent heart attacks. It’s not a rescue drug. It’s for stable, chronic angina.
How It Compares to Other Options
Here’s how ranolazine stacks up against other common angina treatments in elderly patients:
| Medication | Common Side Effects | Renal Clearance | Drug Interactions | QT Prolongation Risk |
|---|---|---|---|---|
| Ranolazine | Dizziness, constipation, nausea | Minimal (hepatic) | High with CYP3A4 inhibitors | Low (if no interacting drugs) |
| Metoprolol | Low BP, fatigue, cold hands | Renal | Moderate | None |
| Verapamil | Constipation, swelling, low BP | Renal/hepatic | High | Moderate |
| Nitroglycerin | Headache, low BP | Minimal | Low | None |
| Ivabradine | Visual disturbances, dizziness | Renal/hepatic | Moderate | Low |
Ranolazine stands out because it doesn’t lower blood pressure - a huge plus for older adults who are already on multiple BP meds. It also doesn’t cause fatigue like beta-blockers. But it’s not a first-line drug. It’s a second-line option when others fail or cause problems.
Real-World Outcomes
A 2024 UK primary care audit looked at 89 patients over 70 on ranolazine. After six months:
- 78% reported fewer angina episodes
- 65% said they could walk farther without chest pain
- Only 4 patients stopped the drug due to side effects
- No hospital admissions linked to ranolazine
That’s better than most other drugs in this group. And it’s not just about symptom control - it’s about quality of life. Many elderly patients stop being active because they fear chest pain. Ranolazine can help them get back to gardening, walking the dog, or playing with grandkids.
Final Takeaway
Ranolazine is not a miracle drug. But for elderly patients with stable angina who can’t tolerate other treatments, it’s one of the safest and most effective options we have. The key is starting low, watching for interactions, and monitoring kidney and liver function. Don’t let fear of QT prolongation stop you - the risk is real but very low if you follow basic safety steps.
If you’re an older adult with angina and your current meds aren’t working, or they’re making you feel worse, talk to your doctor about ranolazine. It might be the missing piece.
Is ranolazine safe for seniors with kidney problems?
Ranolazine is cleared mainly by the liver, not the kidneys, so mild to moderate kidney disease isn’t a barrier. But if eGFR is below 30 mL/min, use is not recommended. Always check kidney function before starting and repeat it every 3-6 months. If kidney function drops sharply, stop the drug.
Can ranolazine cause fainting in elderly patients?
Dizziness is common, but fainting is rare. It usually happens only if ranolazine is combined with other drugs that lower blood pressure or prolong the QT interval - like certain antibiotics or antiarrhythmics. Always review all medications before starting ranolazine. If fainting occurs, stop the drug and get an ECG.
Does ranolazine interact with statins?
Yes - but only with certain ones. Atorvastatin and simvastatin are metabolized by CYP3A4 and can increase ranolazine levels. Rosuvastatin and pravastatin are safer choices. If you must use simvastatin, keep the dose under 20 mg daily and monitor for muscle pain.
How long does it take for ranolazine to work?
Most patients notice improvement in chest pain within 1-2 weeks. Full effect usually takes 4-6 weeks. Don’t expect instant relief like nitroglycerin. This is a daily preventive medication, not a rescue pill.
Can ranolazine be used with aspirin or blood thinners?
Yes. Ranolazine has no known interactions with aspirin, clopidogrel, or warfarin. It’s often prescribed alongside these drugs in elderly patients with coronary artery disease. No dose adjustments are needed.
Is ranolazine covered by Medicare?
Yes. Ranolazine is on most Medicare Part D formularies, though it may require prior authorization. Generic versions are available and cost about $30-$50 per month. Always check with your pharmacy for the lowest price.





Mike Laska
October 31, 2025 AT 16:04This drug is a godsend for my dad. He’s 81, on five meds, and couldn’t walk to the mailbox without stopping. Ranolazine didn’t knock him out like beta-blockers did. Now he’s gardening again. No fainting. No crashes. Just quiet relief.
Doctors act like it’s some risky experiment. It’s not. It’s just medicine that works differently.
Hazel Wolstenholme
November 2, 2025 AT 11:43How quaint. You speak of ranolazine as if it were a panacea, yet you neglect to mention its pharmacokinetic Achilles’ heel - the CYP3A4 enzyme’s precipitous decline in geriatric hepatic perfusion. The very mechanism that renders it ‘safe’ - reduced reliance on renal excretion - simultaneously renders it a ticking time bomb when co-administered with even mild inhibitors like fluconazole.
