It’s 2025, and more Americans than ever are taking SSRIs. About 1 in 8 adults uses one - fluoxetine, sertraline, escitalopram - to manage depression, anxiety, or OCD. They work. They’re safer than older antidepressants. But here’s the quiet danger no one talks about until it’s too late: SSRI interactions can trigger serotonin syndrome, a condition that can kill you in hours.
What Exactly Is Serotonin Syndrome?
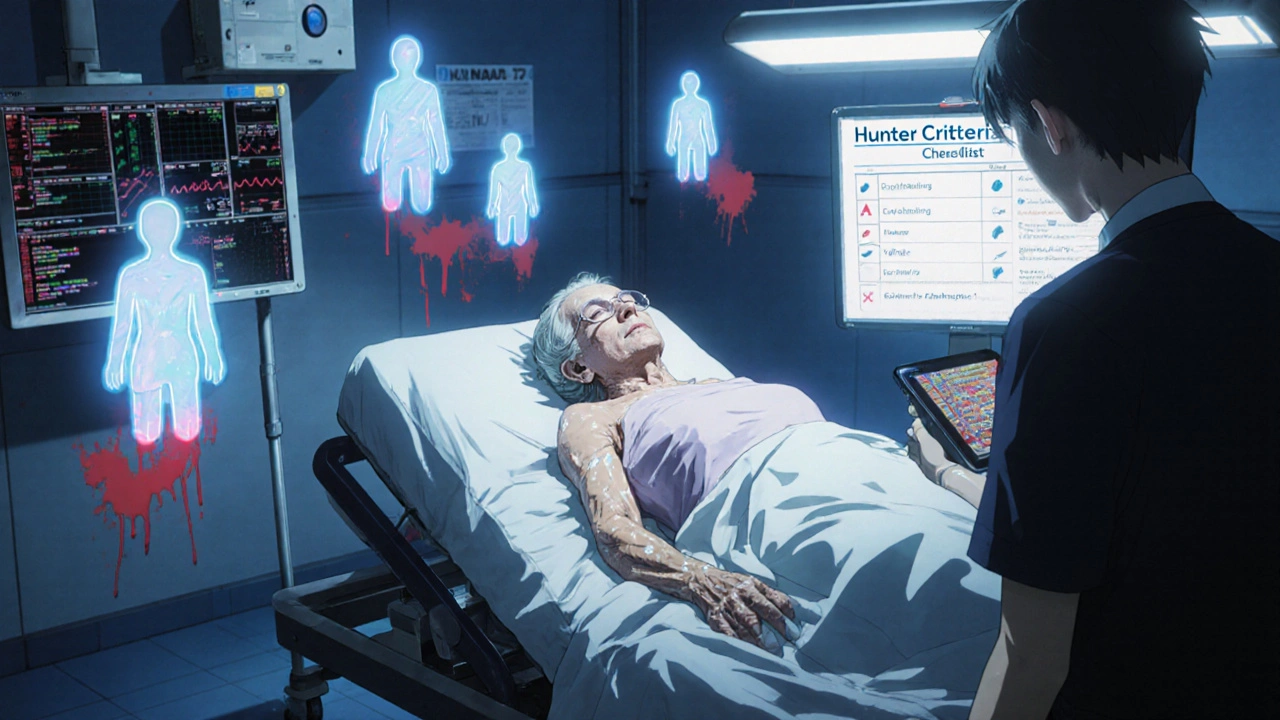
Serotonin syndrome isn’t just feeling a little jittery after coffee and your morning pill. It’s a dangerous overload of serotonin in your brain and nervous system. Think of serotonin as a chemical messenger. SSRIs block its reabsorption, so more stays active in your brain. That’s how they help mood. But if another drug adds even more serotonin - or stops your body from clearing it - things spiral fast.The symptoms aren’t subtle. You might start shivering uncontrollably. Your muscles lock up. You sweat like you’ve run a marathon in 90-degree heat. Your heart races. Your temperature spikes above 102°F. Then comes confusion, hallucinations, or seizures. In severe cases, your organs start to shut down. It’s not rare - estimates say 0.5 to 1.5 cases per 1,000 SSRI users each year. But because doctors often mistake it for infection, heatstroke, or drug withdrawal, it’s underdiagnosed. The Hunter Criteria, now the gold standard for diagnosis, look for specific signs: spontaneous clonus, inducible clonus with fever or sweating, or rigid muscles with high temperature and eye twitching.