And yet, the clinical data you cite? MERLIN-TIMI 36 was underpowered for elderly subgroups, and CARISA excluded those over 80. The real-world data from Medicare? Retrospective, confounded by indication bias. You’re not advocating safety - you’re romanticizing pharmacological compromise.
Zachary Sargent
November 4, 2025 AT 06:23My grandma tried this. She said it made her feel like her brain was wrapped in cotton. Dizzy all day. Then she stopped it. No more chest pain? Sure. But now she’s too tired to watch her favorite game shows. Not worth it.
Eileen Choudhury
November 5, 2025 AT 18:21I love how this article doesn’t just throw numbers at us - it tells stories. That 82-year-old woman in Bristol? That’s my aunt. She said the same thing: ‘I wish I’d tried this sooner.’
For so long, we treat older adults like broken machines that need fixing. But ranolazine? It doesn’t fix. It restores. It lets them live again. Gardening. Walking the dog. Hugging grandkids without fear.
This isn’t just medicine. It’s dignity.
Melissa Kummer
November 6, 2025 AT 15:03Thank you for this meticulously researched and clinically nuanced overview. As a geriatric nurse practitioner, I can attest that ranolazine is vastly underutilized due to unwarranted fear of QT prolongation. The data is unequivocal: when used appropriately, with baseline ECG and medication reconciliation, the risk-benefit ratio is overwhelmingly favorable.
Let us not allow pharmacological dogma to deprive our elderly patients of meaningful quality of life.
Pradeep Kumar
November 8, 2025 AT 06:27From India, I’ve seen this too. Elderly patients here are often told ‘just live with it’ - no one wants to add another pill. But when we start ranolazine low, monitor, and explain it simply - they light up.
One man, 76, stopped using his cane after two weeks. Said his chest didn’t ‘squeeze’ anymore. Simple. Powerful.
❤️
Matthew Kwiecinski
November 9, 2025 AT 19:37Let’s be real - ranolazine is expensive. Generic or not, it’s still $40/month. Medicare may cover it, but what about the 30% of seniors on fixed incomes who skip meds to pay for food?
This whole discussion ignores the elephant in the room: healthcare access. A drug that works is useless if no one can afford it. We’re treating symptoms while the system collapses.
Justin Vaughan
November 11, 2025 AT 05:30My dad’s cardiologist told him ranolazine was ‘for last resort.’ But after three failed trials of beta-blockers and nitrates, it was the only thing that didn’t make him feel like a zombie.
He’s on simvastatin 10mg - not 20. No issues. ECG normal. No dizziness after week one.
Don’t let fear stop you from trying. Start low. Watch. Listen to the patient. That’s all.
And yes - it takes 4-6 weeks. Patience is part of the treatment.
Andy Ruff
November 11, 2025 AT 13:15Stop glorifying this drug. It’s a Band-Aid on a bullet wound. You’re telling people to take a pill that can cause torsades because ‘the risk is low’ - but low isn’t zero. And when it happens? It’s fatal. And who pays? The family. The hospital. The system.
Why not just tell them to stop climbing stairs? Why not refer them to cardiac rehab? Why not fix the root cause instead of slapping on a chemical veneer?
This isn’t medicine. It’s corporate convenience wrapped in clinical jargon.
Manuel Gonzalez
November 12, 2025 AT 22:18Great breakdown. I especially liked the table comparing meds - clear, practical, no fluff.
One thing I’d add: don’t forget to ask about grapefruit juice. I’ve had three elderly patients on ranolazine who didn’t realize grapefruit was a problem. One ended up in the ER with dizziness. Simple fix - stop the juice.
Small things matter.
andrea navio quiros
November 13, 2025 AT 16:37the liver does the work not the kidneys so if you have bad kidneys you might still be ok but if your liver is fried then dont
also check every single med your taking even the herbal stuff
and yes it takes time
no magic
just science
and patience
Brittney Lopez
November 15, 2025 AT 04:55Thank you for writing this with such care. I’ve seen too many older patients dismissed because ‘they’re too old for new drugs.’ But this isn’t about age - it’s about quality of life.
My mom’s doctor was hesitant too. We brought this article. He changed his mind. Now she’s walking 3 miles a day.
It’s not about being young. It’s about being alive.
Alexa Apeli
November 15, 2025 AT 10:17As a caregiver for my 84-year-old mother, I want to say: thank you. This article gave me the courage to ask her cardiologist about ranolazine. We started at 500 mg. She had mild constipation for five days - then nothing. Her angina went from daily to once a week. She’s back to knitting, laughing, and even baking cookies again.
❤️ This isn’t just a drug. It’s a second chance. And I’m so grateful for clinicians who take the time to explain it right.