These Are the Worst Combinations
Not all drug interactions are equal. Some are deadly. Others are risky. Here’s what you need to avoid:- MAOIs - Monoamine oxidase inhibitors like phenelzine or selegiline. Combining them with SSRIs is like lighting a match near gasoline. The FDA says it’s contraindicated. Mortality rates hit 30-50% in documented cases. Even after stopping an MAOI, you need a 2-week washout. With fluoxetine? Wait five weeks. Its metabolite sticks around for weeks.
- Linezolid - An antibiotic for tough infections. It’s an MAOI too. A 2022 JAMA study found patients over 65 on SSRIs who took linezolid had nearly 3 times the risk of serotonin syndrome. It’s not common, but when it happens, it’s bad.
- Tramadol, Dextromethorphan, Pethidine - These aren’t your regular painkillers. Tramadol (Ultram) and dextromethorphan (in cough syrups) both boost serotonin. A 2023 study showed they increase serotonin syndrome risk by 4.7 times when paired with SSRIs. One Reddit user described muscle rigidity and 104.2°F fever after taking tramadol with sertraline. He spent three days in the hospital.
- SNRIs - Venlafaxine, duloxetine. These are also antidepressants. Mixing them with SSRIs triples your risk. The FDA added a black box warning in 2006. Still, doctors prescribe them together - often because they think one isn’t working. It’s a gamble.
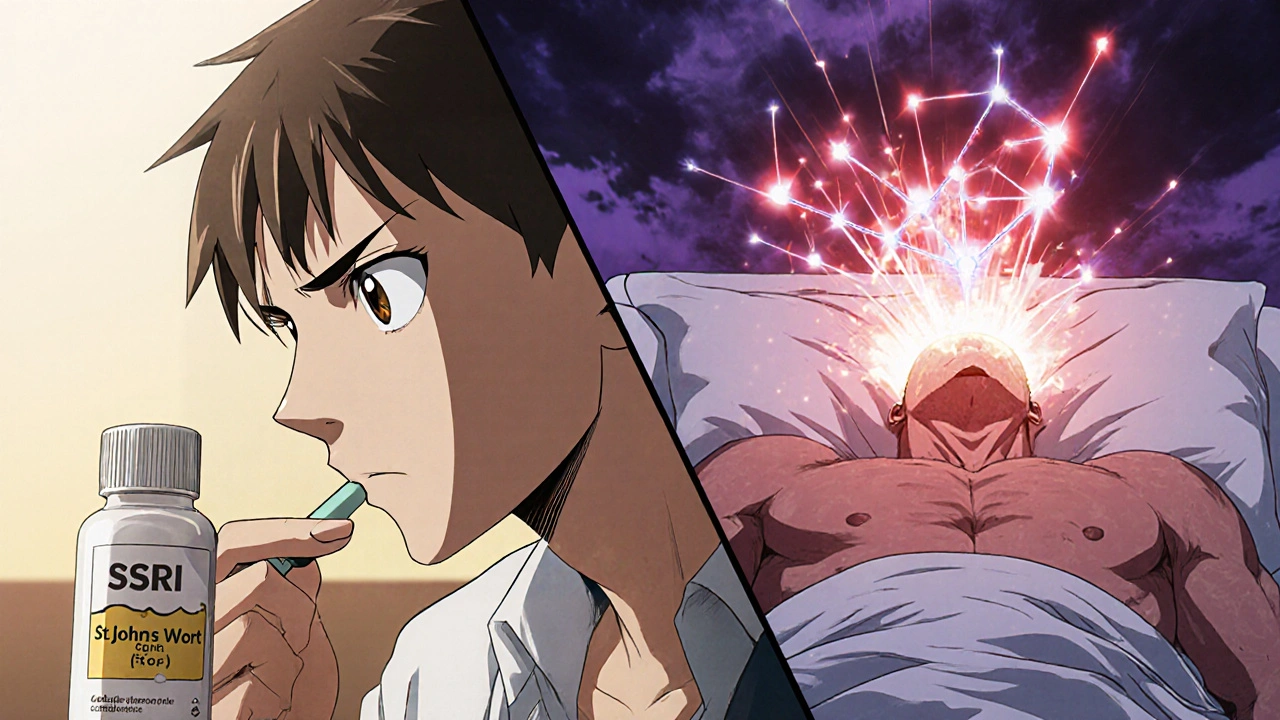
- St. John’s Wort - A popular herbal supplement for mild depression. Sounds harmless, right? Wrong. It’s a serotonin booster. Multiple users on Drugs.com reported shivering and confusion within days of combining it with Prozac. The ER called it early serotonin syndrome.
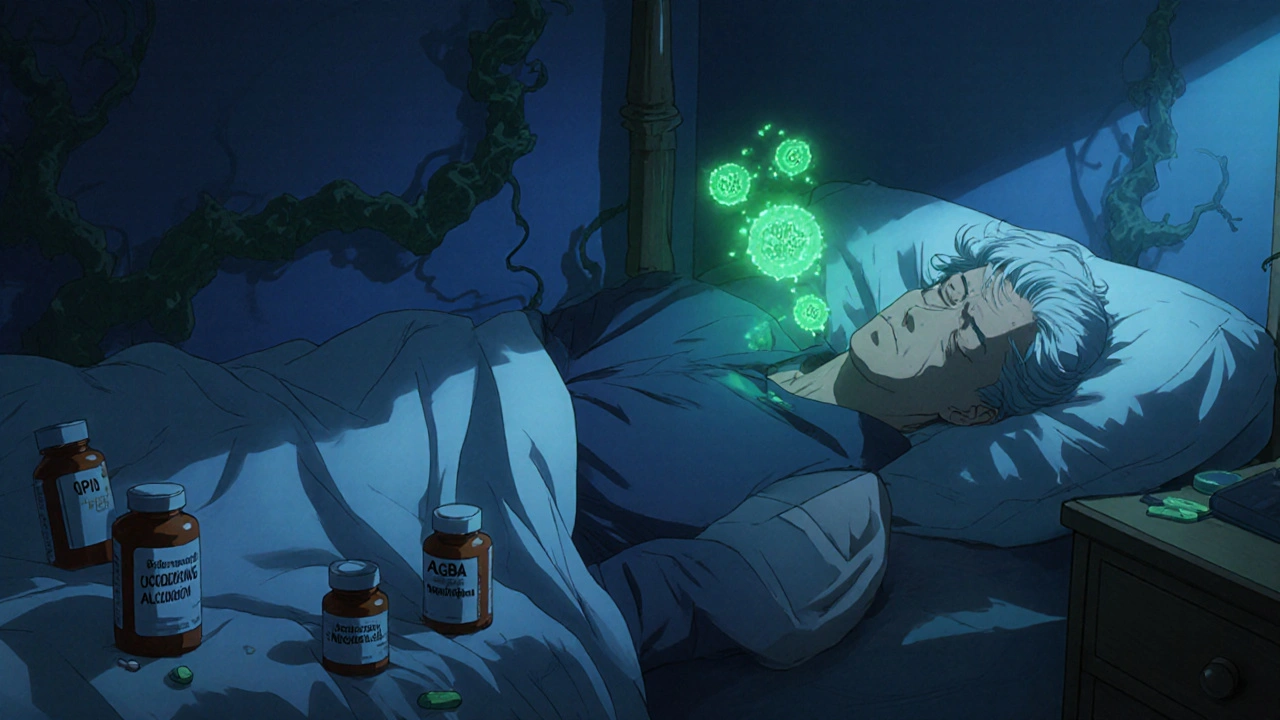
Low-risk opioids like morphine, codeine, and oxycodone? Generally safe. But methadone and fentanyl? Medium risk. They’re not off-limits, but you need close monitoring.
Why Are We Seeing More Cases Now?
It’s not just more people on SSRIs. It’s polypharmacy. People are on more drugs than ever. A 2021 JAMA editorial pointed out that 22% of Americans over 65 take five or more medications daily. Many don’t tell their doctor about supplements. Others get prescriptions from different specialists who don’t talk to each other.Take the example of an elderly woman with chronic pain and depression. Her primary care doctor prescribes sertraline. Her pain specialist prescribes tramadol for her back. Her pharmacist doesn’t flag it. She starts feeling restless, sweaty, and shaky. She thinks it’s just aging. By the time she gets to the ER, she’s in full serotonin syndrome. Her temperature is 105°F. Her kidneys are failing. She spends a week in ICU. The bill? Around $29,000 - the average cost per hospitalization.
Even more concerning: a 2023 FDA analysis found that 68% of serotonin syndrome reports between 2018 and 2022 involved drug combinations. That’s not accidents. That’s systemic.
Who’s at Highest Risk?
You might think it’s just older adults. But it’s not that simple.- People over 65 - Their liver and kidneys don’t clear drugs as fast. They’re more likely to be on multiple meds. 21.5% of Americans over 60 take SSRIs. 18.3% take opioids. That’s a dangerous overlap.
- Genetic slow metabolizers - About 7% of people have a CYP2D6 gene variant that makes them process tramadol poorly. Combine that with an SSRI? Their risk jumps 2.4 times. This isn’t theoretical. It’s measurable.
- People who self-medicate - Taking St. John’s wort, 5-HTP, or tryptophan with SSRIs is a common mistake. Online forums are full of stories like: “I took it for a week and felt like I was having a nervous breakdown.”
- Those switching antidepressants - Jumping from one SSRI to another without a washout period is a major cause. Fluoxetine’s long half-life makes this especially dangerous.
What Should You Do?
You don’t have to stop your SSRI. But you need to be smart.- Know your meds - Make a list. Include every pill, patch, supplement, and cough syrup. Bring it to every appointment. Even “natural” products can be dangerous.
- Ask your doctor - Before starting anything new, ask: “Could this interact with my antidepressant?” Don’t assume it’s safe because it’s OTC.
- Watch for the 5 S’s - As the Cleveland Clinic advises: Shivering, Sweating, Stiffness, Seizures (rare), and Sudden confusion. If you notice two or more, go to the ER. Don’t wait.
- Use a pharmacist - Pharmacists are trained to catch these interactions. Ask them to review your full list every time you get a new prescription. A 2023 study showed pharmacist-led reviews cut serotonin syndrome events by 47% in Medicare patients.
- Don’t rush switches - If your doctor wants to switch SSRIs, ask about washout periods. Fluoxetine? Five weeks. Others? At least two weeks.
What’s Changing?
The system is waking up. In 2024, the FDA mandated that all electronic prescribing systems must now show mandatory alerts for high-risk combinations - like SSRI + tramadol or SSRI + linezolid. Epic Systems already reduced risky co-prescriptions by 32% across 200 hospitals after adding these alerts.There’s even a new blood test in the works. SerotoninQuant, currently in phase 3 trials at Mayo Clinic, could give doctors an objective way to diagnose serotonin syndrome by 2026. Right now, diagnosis is based on symptoms - which can be mistaken for other things. A lab test would change everything.
But until then, the rules are simple: know your drugs. Don’t mix. Ask questions. If you feel off - really off - don’t ignore it.
Can I take ibuprofen with an SSRI?
Yes, ibuprofen is generally safe with SSRIs. It doesn’t affect serotonin levels. But both can increase your risk of stomach bleeding, especially if you’re older or take them long-term. Talk to your doctor if you’re using ibuprofen regularly.
Is serotonin syndrome always obvious?
No. Mild cases can look like anxiety, the flu, or side effects of a new medication. You might just feel restless, sweaty, or have a slight tremor. That’s why many cases go undiagnosed. If symptoms get worse - especially if you develop high fever, muscle rigidity, or confusion - treat it as an emergency.
Can I stop my SSRI if I’m worried about interactions?
Never stop an SSRI cold turkey. It can cause withdrawal symptoms like dizziness, nausea, brain zaps, and worsened depression. If you’re concerned about interactions, talk to your doctor. They can help you switch safely with the right washout period.
Are all SSRIs equally risky?
No. Paroxetine has the strongest serotonin reuptake inhibition (95%), making it the most likely to cause problems in combinations. Fluoxetine lasts the longest, so interactions can pop up weeks after stopping it. Sertraline and escitalopram are often preferred because they’re effective with lower interaction risk.
What should I do if I think I have serotonin syndrome?
Go to the ER immediately. Tell them you’re on an SSRI and recently started another medication. Don’t wait. Serotonin syndrome can progress rapidly. Treatment includes stopping the offending drugs, IV fluids, and sometimes medications like cyproheptadine to block serotonin. Time matters.







Joseph Townsend
November 18, 2025 AT 02:39Bro. I took tramadol with sertraline for my back pain last year. Thought I was just having a bad anxiety day. Then I started shaking like a leaf in a hurricane, sweating buckets, and my muscles turned to concrete. ER said serotonin syndrome. I spent three days hooked up to IVs while they tried to un-fry my brain. Now I carry a card in my wallet that says 'DO NOT GIVE ME TRAMADOL OR DXM'. This isn't hype. This is survival.
And don't even get me started on St. John’s Wort. That 'natural' stuff is basically legal MDMA for your serotonin receptors. People think herbal = safe. Nah. It's just unregulated poison with a yoga vibe.
Bill Machi
November 18, 2025 AT 05:06Another case of American medical incompetence. We let anyone walk into a pharmacy and buy supplements that can kill them, while our doctors are too busy chasing insurance reimbursements to actually read a drug interaction chart. This isn’t a public health issue - it’s a failure of governance. We need mandatory pharmacology certification for every prescriber, not just another FDA alert that no one reads.
Elia DOnald Maluleke
November 20, 2025 AT 02:11One must contemplate the metaphysical weight of neurochemical regulation in a society that commodifies mental well-being. We have turned the sacred dance of neurotransmitters into a pharmacological spreadsheet - a ledger of dosage and risk, devoid of the soul’s quiet equilibrium. The SSRI is not merely a molecule; it is a symbol of our alienation from embodied healing.
And yet - we are told to ‘ask your doctor’ - as if the physician, burdened by 20 patients per hour and an EHR that crashes every third click, can possibly possess the moral clarity to navigate this labyrinth.
Perhaps the cure is not more alerts - but less medicine. More silence. More tea. More listening.
satya pradeep
November 21, 2025 AT 04:31Yo, I’m a pharmacist in Bangalore and we see this ALL the time. Indians love to mix ayurvedic stuff like ashwagandha, brahmi, or even turmeric with SSRIs because ‘it’s natural’. But guess what? Turmeric inhibits CYP enzymes. Ashwagandha boosts serotonin. You think you’re being holistic - you’re just setting yourself up for a trip to ICU.
Also, don’t forget that tramadol is sold OTC in half the countries in Asia. No script. No warning. Just a guy behind the counter handing you a box like it’s candy. This isn’t just a US problem. It’s global.
Prem Hungry
November 21, 2025 AT 06:58Hey, I know this feels scary - but please don’t panic. SSRIs are life-changing for so many people. The key isn’t to avoid them - it’s to be informed. Talk to your pharmacist. Keep a meds list. Use apps like Medscape or Epocrates to check interactions before you take anything new. I’ve helped dozens of patients avoid disasters just by asking one simple question: ‘What else are you taking?’
You’re not alone. We’ve got your back. Stay smart, not scared.
Leslie Douglas-Churchwell
November 22, 2025 AT 02:32OF COURSE the FDA only acted after 68% of cases were documented. Classic. They’re owned by Big Pharma. Why warn people when they can just sell you a new drug to ‘fix’ the side effects of the last one? And don’t get me started on ‘SerotoninQuant’ - it’s just another $$$ lab test so they can charge you $1,200 for a blood draw that confirms what your body’s been screaming for weeks.
Also - who approved St. John’s Wort? Was it the same people who said vaping was safe? 😏
PS: I’ve been on Lexapro for 7 years. I take NO supplements. No ibuprofen. No cough syrup. No ‘wellness’ tea. I’m one of the few who actually READ the warnings. 🙃
shubham seth
November 23, 2025 AT 03:30Let’s be real - the real villain here isn’t tramadol or MAOIs. It’s the fact that psychiatrists are glorified pill-pushers with 15-minute consults. You walk in saying ‘I’m depressed’ and they hand you sertraline like it’s a coupon for happiness. No therapy. No lifestyle review. No ‘what else are you taking?’
And now we’re blaming the patient for mixing meds? Nah. We’re blaming the system that turned mental health into a fast-food drive-thru. You don’t fix depression with a pill and a checklist. You fix it with time, support, and a damn good therapist - not a 30-second interaction with a PA who’s on her 8th script of the hour.
Kathryn Ware
November 24, 2025 AT 10:41I’m a nurse in a psych unit, and I’ve seen serotonin syndrome up close. It’s terrifying. One patient went from ‘just feeling weird’ to seizing in 4 hours. We had to intubate him. He’s fine now - but he didn’t tell his doctor he started taking 5-HTP because ‘it helped his friend’. That’s the thing - people don’t think it’s a big deal because it’s ‘just a supplement’. But your body doesn’t care if it’s synthetic or ‘natural’. It just reacts.
PLEASE - if you’re on an SSRI and thinking about trying anything new - even CBD or melatonin - ask your pharmacist first. They’re the unsung heroes who actually catch these things. I’ve seen them prevent 3 near-misses this month alone. 💙
kora ortiz
November 26, 2025 AT 00:33Knowledge is power. Period. If you’re on an SSRI, you owe it to yourself to know what you’re mixing it with. No excuses. No ‘I forgot’. No ‘it’s just a little cough syrup’. This isn’t about fear - it’s about responsibility. You wouldn’t drive a car without checking the brakes. Don’t treat your brain like it’s a free-for-all.
Print this. Save it. Show it to your doctor. Your life depends on it. 💪
Jeremy Hernandez
November 26, 2025 AT 08:21So let me get this straight - the same people who scream ‘vaxx mandate!’ are now okay with letting strangers walk into CVS and buy serotonin-boosting herbs like they’re buying gum? Classic American hypocrisy.
And don’t even get me started on ‘washout periods’. Who the hell remembers to wait five weeks after stopping fluoxetine? You think your cousin Bob’s 78-year-old grandma with 12 meds is keeping a spreadsheet? Nah. She’s taking her pills when the pillbox beeps. This system is a death trap.
And the FDA’s ‘mandatory alerts’? That’s like putting a sticker on a grenade saying ‘DO NOT PULL’. It doesn’t change the fact that the damn thing’s still in the room.
Tarryne Rolle
November 27, 2025 AT 06:12Isn’t it ironic that we’ve created a society where we outsource our emotional regulation to pharmaceuticals - then blame the drugs when they malfunction? We’ve turned the human nervous system into a lab experiment, and now we’re shocked when the variables go haywire.
Perhaps serotonin syndrome isn’t a medical condition - it’s a symptom of our collective spiritual dissonance. We seek chemical peace while ignoring the quiet screams of our own unprocessed grief.
But of course - that’s too metaphysical for a 15-minute consult.
Kyle Swatt
November 27, 2025 AT 17:08I was on Lexapro for years. Never had an issue. Then I started taking melatonin for sleep. Didn’t think twice. One night I woke up drenched, heart racing, muscles locked. Thought I was having a heart attack. Turned out to be mild serotonin syndrome.
Turns out melatonin can inhibit serotonin reuptake too - not as strong as tramadol, but enough to tip the scales if you’re sensitive.
Now I tell everyone: if it affects your mood, sleep, or energy - it might affect your serotonin. Even ‘harmless’ stuff. Your body’s not a vending machine. It’s a living system. Treat it like one.
Deb McLachlin
November 27, 2025 AT 17:49Thank you for this comprehensive and clinically grounded overview. The integration of epidemiological data, pharmacokinetic considerations, and practical clinical guidance is exemplary. I am particularly impressed by the emphasis on pharmacist-led interventions, which aligns with recent literature in the Journal of Clinical Pharmacy and Therapeutics (2023).
One point of further inquiry: Have any studies examined the impact of polypharmacy alerts on non-Medicare populations, particularly younger adults who are increasingly prescribed SSRIs for anxiety disorders? The demographic shift toward early-onset depression may render current alert systems insufficient if they are primarily calibrated for elderly polypharmacy profiles.
saurabh lamba
November 29, 2025 AT 08:48lol. So now we’re scared of cough syrup? Next they’ll ban coffee because it has caffeine. People are dying from SSRIs? Bro. People die from falling out of bed. This is just fearmongering wrapped in a JAMA paper.
Also, ‘St. John’s Wort is dangerous’? Yeah, so is sunlight. Everything’s dangerous if you’re dumb enough to mix it. Grow up.
Joseph Townsend
November 29, 2025 AT 15:25Bro. I took tramadol with sertraline for my back pain last year. Thought I was just having a bad anxiety day. Then I started shaking like a leaf in a hurricane, sweating buckets, and my muscles turned to concrete. ER said serotonin syndrome. I spent three days hooked up to IVs while they tried to un-fry my brain. Now I carry a card in my wallet that says 'DO NOT GIVE ME TRAMADOL OR DXM'. This isn't hype. This is survival.
And don't even get me started on St. John’s Wort. That 'natural' stuff is basically legal MDMA for your serotonin receptors. People think herbal = safe. Nah. It's just unregulated poison with a yoga vibe.